Real body weight and height are essential data to be obtained in all critically ill patients (CIP), due to their influence in the designing of therapies and monitoring. Visual estimation is a very inaccurate practice. No precise descriptions of anthropometric measurements among CIP are available in the clinical practice guides.
ObjectiveTo describe anthropometric quality in CIP, health professional perception of such quality, and its influencing factors.
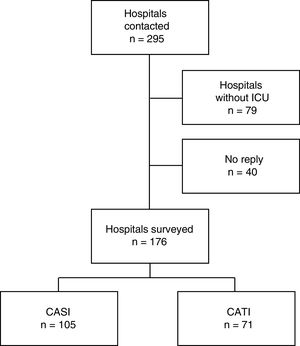
DesignComputer-assisted telephone or self-interviewing.
SettingDoctors and nurses of all Spanish Intensive Care Units (ICU) attending adults.
Relevant variablesAnthropometric practices were described in detail, along with the proclivity to obtain real measurements, and the influence of professional experience, the number of ICU beds, and the health professional group involved.
ResultsA total of 481 questionnaires were collected from 176 hospitals (36.8% from physicians). The availability of measuring tools is limited (weight 68.7% – height 76.7%), with no relation to the number of ICU beds (weight p=.343, height p=.61). Visual estimation was the most frequent way of obtaining measurements (weight 65.9% – height 64.8%), even when measuring tools were available. Willingness to take real measurements was very low, especially among physicians, and professional experience was associated to increased rejection (p<.001).
ConclusionsVisually estimated measurements exceed real measurements in the routine practice of Spanish ICUs. Measurement tools are not widely available in the ICU, and even when available, their use is not guaranteed. The surveyed population does not view anthropometric measures as being important for clinical practice. An effort should be made by scientific societies to promote reliable anthropometric practice in Spanish ICUs.
El peso y la talla reales son datos de inexcusable obtención en todos los pacientes críticamente enfermos (PCE) por su implicación en el diseño de las terapias y la monitorización. La estimación visual es una práctica poco fiable. No existe una descripción precisa en las guías de práctica clínica del PCE acerca de la obtención de medidas antropométricas.
ObjetivoDescribir la calidad en la práctica de la antropometría en el PCE, la percepción de los sanitarios y los factores influyentes.
DiseñoEntrevista telefónica y personal asistida por ordenador.
ÁmbitoMédicos y diplomados en Enfermería de todos los servicios de Medicina Intensiva (UCI) de adultos del territorio español.
Variables de interésSe exploró la práctica habitual de toma de medidas, la proclividad al uso de medidas reales y la influencia de la experiencia, el tamaño de la UCI y el grupo profesional.
ResultadosSe obtuvieron 481 cuestionarios desde 176 hospitales, el 36,8% de médicos. La dotación en equipos de medida es escasa (peso 68,7%, talla 76,7%) y no se relaciona con el tamaño de la UCI (peso p = 0,343, talla p = 0,61). La estimación visual es la forma más frecuente de obtener medidas (peso 65,9%, talla 64,8%), incluso cuando se dispone de herramientas de medida. La disposición a la toma de medidas reales es baja, sobre todo entre médicos (36,2% de rechazo) y mayor experiencia asoció mayor rechazo (p < 0,001).
ConclusionesLa estimación supera a la toma de medidas reales en la rutina de las UCI españolas. Las herramientas de medida no están ampliamente disponibles en las UCI y su uso es minoritario aun existiendo. La población encuestada es poco tendente a considerar importante la toma de medidas. Debe realizarse un esfuerzo por parte de las sociedades científicas para promover la práctica antropométrica fiable en las UCI españolas.
None of the scientific societies that publish guides on the management of acute and critically ill patients doubt the need for measuring the body weight and height of those subjects admitted to the Intensive Care Unit (ICU), though they do not specify exactly how such measurements are to be obtained. These parameters are essential for planning the treatment of critically ill patients, since many management interventions require rigorous body weight measurement, such as protective mechanical ventilation; the administration of vasoactive drugs, inotropic agents, aminoglycosides, glycopeptides or antiseizure drugs; and artificial nutrition support. Error in measuring body weight can result in overdosing, with the associated increase in risk of adverse effects, or in underdosing, with failure to obtain the expected benefits. Previous studies have pointed out the incapacity of healthcare staff to adequately estimate the measurements of critically ill patients within tolerable limits of error,1,2 though despite this fact estimation appears to remain the most widely used strategy for recording patient weight and height in the ICU.
