A few days ago, new definitions of sepsis and septic shock were launched as a result of a consensus of 19 experts SCCM (Society of Critical Care Medicine) and ESICM (European Society of Intensive Care Medicine).1
Perhaps the greatest contribution of this expert opinion consensus has been to recognize sepsis as a difficult to characterize syndromic condition, with a cellular metabolic disorder as a lead condition along with the development of organ failure. However, as the most important feature, the new definition excludes the concept of SIRS (Systemic Inflammatory Response Syndrome) since this term is being considered of not useful anymore. The authors supported this decision mainly based on a retrospective study conducted in Australia and New Zealand2 in which it was observed (glass half-empty approach) that 1 out of 8 patients (12.5%) with sepsis and multiorgan failure (MOF) did not have at least 2 SIRS criteria. However, these results (glass half-full approach) could be reinterpreted as 7 out of 8 patients (87.5%) did present positive SIRS criteria.
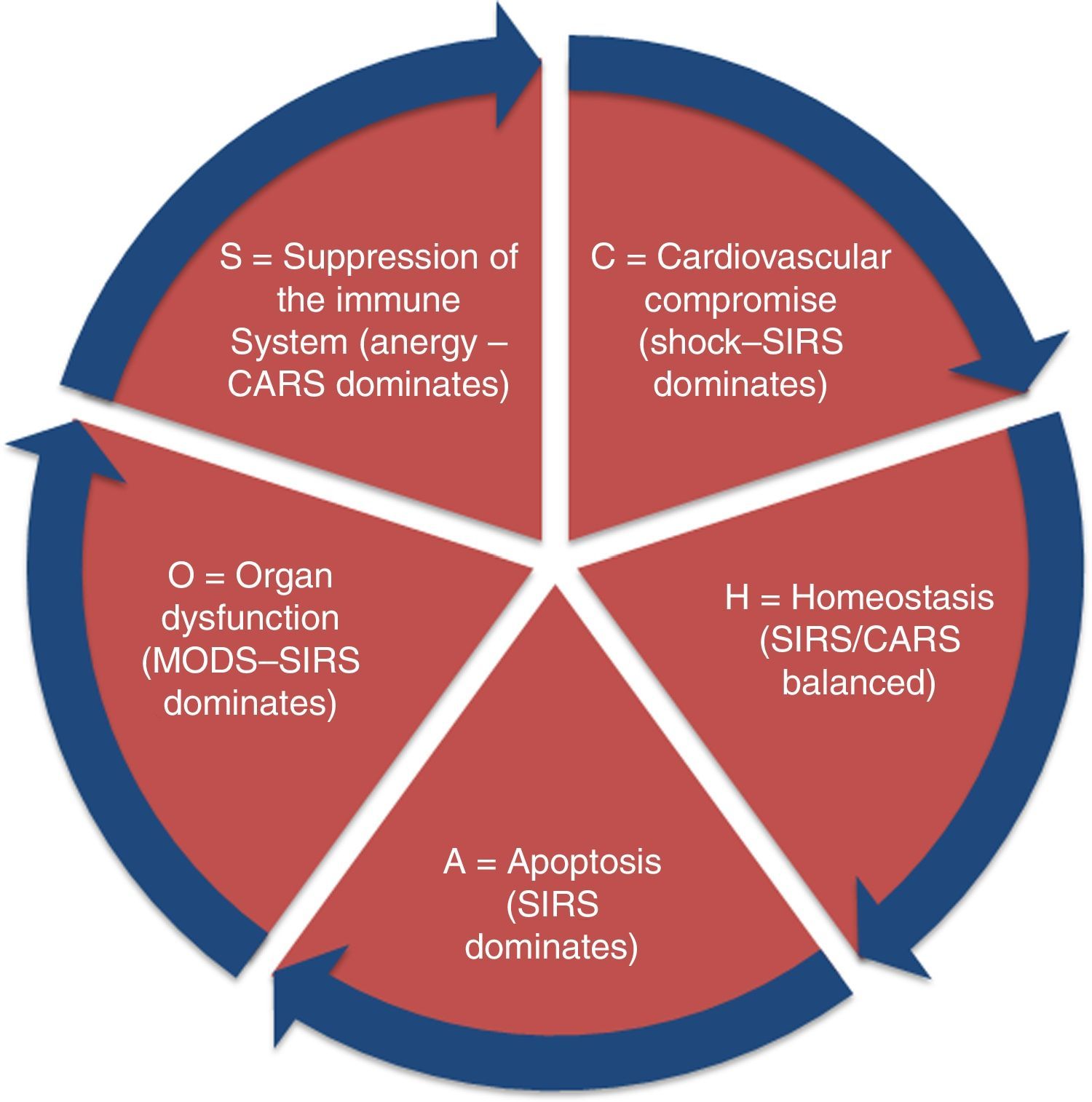
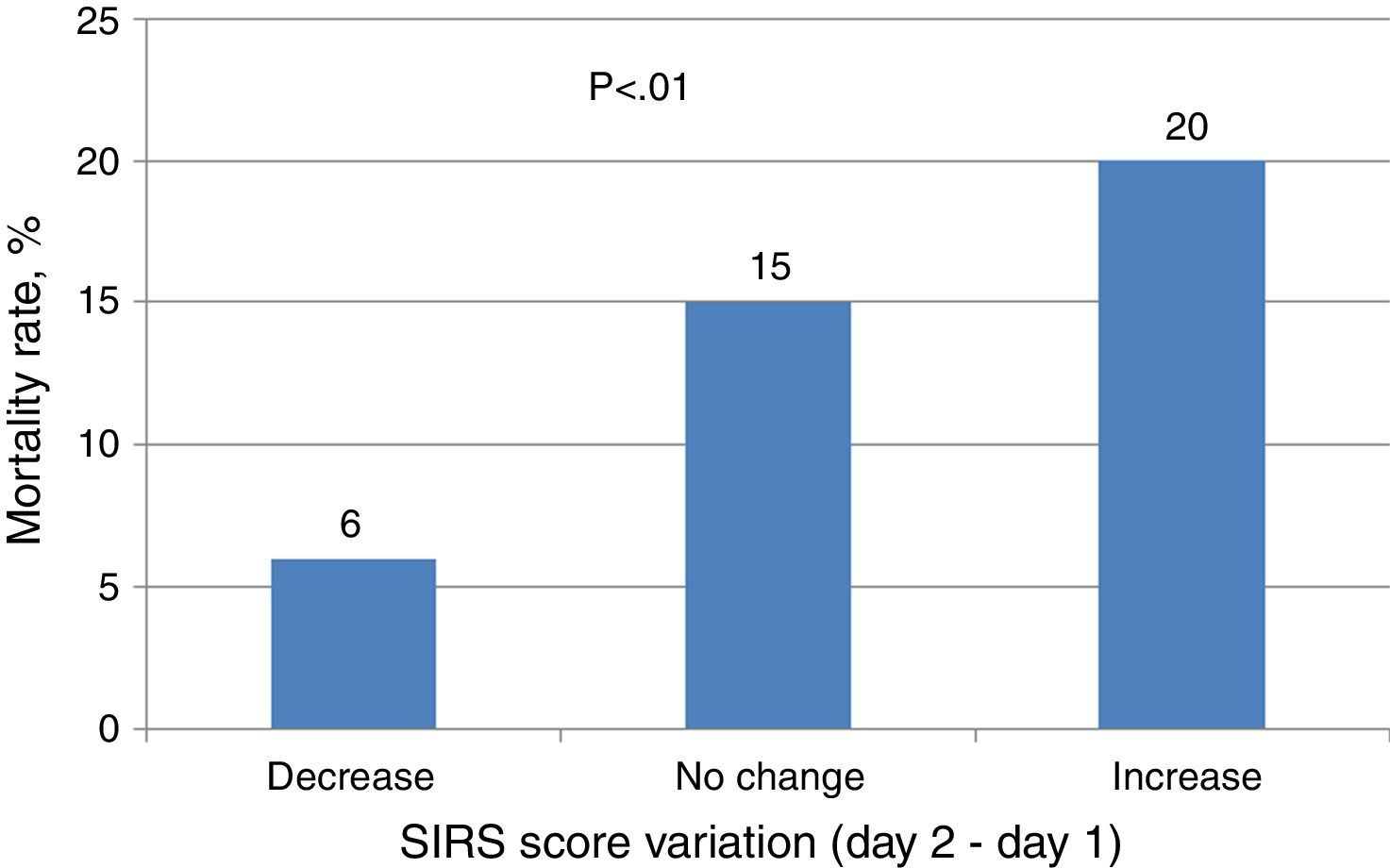
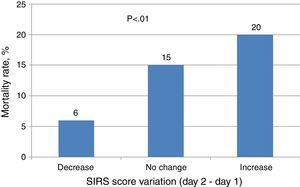
Furthermore, the authors, in the paper on new sepsis definitions, affirmed that SIRS does not represent a dysregulated systemic response compromising host survival for the diagnosis of sepsis anymore. The concept of SIRS, such as expressed by Bone et al.3 is a clear one and refers to non-specific inflammatory response of the host to an injury. The theory of “CHAOS” proposed by Bone (Fig. 1) masterfully develops the different interactions between the pro and anti-inflammatory response of the host taking into account a translational view, which has elucidated the different phases or states of patients with sepsis. Moreover, several studies have found a direct association between SIRS severity and clinical progression. Rangel-Frausto et al.4 showed that mortality significantly increased from 7% to 17% based on the number of SIRS criteria (from two to four respectively). Interestingly, Napolitano et al.5 observed in trauma patients the relative risk (RR) of mortality increased from 3.46 (interquartile range [IQR=1.48–8.11], p=0.004) with a SIRS score=2–6.88 [1.81–22.8], p=0.004 for SIRS=4. In addition, Barie and Hydo6 reported that the change in SIRS score within the first 24h of treatment was significantly associated with mortality (Fig. 2).
