To evaluate the number and characteristics of potential organ donors among cardiocirculatory death cases.
Design and settingA retrospective observational study was made of individuals between 15 and 65 years of age who died in the period 2006–2014 in Elche University General Hospital (Alicante, Spain).
InterventionA univariate analysis and binary logistic regression predictive model were performed to discriminate factors related to donation contraindication.
Variables of interestIdentification of patients with donation contraindication.
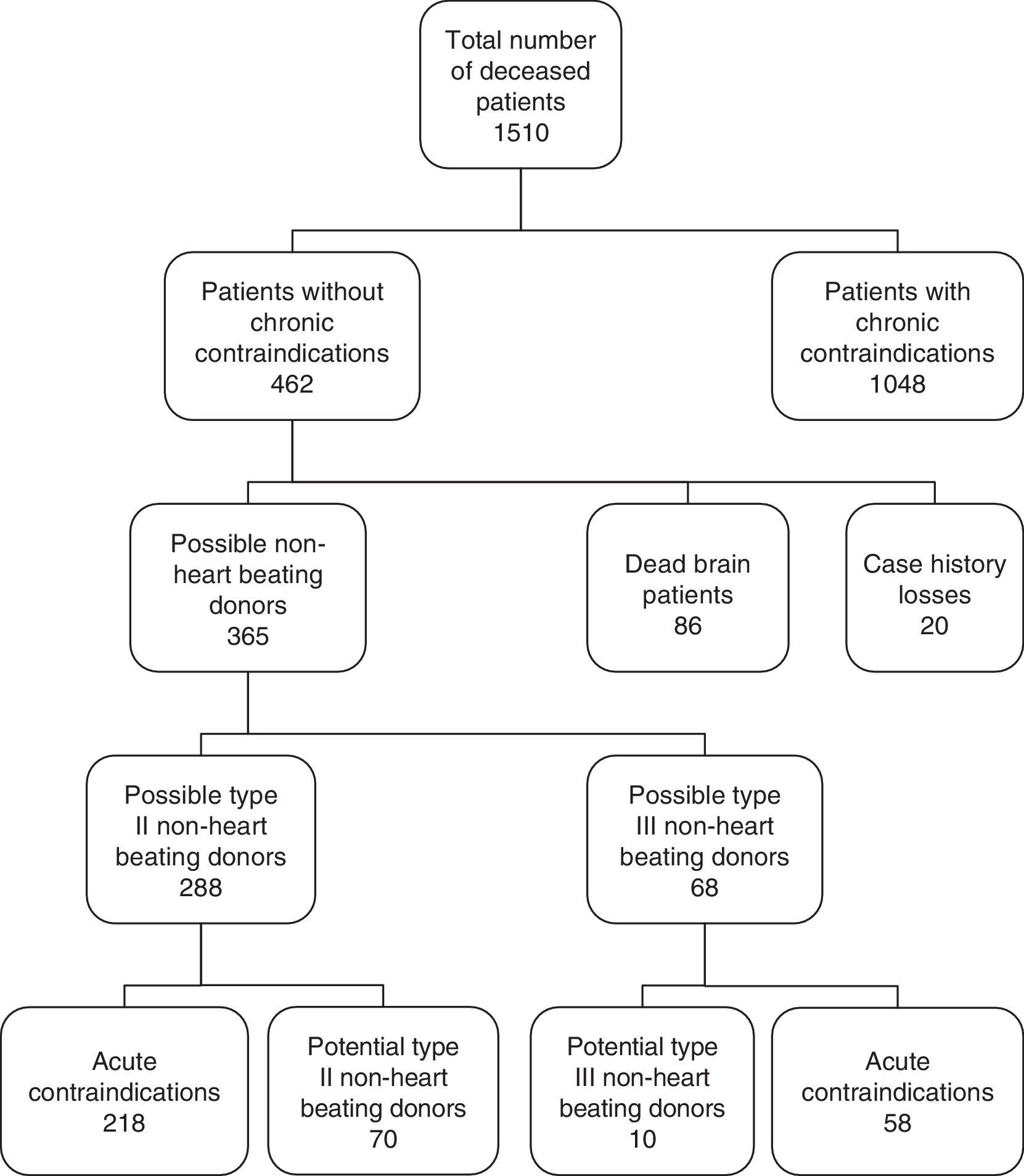
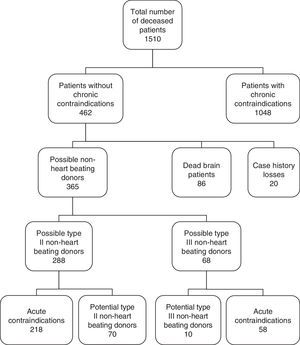
ResultsOf the 1510 patients who died in the mentioned period, 1048 were excluded due to the application of exclusion criteria; 86 due to evolution toward brain death; and 20 due to losses. A total of 356 patients were analyzed, divided into two groups: 288 in non-heart beating donation II and 68 in non-heart beating donation III. Seventy patients were found to be potential non-heart beating donation II and 10 were found to be potential non-heart beating donation III, which could increase donation activity by 8–9 donors a year. The patients died in the ICU, Resuscitation, Emergency Care, Internal Medicine, Digestive Diseases and Neurology. The following protective factors against organ donation contraindication were identified: death in Emergency Care, cardiorespiratory arrest before or during admission, and heart, respiratory and neurological disease as the cause of admission. Death in Internal Medicine was associated to an increased risk of donation contraindication.