Although it seems reasonable that anthropometric measurements should be the standard in the ICU, the literature indicates that this practice is neither widespread nor protocolized. We decided to carry out a national survey to define anthropometric practices in Spain.
Material and methodsA population-based descriptive study involving census sampling was carried out, with the development of a questionnaire for administration to all hospitals of the Spanish public healthcare system. The hospitals and number of beds were recorded from the Spanish National Hospitals catalog of 2013, published by the Spanish Ministry of Health, Social Services and Equality.3 A total of 96 Social Security hospitals, two central administration hospitals, 168 Autonomous Community hospitals, 14 provincial authority (Diputación) hospitals and 15 municipal hospitals were included.
The questionnaire was administered in two ways: computer-assisted telephone interviewing (CATI) and computer-assisted self-interviewing (CASI). If no reply was received from a given center, up to two further attempts were made, spaced 30 days apart.
A pilot survey was conducted in two phases, targeted to: (1) the nursing supervisor (NSICU) and nursing staff (NS) of our center; and (2) the NSICU, NS and physicians of Torrevieja University Hospital (Alicante, Spain).
We attempted to establish telephone contact with all the selected hospitals and interview the NSICU. In the absence of the NSICU, we requested his or her e-mail and the possibility of talking to a physician. We asked those interviewed to distribute the questionnaire among the rest of the physicians and NS of their Department.
An online form was developed using Google SpreadSheets® (Google Inc., 1600 Amphitheatre Parkway, Mountain View, CA, USA), and was completed during the CATI, with access through a link provided in the letter of request for participation in the study. This letter was sent to the e-mail list of the Spanish Society of Intensive Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva y Unidades Coronarias [SEMICYUC]) and to the e-mail addresses which we were given during the CATI interviews.
At the end of the interview we requested the e-mail address of the participant, which in turn was used to explore the database in search of duplications. For defining objective questions such as the existence of a protocol or of measurement tools, a single reply per center was required. The defined order in selecting the reference questionnaire per center was: (1) the NSICU; (2) the physician of greatest experience; and (3) the NS of greatest experience.
In contrast, when dealing with questions exploring subjective perceptions, we analyzed the total interviewed sample.
The database was developed from Google SpreadSheets®, with coded access and authorization of the principal investigators and study collaborators using a password.
The questionnaire consisted of 7 sections with a cascade format that avoided inadequate questions and minimized the risk of antagonic answers (Annex 1, Supplementary material). The time taken to answer the largest number of questions in the CATI was about 3min on average. Anthropometric measurement practices were documented by means of closed questions, while perception of the relevance of such measurements was explored by questions scored on a 5-point Likert scale.
The validity of the questionnaire was established from expert evaluation of its contents, in view of the lack of a gold standard; the quality of the construct in answering the study hypothesis; and concordance or agreement with previously published experiences.
The data were analyzed using the Statistical Package for the Social Sciences (SPSS Inc., IBM, Armonk, NY, USA), version 22. Categorical variables were reported as frequencies and percentages, while continuous variables were reported as the mean and standard deviation (SD) in the presence of a normal distribution, or as the median and interquartile range (IQR; percentiles 25–75) in the presence of a non-normal distribution. Percentages were compared using the chi-squared test (χ2) or the Fisher exact test, as applicable, while means were contrasted with the Student t-test, and medians with the Mann–Whitney U test.
The hospitals were classified into four groups according to the number of beds (<100, 100–199, 200–499 and ≥500), while the ICUs were classified into three groups (<10, 10–15 and >15 beds). The comparison of medians referred to the number of ICU beds according to hospital size was carried out using Kruskal–Wallis analysis of variance. Statistical significance was considered for p≤0.05.
Analysis of the Likert scale questions was made by standardizing the typical scores as stanine scores. The criterion involved grouping into intervals with one same standard deviation magnitude, with a final group number of 9 – each comprising the mean and standard deviation, except the two extremes (1 and 9). Such grouping served to minimize small inter-individual differences and reduced the total number of distinct scores, thereby simplifying the analysis. The stanine scores were graphically displayed grouped by healthcare position.
In order to compare the propensity to use anthropometric measurements, an indifferent attitude was defined as the mean±0.5 times the SD of the aggregation of answers. We applied the chi-squared test (χ2) and strength of association with the odds ratio (OR) for the rejection or trend groups. Lastly, the propensity analysis was adjusted to the age of the interviewed individual based on the comparison of means with the Student t-test, and to the healthcare position using the χ2 test.
Scientific endorsement was obtained from the SEMICYUC, with approval of the study from the Clinical Research Ethics Committee (CREC) of Torrevieja University Hospital. Data confidentiality was guaranteed by processing them in the database with TLS 1.2 (Transport Layer Security).
