Severe traumas are an important cause of morbimortality, being blunt traumas, and traffic accidents the most common etiologies in our setting.1 Even though the non-surgical management of these patients is widely indexed in medical literature, today there is still controversy on the indications of total-body CT scans, and, actually, on some occasions, it is determinant to establish surgical management.
After obtaining the patient's informed consent, we hereby present the case of one multi-trauma individual who was in serious condition after a motorcycle crash, with non-surgical management of the patient's thoracoabdominal lesions and satisfactory progression.
Male; 32 years old; no significant clinical history; the driver was wearing a helmet and suffered from high-energy trauma due to motorcycle crash with further ejection from the vehicle. After initial assessment following the ATLS principles and confirmation of airway patency; good ventilation; hemodynamic stability; and absence of severe CET, the patient was transferred to a trauma reference center.
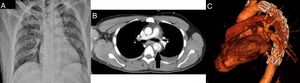
We conducted the initial assessment upon arrival: patient alert, oriented, and speaking in a coherent manner. Good airway patency with cervical protection; spontaneous respiration rate at 18bpm; symmetrical respiratory movement pattern; absence of external signs of cervical and thoracic lesions; and normal percussion, and lung auscultation. The patient remains hemodynamically normal at 80bpm; normothermic; with adequate pulse; capillary refill; and cutaneous-mucosal coloration. The possible bleeding focus may come from one right, displaced, humeral, diaphisary fracture that is immobilized after the administration of anti-tetanus prophylaxis. At abdominal level, there is diffuse pain at palpation, without any signs of peritonism, or pain in the pelvis. The patient shows macroscopic hematuria with spontaneous micturition, but without any visible perineal alterations, which is why we did not proceed with the catheterization of the gallbladder at that time. The X-rays from the chest (Fig. 1A), and the pelvis look normal.
The neurological assessment confirmed the presence of symmetrical reactive pupils; a score of 15 in the Glasgow Coma Scale; and no signs of lateralization or spine injury.
The secondary survey analyzed the skin surface, and cleaned and sutured wounds in the lower lip region; jaw; right forearm; and right ankle.
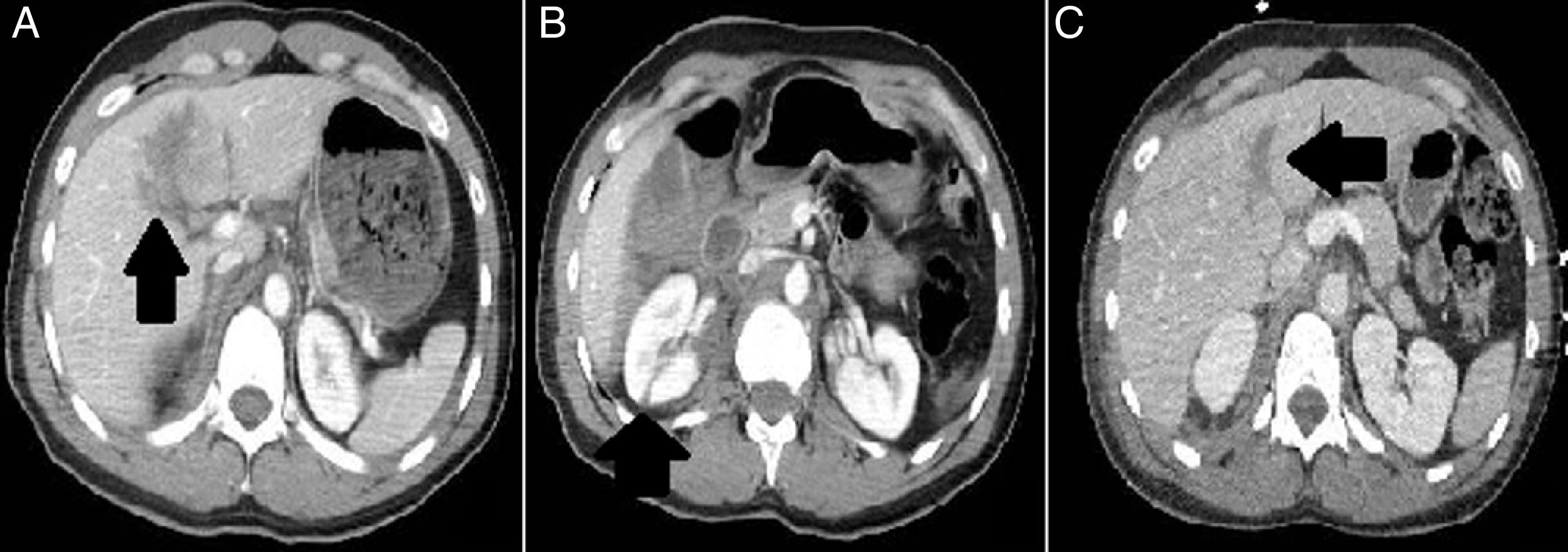
In this context, we conducted one total-body CT scan that found multiple lesions: rupture of the descending thoracic aorta type IV with pseudoaneurysm; periaortic hematoma; small left hemithorax (Fig. 1B); posterior splenic lacerations grade II; hepatic lacerations grade II in segment V with signs of active bleeding (Fig. 2A); right posterior–superior renal laceration grade IV (Fig. 2B); and gallbladder microperforation grade I. There was no damage to the axial skeleton or the pelvic girdle, but there were left and sternal nondisplaced mandibular fractures.