ConclusionsImplementing a non-heart beating donation protocol in our hospital could increase the donation potential by 8–9 donors a year.
Estimar el número y las características de potenciales donantes de órganos de personas fallecidas por muerte cardiocirculatoria.
Diseño y ámbitoEstudio retrospectivo observacional de los fallecidos entre 15-65 años entre el 2006 y 2014 en el Hospital General Universitario de Elche.
IntervenciónRealización de análisis univariante y modelo predictivo de regresión logística binaria para discriminar los factores relacionados con la contraindicación para la donación.
Variables de interésIdentificar los pacientes con contraindicaciones para la donación.
ResultadosDe los 1.510 pacientes fallecidos se excluyeron 1.048 por criterios crónicos de exclusión, 86 por evolucionar a muerte encefálica y 20 por pérdidas. Se analizaron 356 pacientes en 2 grupos: 288 en donación en asistolia ii y 68 en donación en asistolia iii. Resultaron potenciales donantes en asistolia ii 70 pacientes y 10 donantes en asistolia iii, lo que podría incrementar la actividad de donación en 8-9 donantes/año. Los pacientes fallecieron en: UCI, reanimación, urgencias, medicina interna, digestivo y neurología. Resultaron variables protectoras frente a contraindicación para la donación: fallecer en urgencias, parada cardiorrespiratoria previa o durante el ingreso, la enfermedad cardiológica, respiratoria y neurológica como causa de ingreso. Fallecer en el servicio de medicina interna se asoció a un mayor riesgo de contraindicaciones para la donación.
ConclusionesPoner en marcha un protocolo de donación en asistolia en nuestro hospital podría incrementar el potencial de donación en unos 8-9 donantes/año.
The decrease in possible brain dead donors resulting from traffic accidents observed in recent years, together with the gradual increase in indications of organ transplantation, have led to a progressive increment in the number of patients requiring organ transplantation and who are on the waiting list. This requires optimization of all the available resources with a view to increasing the number of donations, including donation after cardiocirculatory death—a practice already widely adopted at international level for decades.
Donation after cardiocirculatory death (DCD) or non-heart beating donation (NHBD), allowing the harvesting of tissues and organs (kidneys, liver, lungs, etc.), is an important potential source of organs, along with brain dead donation (DBD)—which to date has represented the main source of donations in our setting, and which likewise allows the harvesting of tissues and organs (kidneys, liver, pancreas, heart, lungs, etc.).
With the purpose of offering an adequate framework for the development of multiple NHBD programs in our country, the Spanish National Organization of Transplants (Organización Nacional de Trasplantes [ONT]) developed a consensus document for NHBD1 in 2012, with the opportune and necessary ethical and legal considerations. Cardiocirculatory death is defined as the irreversible cessation of cardiac function, manifesting as the absence of a heart beat demonstrated by the absence of a central pulse or as established from the electrocardiogram, and the absence of spontaneous breathing - both situations being witnessed for a period of no less than 5min.2,3 Emphasis is placed on the principle that the death of an individual is not determined by irreversible loss of cardiac function but by the irreversible loss of circulatory (and respiratory) function.
To classify donors of this kind, the ONT recommends the system proposed by the Maastricht Conference of 1995,4 with the modification introduced on occasion of the last National Consensus meeting held in Madrid in 20111 (Maastricht, modified), in view of the importance of establishing whether cardiac arrest (CA) occurs in the out- or in-hospital setting. Type I corresponds to patients suffering sudden death (of traumatic origin or otherwise) occurring out of hospital, and which for obvious reasons are not amenable to resuscitation. Type II corresponds to patients that suffer CA and are subjected to resuscitation maneuvering that proves unsuccessful. These cases in turn are subclassified into Type IIa (out-hospital CA) and Type IIB (in-hospital CA). Type III corresponds to patients in which CA is expected in view of the seriousness of the clinical condition, and in which the limitation of life support treatment (LLST) is decided in agreement with the family or the pre-stated will of the patient. It is important to distinguish LLST from donation as two independent processes: in effect, the decision to apply LLST is first made in agreement with the family and/or relatives and the medical team, and once this decision has been made, the possibility of donation after death is commented with the family or patient. Lastly, Type IV corresponds to patients that suffer CA during or after the diagnosis of brain death. Donation can also be classified as either controlled or non-controlled, in reference to the likeliness of CA, and which can lead to the decision to adopt earlier preservation measures in a “controlled” manner—with the consequent shortening of the ischemia times. Types I and II are regarded as “non-controlled” donors, while types III and IV are regarded as “controlled” donors.
In Spain, the drafting of the Spanish consensus document on organ harvesting from non-heart beating donors, published in 1995,5 and the legal reform embodied in Spanish Royal Decree 2070/1999,3 made it possible for certain hospital centers to develop type II non-heart beating donation programs, with increasingly better outcomes.6–10 Type III non-heart beating donation has been the procedure routinely used in Europe, the United States, Canada and Australia.11,12 Very good outcomes have been recorded in terms of both survival of the graft and of the patient receiving the organ, in the case of kidney,13 liver14 and lung transplants.15
In order to clarify the terminology referred to donors in the course of the donation process,16,17 “possible donors” are defined as patients with serious brain damage or with circulatory failure and no apparent medical contraindications to organ donation. In turn, “potential donors” are patients in which circulatory function has ceased and in which resuscitation maneuvers will not be started or continued, or individuals in which the cessation of circulatory function is expected in a period of time allowing the harvesting of organs for transplantation. “Eligible donors” are those without medical contraindications to donation, in which death has been evidenced by the irreversible cessation of circulatory function as established by current legislation, and in a period of time allowing the harvesting of organs for transplantation. “Real donors” are eligible donors in which consent to donation has been obtained and where a surgical incision has been made for the harvesting of organs for transplantation, or in which at least one organ has been harvested for transplantation. Lastly, “used donors” are real donors from which at least one organ has been transplanted.
