Propofol is a widely used phenol derivative with sedative and hypnotic properties.1 Among its cardiovascular effects we may find the dose-dependant reduction of pre-load, post-load, and myocardial contractility as the most widely known ones,1 although other effects have come up recently such as its potential protective role in the ischaemia-reperfusion damage,2 its influence on the cardiac conduction system,3,4 and its capacity to modify the action potential phases since it can act on the ionic channels of the myocyte membrane.4,5 These effects provide this drug with antiarrhythmic properties, even though the evidence and clinical experience on this field is still scarce.6–9 This is why we decided to conduct a retrospective analysis on the clinical histories of patients who got medical assistance in our hospital and presented with supraventricular tachyarrhythmias, and who restored their sinus rhythm after the administration of propofol without the need for any further manoeuvres. We designed a protocol for the collection of data aimed at homogenizing all information, and brought it to our hospital ethics committee that would later approve it (HCB Code/2016/0751, approval date October 24th, 2016).
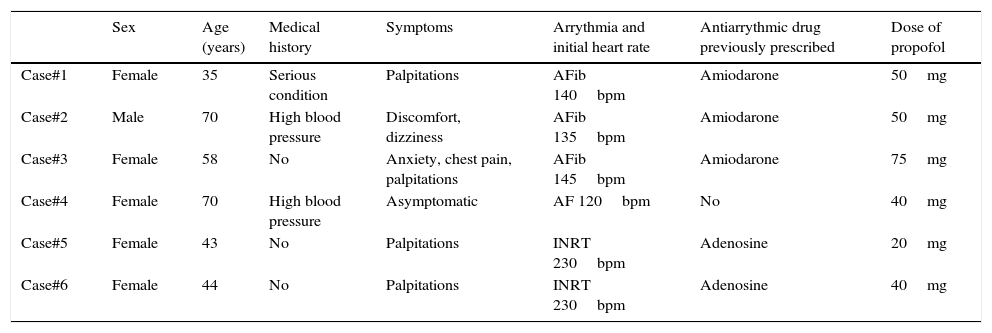
Six patients were included in this analysis between January 2010 and April 2016. The age range of most women (83.33 per cent) was between 35 and 70years of age (53.3±13.53). The arrhythmias detected were atrial fibrillation (AFib) (50 per cent), intranodal re-entrant tachycardia (INRT) (33.3 per cent), and atrial flutter (AF) (16.7 per cent). Nearly all cases presented at the ER with symptoms associated with any of these arrhythmias, being palpitations and chest pains the most common symptoms of all. Only one case happened in the ophthalmology operating room but the patient remained asymptomatic (Table 1).
Characteristics of patients.
| Sex | Age (years) | Medical history | Symptoms | Arrythmia and initial heart rate | Antiarrythmic drug previously prescribed | Dose of propofol | |
|---|---|---|---|---|---|---|---|
| Case#1 | Female | 35 | Serious condition | Palpitations | AFib 140bpm | Amiodarone | 50mg |
| Case#2 | Male | 70 | High blood pressure | Discomfort, dizziness | AFib 135bpm | Amiodarone | 50mg |
| Case#3 | Female | 58 | No | Anxiety, chest pain, palpitations | AFib 145bpm | Amiodarone | 75mg |
| Case#4 | Female | 70 | High blood pressure | Asymptomatic | AF 120bpm | No | 40mg |
| Case#5 | Female | 43 | No | Palpitations | INRT 230bpm | Adenosine | 20mg |
| Case#6 | Female | 44 | No | Palpitations | INRT 230bpm | Adenosine | 40mg |
AF: atrial flutter; AFib: atrial fibrillation; INRT: intranodal re-entrant tachycardia.
The cases of AFib were interpreted as episodes of paroxistic AFib, which is why pharmacological cardioversion was attempted with amiodarone (they received one IV bolus of 300mg, and then continuous perfusion of 900mg in 24hours). The cases of INRT received carotid massages plus IV adenosine (up to 24mg) before making any decision to perform electrical cardioversions.