Moreover, to define sepsis based on organ dysfunction may have serious limitations. The SOFA score was designed to estimate more objectively organ dysfunction associated with sepsis7 and its use is common in intensive care units (ICUs), but not in other health care settings,8 where a more large number of patients with sepsis are screened. This is by far the area of detection and Sepsis Code activation.
In the other hand, it important to highlight that with the previous definitions and international campaigns implementations based on such, mortality of sepsis has dramatically decreased.9 As other authors have previously acknowledged it, SIRS and MOF are not syndromes but merely concepts. SIRS criteria are non-specific physiological responses to an aggression to the host. Whilst SIRS should be promptly identified, MOF should be considered a delayed failure to an inadequate clinical response.
Another important aspect of the recently launched definitions of sepsis is the proposal of “quick SOFA” as a criterion for suspected sepsis if there are two of the three criteria chosen (systolic blood pressure <100mmHg, tachypnea >22min–1 or altered mentation [derived from Glasgow Coma Score <13]) while SIRS (including tachycardia >90 and tachypnea >20) criteria is deleted. Unfortunately, there is a potential exclusion of physiopathology concept. Vasoconstriction and tachycardia are physiological mediated responses aimed to keep adequate oxygen transport and metabolism. This phenomenon has been extensively studied showing a good correlation between shock index (heart rate/systolic blood pressure ratio) and mortality. This concept is extremely valid and useful in young patients or patients without chronic diseases.10–12 Moreover, based on new definitions, to have chosen just hypotension or altered sensorium for sepsis detection, may (a) delay essential therapeutic measures such as early administration of antibiotics and (b) accepting organ failure establishment as the first sign of detection.
As a common rule, the choice of one or other clinical indicator should be related to the goal to be achieved. Thus, if the goal is to detect promptly a wide number of patients at risk (even with the risk of over diagnosis) of one event (sepsis), a very sensitive indicator should be chosen even when less associated specificity. The recent definitions focus on a more specific goal, organ dysfunction, which will somehow jeopardize the detection of patients with sepsis with both lack or delayed identification of patients at risk. Like in other diseases (i.e. stroke, myocardial infarction), the efforts have been made in early detection campaigns rather than very specific approaches.
We have to acknowledge the limitations of the former definitions especially severe sepsis and the new interpretation of septic shock. Now, shock is defined, as a clinical condition associated to vasopressor requirement to maintain a mean arterial pressure of 65mm Hg or greater and serum lactate level greater than 2mmol/L (>18mg/dL) in the absence of hypovolemia. This is something that might be applicable only within the first hours of resuscitation to identify patient's response but not to define a clinical state. It is true that different recent clinical trials have shown an unexpected low mortality in some patients with septic shock. However, there is a lack of timing with this very important change in the concept. For instance, if a patient has a sustained high lactate level, would this define a terminal event after a failure in resuscitation instead?
In summary, we consider that new definitions must foster to adequately characterize identification, management and stratification with an integrative clinical and pathophysiological approach. We wonder, after a careful review of the new definitions, if they are just a confusing episode of research or they bring anything truly needed to improve current clinical practice.
Conflict of interestThe authors declare no conflict of interest.