Many patients that die in hospital and which could be candidates for NHBD are lost in practice. Knowing the number of potential NHBD cases we could detect, as well as their characteristics and origin, may provide an orientation as to how to implement an NHBD program and which hospital Departments should be targeted in this context. On the other hand, we could explore whether it is possible to identify the subgroups of patients that are most likely to be potential non-heart beating donors, and to identify the most frequent contraindications to NHBD that might be avoided by adopting certain protocols in the hospital (such as LLST or sepsis protocols). The present study was therefore carried out to: determine the number of potential donors among people suffering cardiocirculatory death between 2006 and 2014 in Elche University General Hospital (Alicante, Spain) (Health Department 20 of the Valencian Community); identify the Departments of origin of the potential donors; analyze the potential donors according to category (type II and type III) and organ viability; and study those characteristics related to the contraindications that result in an increased loss of potential donors.
Patients and methodsA cross-sectional retrospective study was made of all adult cardiocirculatory deaths recorded between 2006 and 2014 in Elche University General Hospital. The NHBD project was approved by the Ethics Committee of our hospital for the development of the full NHBD program. The present study constitutes a preamble to implementation of the program.
We first generated a list of all the deceased patients from the mortality records of our hospital corresponding to the period 2006–2014. Using the electronic case history database of our hospital, which includes the codes of all diagnoses referred to all diseases in International Classification of Diseases – Ninth Edition (ICD-9) format, we selected those patients between 15 and 65 years of age that did not meet the general exclusion criteria referred to donor candidates, based on the recommendations of the ONT18,19 (document on infections and tumors of the ONT specifying those chronic infections and tumors that discard possible donation) and documented in the electronic case history (Fig. 1). The acute infections contraindicating donation were subsequently reviewed on examining the case history in paper format, in order to determine whether the acute infection was active at the time of death or was a disease antecedent—i.e., a condition of the past and which at the time of death would not have constituted a contraindication to donation. We also excluded those patients that died according to neurological criteria (brain death), and those cases in which access to the full clinical information did not prove possible. A detailed review was made of the case histories of all the selected patients, which were divided into two groups: type II possible non-heart beating donors (NHBDII)(those dying of unexpected CA), or type III possible non-heart beating donors (NHBDIII)(those in which LLST was considered before death). We discarded those cases meeting other general exclusion criteria (acute infection, organ failure, sepsis, etc., at the time of death) and those meeting some specific exclusion criterion for each type of donation: in the case of NHBDII this would be CA not witnessed, while in the case of NHBDIII it would correspond to a time of over 120min between LLST and CA. We reviewed the type of LLST (withdrawal of treatments, no new life support treatment measures, no admission to the Intensive Care Unit [ICU], instructions against resuscitation, etc.). It should be noted that no type III NHBD program had been implemented up to that time; as a result, it was to be expected that patients with LLST would not have undergone any resuscitation maneuvering. This in turn would imply a lack of information referred to parameters such as resuscitation time, critical ischemia time, etc., since maneuvers causing discomfort (e.g., the recording of vital signs) are avoided in patients of this kind.
Lastly, we assessed pre-CA viability of the organs of the potential donors (lungs, kidneys and liver). The contraindications to kidney donation were the presence of chronic renal failure (chronic serum creatinine or urea elevation, with creatinine clearance <60ml/min according to the Cockroft formula), the presence of proteinuria in the nephrotic range (>0.5g/24h), and primary kidney disease (diabetic nephropathy, hypertensive disease, polycystosis, etc.). In the case of the liver, we considered the following contraindications: previous liver disease (cirrhosis, steatosis >40%, hepatic polycystosis, chronic hepatitis), non-controlled intraabdominal infection, intoxications with liver involvement, and liver rupture or trauma. Lastly, the following contraindications were considered in relation to lung donation: age over 55 years, chronic lung disease and trauma, a history of chest surgery, presence of lung infiltrates on chest X-rays, bronchoaspiration and/or purulent secretions.
Qualitative variables were expressed as proportions and quantitative variables as the median and percentiles (P25 and P75). The comparison of quantitative variables was carried out using the Student t-test, while qualitative variables were compared using the chi-squared test. The identification of factors associated to greater or lesser contraindication to donation in general was based on the generation of a binary logistic regression predictive model. Statistical significance was considered for P<0.05. The SPSS version 19 statistical package was used throughout.