The administration of propofol in the cases that presented with AFib and INRT attempted to initiate a process of deep sedoanalgesia in order to perform an electric cardioversion procedure once other antiarrhythmic measures had failed. When it comes to the female patient with AF, the hypnotic drug was administered as an inducer to be able to perform the peribulbar ophtalmic blockade. The average dose administered was 45.8mg±16.4mg (range 20–75mg). The patients with INRT received lower doses (20–40mg) compared to those with paroxistic AFib (50–75mg). All of them received the hypnotic drug through one IV bolus and reversion to sinus rhythm occurred within the first two minutes after the administration of the drug. The 6 cases were discharged from the hospital in sinus rhythm after a period of 4±1.3hours. None of the patients came back to the hospital days later with a new episode of arrhythmia in the 6-month follow-up that we conducted. These data are shown in Table 1.
There are isolated reports of reversion to sinus rhythm of supraventricular tachyarrhythmias after the administration of propofol in adult patients.6–9 Kannan and Sherwood6 reported the case of a sixty-eight year old patient with a history of ischaemic heart condition who presented with atrial flutter that could be reversed after the administration of one IV bolus of 100mg of propofol. Similarly, and in the same journal, Magaldi et al.7 reported one of the six cases collected in the analysis where they talked about the possible antiarrhythmic properties of the drug in a seventy year old patient with reversion of AF after the administration of 40mg de propofol. Similarly, Choi and Jee8 describe 2 cases of women with AF who received both remifentanil and propofol through target-controlled infusion during surgical acts (propofol dose of 3.7 and 2.5μg/ml), achieving reversion to sinus rhythm 10 and 30minutes after initiating the perfusion, respectively. The average dose administered to our patients was 45mg. We should mention that the wide variability of the doses administered, also mentioned in the reference and in our patients might be due to a prior use of antiarrhythmic drugs, to the anthropometric characteristics of the subjects, and to the physiopathogenic mechanism of the arrhythmias (re-entrant, abnormal automacity, etc.).
Although the cardiovascular effects of alkylphenol are well known since it was first introduced, the mechanisms through which it acts upon the cardiac conduction system are still under study today. In electrophysiological studies of patients with AFib, a decrease in the P-wave dispersion when homogenizing and regularizing the spreading compared to the atrial wall depolarization could be confirmed, being this effect even more relevant when the AFib was paroxistic.5 On the other hand, in experimental models of myocardial ischaemia-repefusion,1 propofol has proven beneficial effects since it reduces the trend towards action potential shortening in ischaemic regions, which in turn leads to a reduced incidence of functional re-entrant tachyarrhythmias. These intrinsic antiarrhythmic effects of propofol seem to be mediated by its proven inhibitory effects on the potassium channels responsible for the repolarization phases 1 and 3 (Ito, and IKUR, and ATP-sensitive, respectively), and the calcium channels involved in repolarization phase 2 (ICa).3,4
To the aforementioned direct effects of propofol on the myocardium and the myocardial conduction tissue, we should add its influence on the autonomic nervous system (ANS), which has indirect repercussions on the heart. Propofol supresses the activity within the ANS, though its effect is significantly greater on the adrenergic system.10 The resulting parasympathetic predominance may be one of the mechanisms that condition the reduction of arrhythmias due to abnormal automaticity, as it is the case with myocardial ischaemia.
Although our study shows the series with the largest number of patients ever recorded where the possible antiarrhythmic properties of propofol are shown, there are relevant plausible limitations that we should comment. In the first place, since it is a descriptive analysis, there is no way of confirming the real cause-effect hypothesis. Also, the very natural history of this type of arrhythmias may be limiting. The paroxistic AFib, the AF, and the INRT are arrhythmias that may appear occasionally and cause a spontaneous reversion to sinus rhythm, so it is possible that, while propofol was being administered, the arrhythmia just ceased. Lastly, the prior administration of amiodarone in cases of AFib may have had an influence on the reversion after the administration of propofol, although initially (after the total dose of 1200mg of amiodarone in 24hours) the goal of sinus rhythm control was not accomplished.
As a conclusion and with the evidence available today, we the authors believe that prospective and comparative trials should be conducted in order to assess the real effectiveness of this drug in the context of stable supraventricular tachyarrhythmias that do not respond to other medications.
Conflict of interestsThe authors declare that there are no conflicts of interest whatsoever or any financing from public or private entities, research centres, or foundations.
Please cite this article as: Montero-Tinnirello J, Magaldi M, Fontanals J, Masgoret P, Bravo JC. Reversión de taquiarritmias supraventriculares tras la administración de propofol. Serie de casos. Med Intensiva. 2017;41:499–501.