(A) The arrow shows one hypodense area in the hepatic segment V that is consistent with the hepatic lesion reported. (B) The arrow shows one right renal lesion at posterior-superior level. (C) The control CT scan conducted at day 8 confirms that the hepatic lesion has reduced its size and shape.
The urgent percutaneous placement of one aortic endoprosthesis (Fig. 1C) followed by hepatic, renal, and splenic selective arteriography is suggested, but in the absence of active bleeding, a decision is made to implement conservative therapy of the abdominal lesions. The gallbladder lesion is managed through the gallbladder catheter that is kept during the whole hospital stay. Also, the surgery of the mandibular fracture is ruled out due to the lack of lateral deviation; pain; or opening/closing alterations.
The patient was then transferred to the ICU for monitoring and fluid therapy. Left endothoracic drainage was placed at a volume of 500 cc of hematic fluid for 24h to be removed after 72h and once the resolution was confirmed radiologically. The patient was extubated at day 4, and at day 5 both the surgical internal fixation of the humeral fracture, and the escharotomy of the right ankle lesion were conducted, resulting in a cutaneous defect of approximately 10cm with exposure of the superficial peroneal nerve.
At day 8, one control CT scan is conducted that confirms the good progression of the aortic, hepatic, and renal lesions (Fig. 2C), and the disappearance of the splenic and gallbladder lesions.
The patient was then taken to his room and discharged from the hospital 10 days later. He required one graft at the back side of his right foot–procedure that was conducted outpatiently, followed by one kinesiotherapy rehabilitation program, and infiltration of the posterior tibial nerve.
At present, 30 months after being discharged from the hospital, the patient shows no significant sequelae.
In our setting, we use different anatomical scoring systems, among them the Injury Severity Score (ISS), or the Anatomic Profile (AP) that, in our patient, scored 45 and 15.85 points, respectively. In order to calculate these scoring systems, one total-body CT scan is required,2 although recent publications show that the systematic use of such systems does not reduce mortality compared to the use of conventional imaging modalities.3 However, the identification of possible subgroups that could benefit from the use of the aforementioned scoring systems is still pending. We believe that in the case of a severe hemodynamically stable multi-trauma with unfavorable kinematics of trauma such as the case of a motorcycle crash at a speed of more than 32km/h with driver ejected,4,5 conducting one total-body CT scan would certainly benefit and guide the therapeutic plan.6 Upon hospital arrival, both the examination of the patient and his chest X-rays were normal, so had the total-body CT scan not been conducted, the aortic lesion would have never been found.
The finding of minimum aortic lesions on CT scans can make us opt for medical management. In more advanced lesions in patients selected with no risk of imminent free aortic rupture, the endovascular therapy is feasible,7 whose optimal time will depend on concomitant lesions and the resources available at the medical center. In the case of pseudoaneurysmatic lesions like our patient's lesion with damage to less than 50 per cent of the aortic circumference, an early repair may not be necessary in an attempt to improve the patient's condition and plan endovascular control with higher chances of success.8
ICU admissions are essential if we want to optimize the patient's hemodynamic situation; medical management during and after the procedure; and, also, if we want to monitor serious concomitant lesions.9 The prognosis has improved in these selected cases, especially in younger patients, being the radiological confirmation useful for their resolution.
In sum, although today there is still controversy on which multi-trauma patients should be eligible for one total-body CT scan, we believe that when in the presence of one multi-trauma hemodynamically stable patient with unfavorable kinematics of trauma, conducting one total-body CT scan is advisable, because it can avoid misdiagnoses of important lesions, and is essential to plan minimally invasive management.
AuthorsMs. Sandra Dios, and Ms. Virginia Durán conducted the reference search and shaped this manuscript.
Mr. Felipe Pareja, and Ms. Virginia Durán suggested the case and provided ideas on study design and concept.
Mr. Felipe Pareja, Ms. Cristobalina Martín, Ms. Mercedes Rubio, and Mr. Francisco Javier Padillo conducted the paper critical review and provided relevant know-how.
All authors gave their approval to the final version of this paper.
Please cite this article as: Dios-Barbeito S, Durán-Muñoz-Cruzado V, Martín-García C, Rubio-Manzanares-Dorado M, Padillo-Ruiz FJ, Pareja-Ciuró F. ¿Qué pacientes politraumatizados graves se benefician de la realización de un total-body CT? Med Intensiva. 2018;42:129–131.