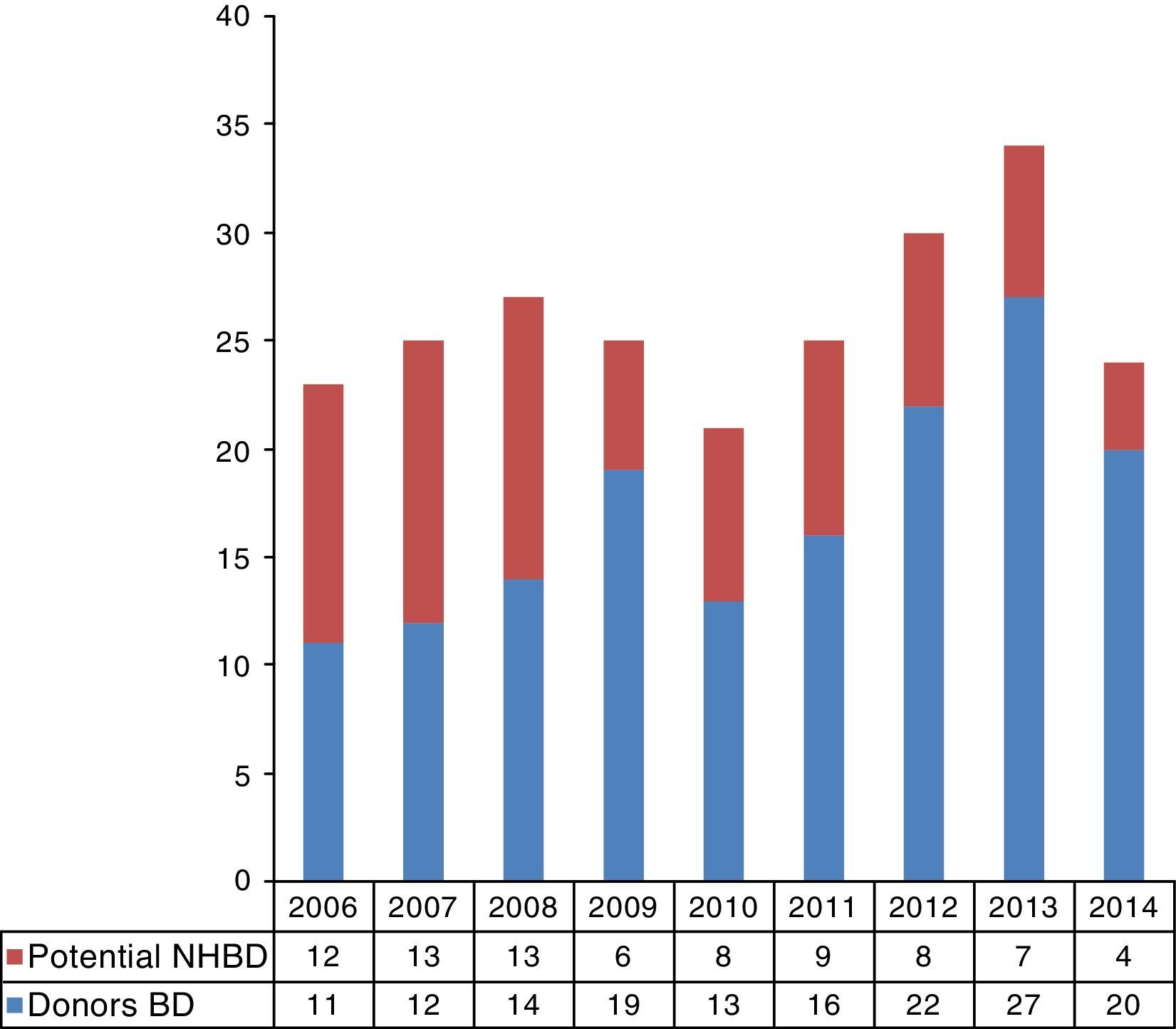
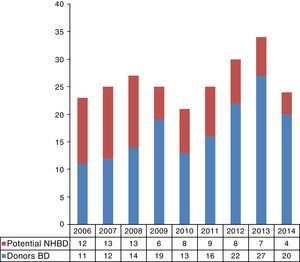
ResultsA total of 1510 patients died in our center during the study period. Of these patients, 462 met the inclusion criteria according to age and electronic diagnostic code. Eighty-six patients (18.6%) evolved toward BD, and in 20 cases the case history could not be retrieved—these subjects being excluded from the study. We subsequently reviewed the case histories of the remaining 356 patients, discarding those meeting donation exclusion criteria. In accordance to the type of death, 288 of these patients corresponded to possible NHBDII and 68 to possible NHBDIII. Following detailed review of the case histories, we identified 70 potential NHBDII and 10 potential NHBDIII during the 9-year study period (Fig. 1). On considering the mean rejection rate in our hospital during those years (9.3%; data not published), we could assume an average of 8.9 donors a year in the context of NHBD. On extrapolating these data to the recruitment population of our hospital (approximately 170,000 inhabitants),20 it may be concluded that there was an increase of 47 donors per million population (pmp). The time course of the potential NHBD (types II and III) calculated with respect to the real brain dead donors are shown in Fig. 2.
The main Departments implicated in possible NHBDII were the Intensive Care Unit (32.3%), followed by Internal Medicine (14.1%), the Postanesthesia Resuscitation Unit (13.8%), Digestive Diseases (13.8%) and Emergency Care (10.4%). The Departments implicated in possible NHBDIII were the Intensive Care Unit (42.6%), followed by Internal Medicine (20.6%), Digestive Diseases (11.7%), Neurology—Neurosurgery (10.3%) and Pneumology (6%).
As regards the type of LLST, the decision not to introduce new life support treatments was made in 59% of the cases, with the withdrawal of life support measures in 10%, and discharge from the ICU in 4%. In 26.5% of the cases no limitation measures were stated in the case history (though this information was recorded by the nursing staff). With regard to the time elapsed from the decision referred to LLST and patient death, we only obtained information corresponding to 26 patients, where the median was found to be 24h (P25: 1.75; P75: 48).
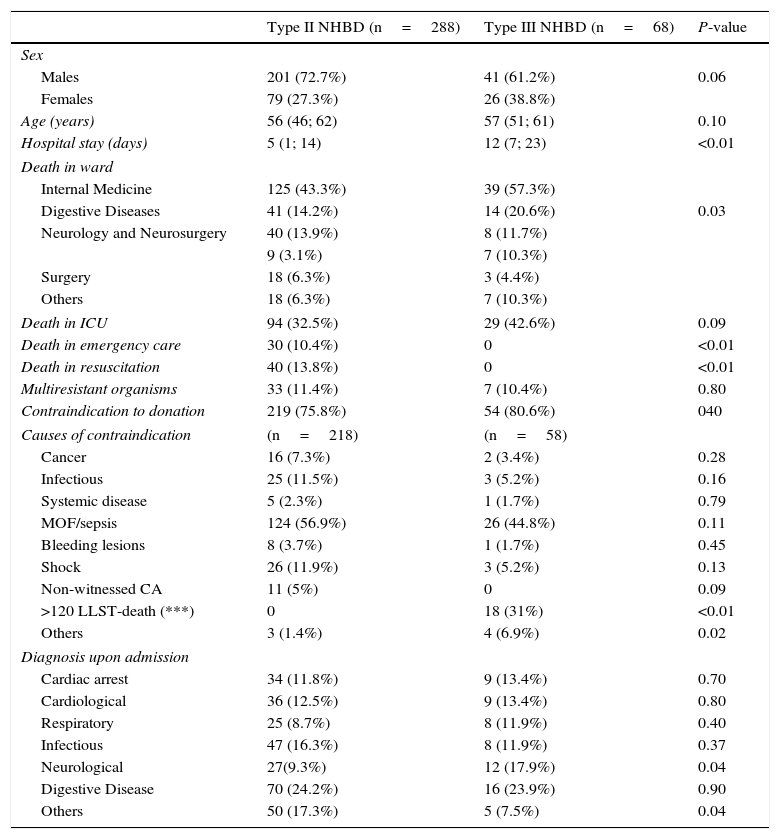
On comparing NHBDII versus NHBDIII (Table 1), we recorded a greater proportion of males in the former group, though statistical significance was not reached. Significantly longer stays were recorded in NHBDIII, and these patients died more often in the hospital ward, with a greater proportion of neurological disease upon admission.
Comparison between type II and type III non-heart beating donors.
| Type II NHBD (n=288) | Type III NHBD (n=68) | P-value | |
|---|---|---|---|
| Sex | |||
| Males | 201 (72.7%) | 41 (61.2%) | 0.06 |
| Females | 79 (27.3%) | 26 (38.8%) | |
| Age (years) | 56 (46; 62) | 57 (51; 61) | 0.10 |
| Hospital stay (days) | 5 (1; 14) | 12 (7; 23) | <0.01 |
| Death in ward | |||
| Internal Medicine | 125 (43.3%) | 39 (57.3%) | |
| Digestive Diseases | 41 (14.2%) | 14 (20.6%) | 0.03 |
| Neurology and Neurosurgery | 40 (13.9%) | 8 (11.7%) | |
| 9 (3.1%) | 7 (10.3%) | ||
| Surgery | 18 (6.3%) | 3 (4.4%) | |
| Others | 18 (6.3%) | 7 (10.3%) | |
| Death in ICU | 94 (32.5%) | 29 (42.6%) | 0.09 |
| Death in emergency care | 30 (10.4%) | 0 | <0.01 |
| Death in resuscitation | 40 (13.8%) | 0 | <0.01 |
| Multiresistant organisms | 33 (11.4%) | 7 (10.4%) | 0.80 |
| Contraindication to donation | 219 (75.8%) | 54 (80.6%) | 040 |
| Causes of contraindication | (n=218) | (n=58) | |
| Cancer | 16 (7.3%) | 2 (3.4%) | 0.28 |
| Infectious | 25 (11.5%) | 3 (5.2%) | 0.16 |
| Systemic disease | 5 (2.3%) | 1 (1.7%) | 0.79 |
| MOF/sepsis | 124 (56.9%) | 26 (44.8%) | 0.11 |
| Bleeding lesions | 8 (3.7%) | 1 (1.7%) | 0.45 |
| Shock | 26 (11.9%) | 3 (5.2%) | 0.13 |
| Non-witnessed CA | 11 (5%) | 0 | 0.09 |
| >120 LLST-death (***) | 0 | 18 (31%) | <0.01 |
| Others | 3 (1.4%) | 4 (6.9%) | 0.02 |
| Diagnosis upon admission | |||
| Cardiac arrest | 34 (11.8%) | 9 (13.4%) | 0.70 |
| Cardiological | 36 (12.5%) | 9 (13.4%) | 0.80 |
| Respiratory | 25 (8.7%) | 8 (11.9%) | 0.40 |
| Infectious | 47 (16.3%) | 8 (11.9%) | 0.37 |
| Neurological | 27(9.3%) | 12 (17.9%) | 0.04 |
| Digestive Disease | 70 (24.2%) | 16 (23.9%) | 0.90 |
| Others | 50 (17.3%) | 5 (7.5%) | 0.04 |
Values reported as median, percentile 25 and percentile 75, or number (percentage).
MOF: multiorgan failure; >120 LLST-death: time between limitation of life support treatment and death >120min.
With regard to organ viability, the organs potentially amenable to donation comprised 77 livers, 34 lungs and 138 kidneys. The causes of non-viable livers were: three cases of cirrhosis and one case of acute hepatitis. The lungs were found to be non-viable in 58 patients, due to the following reasons: age in 27 cases, acute lung edema in 12, severe chronic obstructive pulmonary disease in 10, pulmonary thromboembolism in four, pulmonary hypertension in three, pneumonia in 5, cystic fibrosis in one, and acute respiratory distress syndrome in one patient. With regard to the kidneys, donation was not viable in 11 patients due to the presence of chronic renal failure.
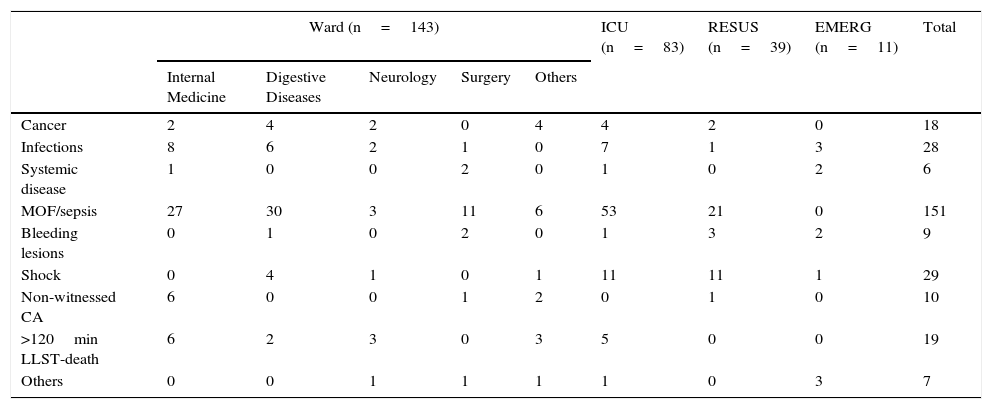
On examining the causes of contraindication to donation according to the Department attending the patient (Table 2), multiorgan failure (MOF) due to sepsis was seen to predominate, followed by shock and infection.
Contraindications to organ donation according to the Department in which the patients die.
| Ward (n=143) | ICU (n=83) | RESUS (n=39) | EMERG (n=11) | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| Internal Medicine | Digestive Diseases | Neurology | Surgery | Others | |||||
| Cancer | 2 | 4 | 2 | 0 | 4 | 4 | 2 | 0 | 18 |
| Infections | 8 | 6 | 2 | 1 | 0 | 7 | 1 | 3 | 28 |
| Systemic disease | 1 | 0 | 0 | 2 | 0 | 1 | 0 | 2 | 6 |
| MOF/sepsis | 27 | 30 | 3 | 11 | 6 | 53 | 21 | 0 | 151 |
| Bleeding lesions | 0 | 1 | 0 | 2 | 0 | 1 | 3 | 2 | 9 |
| Shock | 0 | 4 | 1 | 0 | 1 | 11 | 11 | 1 | 29 |
| Non-witnessed CA | 6 | 0 | 0 | 1 | 2 | 0 | 1 | 0 | 10 |
| >120min LLST-death | 6 | 2 | 3 | 0 | 3 | 5 | 0 | 0 | 19 |
| Others | 0 | 0 | 1 | 1 | 1 | 1 | 0 | 3 | 7 |
MOF: multiorgan failure; >120 LLST-death: time between limitation of life support treatment and death>120min; CA: cardiac arrest; RESUS: resuscitation; EMERG: emergency service; ICU: Intensive Care Unit.
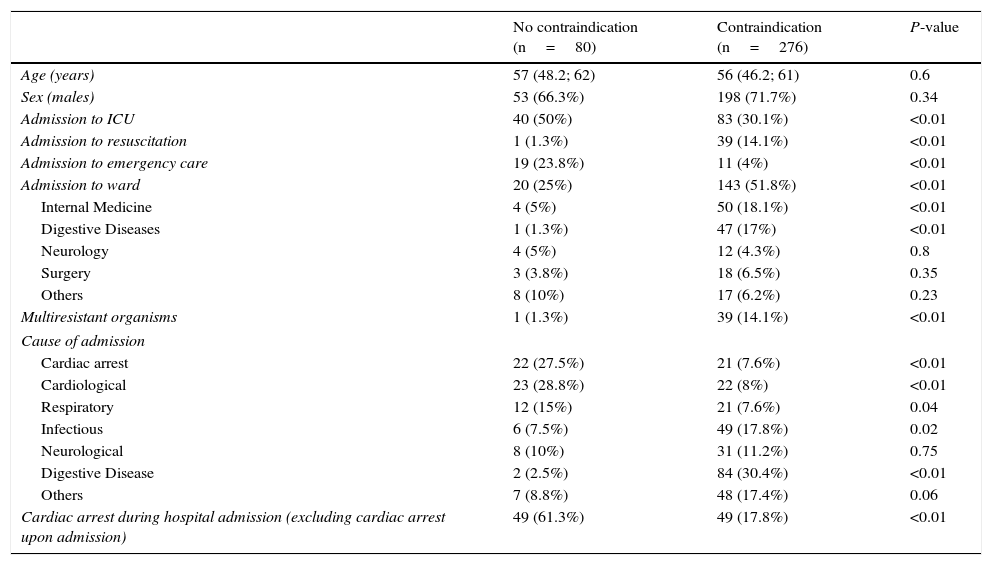
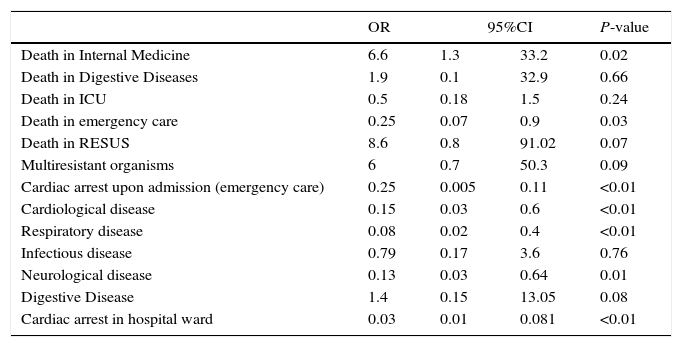
Table 3 shows the variables exhibiting differences on comparing the groups with contraindications versus those without contraindications, based on the univariate analysis. On entering these variables in the logistic regression model, with contraindications to donation as the dependent variable, the results identified the following parameters as protectors against contraindication (Table 4): patient death in the emergency room, cardiological disease, admission due to CA, respiratory and neurological disease upon admission, and CA during hospital stay. The variable death in the Department of Internal Medicine was associated to an increased risk of contraindications to donation.
Comparison between groups with and without contraindications to non-heart beating donation.
| No contraindication (n=80) | Contraindication (n=276) | P-value | |
|---|---|---|---|
| Age (years) | 57 (48.2; 62) | 56 (46.2; 61) | 0.6 |
| Sex (males) | 53 (66.3%) | 198 (71.7%) | 0.34 |
| Admission to ICU | 40 (50%) | 83 (30.1%) | <0.01 |
| Admission to resuscitation | 1 (1.3%) | 39 (14.1%) | <0.01 |
| Admission to emergency care | 19 (23.8%) | 11 (4%) | <0.01 |
| Admission to ward | 20 (25%) | 143 (51.8%) | <0.01 |
| Internal Medicine | 4 (5%) | 50 (18.1%) | <0.01 |
| Digestive Diseases | 1 (1.3%) | 47 (17%) | <0.01 |
| Neurology | 4 (5%) | 12 (4.3%) | 0.8 |
| Surgery | 3 (3.8%) | 18 (6.5%) | 0.35 |
| Others | 8 (10%) | 17 (6.2%) | 0.23 |
| Multiresistant organisms | 1 (1.3%) | 39 (14.1%) | <0.01 |
| Cause of admission | |||
| Cardiac arrest | 22 (27.5%) | 21 (7.6%) | <0.01 |
| Cardiological | 23 (28.8%) | 22 (8%) | <0.01 |
| Respiratory | 12 (15%) | 21 (7.6%) | 0.04 |
| Infectious | 6 (7.5%) | 49 (17.8%) | 0.02 |
| Neurological | 8 (10%) | 31 (11.2%) | 0.75 |
| Digestive Disease | 2 (2.5%) | 84 (30.4%) | <0.01 |
| Others | 7 (8.8%) | 48 (17.4%) | 0.06 |
| Cardiac arrest during hospital admission (excluding cardiac arrest upon admission) | 49 (61.3%) | 49 (17.8%) | <0.01 |
Values reported as median, percentile 25 and percentile 75, or number (percentage).
Binary logistic regression model based on medical contraindication to donation as dependent variable.
| OR | 95%CI | P-value | ||
|---|---|---|---|---|
| Death in Internal Medicine | 6.6 | 1.3 | 33.2 | 0.02 |
| Death in Digestive Diseases | 1.9 | 0.1 | 32.9 | 0.66 |
| Death in ICU | 0.5 | 0.18 | 1.5 | 0.24 |
| Death in emergency care | 0.25 | 0.07 | 0.9 | 0.03 |
| Death in RESUS | 8.6 | 0.8 | 91.02 | 0.07 |
| Multiresistant organisms | 6 | 0.7 | 50.3 | 0.09 |
| Cardiac arrest upon admission (emergency care) | 0.25 | 0.005 | 0.11 | <0.01 |
| Cardiological disease | 0.15 | 0.03 | 0.6 | <0.01 |
| Respiratory disease | 0.08 | 0.02 | 0.4 | <0.01 |
| Infectious disease | 0.79 | 0.17 | 3.6 | 0.76 |
| Neurological disease | 0.13 | 0.03 | 0.64 | 0.01 |
| Digestive Disease | 1.4 | 0.15 | 13.05 | 0.08 |
| Cardiac arrest in hospital ward | 0.03 | 0.01 | 0.081 | <0.01 |
RESUS: resuscitation; ICU: Intensive Care Unit.
The donation potential of the NHBD programs in Spain has not been fully established.21,22 The experience of San Carlos Clinic Hospital,23 involving very strict screening criteria, indicates that the number of used donors from NHBD programs is currently in the range of 15–16 donors pmp. Barcelona Clinic Hospital24 offers similar figures, in the order of 13 real donors pmp. The data are almost exclusively referred to out-hospital cardiac arrest NHBD cases. There are not enough data regarding donation following LLST. In our study we have estimated 80 potential type II and III NHBD in the 9-year study period (2006–2014). On considering the mean rejection rate in our hospital during those years (9.3%), we could assume an average of 8.9 donors a year in the context of NHBD. A full 87.5% of the increment would be at the expense of NHBDII, while the remaining 12.5% would correspond to NHBDIII. On extrapolating these data to the recruitment population of our hospital (approximately 170,000 inhabitants), this may imply an increase of 47 donors pmp.
As regards the characteristics of the patients studied, it is logical for NHBDIII cases to show longer stays than NHBDII patients. In effect, they are individuals in which it takes some time to consider LLST, since the majority do not have treatment limitations upon admission, and LLST is contemplated only as their clinical course becomes extremely unfavorable. Such NHBDIII cases also die more often in the ICU and in the hospital ward (particularly Neurology—Neurosurgery), since it is in these Departments where LLST is considered after a period of maximum therapeutic effort, as evidenced by some recent studies.24
A large proportion of potential NHBDIII patients are carriers of multiresistant microorganisms (MOF)—this being related to their longer hospital stay. The leading contraindication to donation in both groups is the presence of MOF due to sepsis. This suggests that the early detection and treatment of sepsis in the hospital setting, even in patients with LLST, could result in fewer contraindications among the potential donors. In the specific case of NHBDIII, the next most common contraindication to donation would be a time from LLST to death of over 120min. In this regard, an adequate LLST protocol,25,26 with adequate diffusion among the implicated Departments, could improve the process and the recording of LLST, since we found that such records often do not exist (no indication in 26% of the cases), or the data are very scarce (limited to not performing resuscitation maneuvers in most cases [no CPR in 48%]). Of note is the observation that we recorded no NHBDIII cases in the emergency and resuscitation services, since no patient with LLST was registered. In the case of emergency care, these data do not coincide with the findings of a study carried out in France and Belgium,27 where up to 45% of the patients over 65 years of age were indeed subjected to LLST upon admission to the emergency room. This may be explained by the limited diffusion of living wills or advanced directives in Spain, and the tendency toward low LLST rates as evidenced by the Ethicus study28 in the Mediterranean areas. With regard to the patients admitted to resuscitation, LLST probably is applied but is not recorded, and the case is referred to the surgical departments, where LLST is then effectively registered.
In relation to the contraindications to donation in both NHBD groups, we found that patients admitted to Internal Medicine and Digestive Diseases had a greater percentage of contraindications. Following a detailed review of the data, we found that this was due to a large incidence of infectious disease with MOF in Internal Medicine and Digestive Diseases, and a large number of patients with MOF secondary to terminal liver disorders in Digestive Diseases. Patients admitted to the ICU and the emergency service had a lesser proportion of contraindications to donation. There were significantly fewer contraindications in patients admitted due to cardiac arrest, cardiological disease (no CA) and respiratory illness. On the other hand, there was a greater proportion of contraindications in the patients with gastrointestinal disease upon admission.
As a protective factor against contraindications to donation, we identified patient death in the emergency service, while death in Internal Medicine was identified as a risk factor for the presence of contraindications to donation. Patients dying in emergency care have fewer contraindications, since hospital stay is shortened by passing through this service: the patients are not moved to the hospital ward, and they consequently have fewer evolutive complications and nosocomial infections—particularly those admitted under conditions of CA. On the other hand, patients in Internal Medicine often have associated comorbidities, and this Department moreover has a specific area for infectious patients under their care. The observed result is therefore logical considering the type of disorders involved. It also must be taken into account that a form of LLST is the decision not to admit patients to services such as ICU but to refer them to areas such as Internal Medicine. These are typically elderly patients with multiple disease conditions, and with many chances of having contraindications to donation in general.
The estimates referred to donation potential, and specifically the percentage losses due to family refusal, are limited by the fact that the historical rejection rates are extrapolated from family refusals recorded in those years among brain dead donors.
In Spain, it is known that the family refusal rates in type II NHBD are in the order of 6%,1 while data referred to type III NHBD are not yet available. These rejection rates may vary among different types of donors; this fact therefore could be regarded as a limitation of our study. With regard to organ viability, due consideration is required of the number of organs considered not valid after macroscopic assessment by the surgical team. This aspect was logically not evaluable in our study; the data obtained therefore probably overestimate the real number of organs for transplantation. It also must be mentioned that we did not take into consideration the possible losses due to prolonged resuscitation or ischemia times in maintaining these potential donors, since patients with LLST are not subjected to such maneuvers.
In contraposition, the fact that we found very poor and scarce (or inexistent) LLST records suggests that the real number of patients with LLST is underestimated.
In conclusion, and despite all the limitations involved, it seems useful to incorporate an NHBDII and NHBDIII protocol in our hospital, considering that we could increase our donation activity by 47 donors pmp. These patients mainly originate from the Department of Intensive Care Medicine, the emergency service, resuscitation units, Internal Medicine, Digestive Diseases and Neurology. The most frequent cause of contraindication to NHBD in general is the development of MOF due to sepsis, and in the specific case of NHBDIII the leading cause is a prolonged time between LLST and patient death. These data, together with poor specification of the treatment measures to be limited, suggest that developing and improving the hospital sepsis and LLST protocols would be of great help in improving the performance and yield of an NHBD program.
AuthorshipMs. Eva Tenza has carried out the study entitled: Estimation of potential donors after cardiocirculatory death in Elche University General Hospital (Alicante, Spain) as an end of Master project corresponding to the course 2014–2015, within the Master in Research in Organ Donation and Transplantation of the University of Barcelona. This study has not been submitted for publication to date.
Mr. Ricard Valero and Mr. Vicente Arraez contributed as directors of the project and participated in the review of the manuscript. All of them agree to the final version of the article.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Tenza E, Valero R, Arraez V. Estimación de potenciales donantes en muerte cardiocirculatoria en el Hospital General Universitario de Elche. Med Intensiva. 2017;41:153–161.