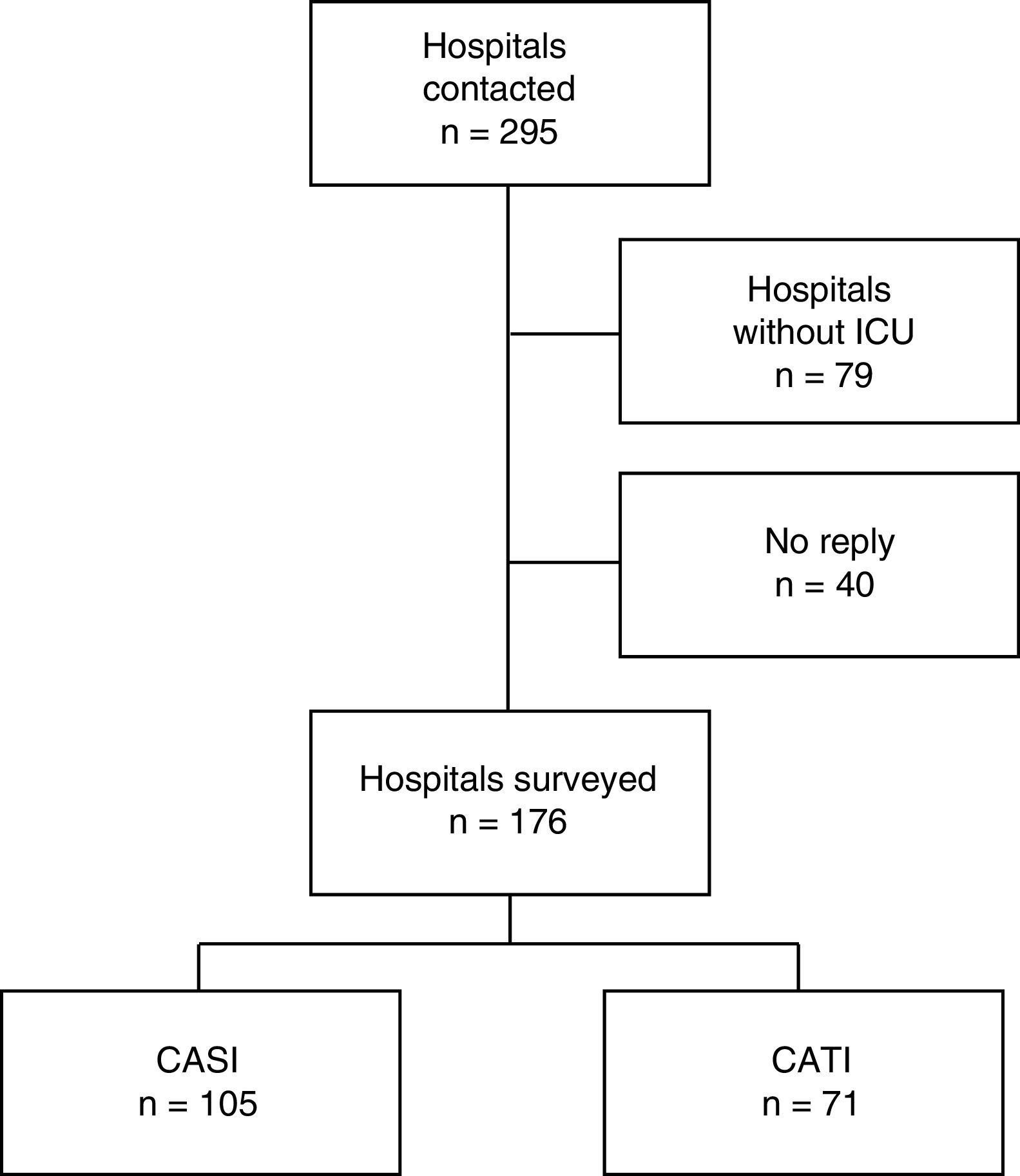
ResultsA total of 295 hospitals throughout Spain were contacted by telephone and/or e-mail between October and December 2013 (Fig. 1). We obtained 481 questionnaires corresponding to 176 hospitals, with representation of all 17 Autonomous Communities and of one autonomous city (Fig. 2). Those selected for evaluating measurement instruments, protocols and care activity in the ICU were 107 nursing supervisors (NSICU), 53 physicians with an average experience of 18.5 years, and 16 nursing staff (NS) members with an average experience of 18.1 years.
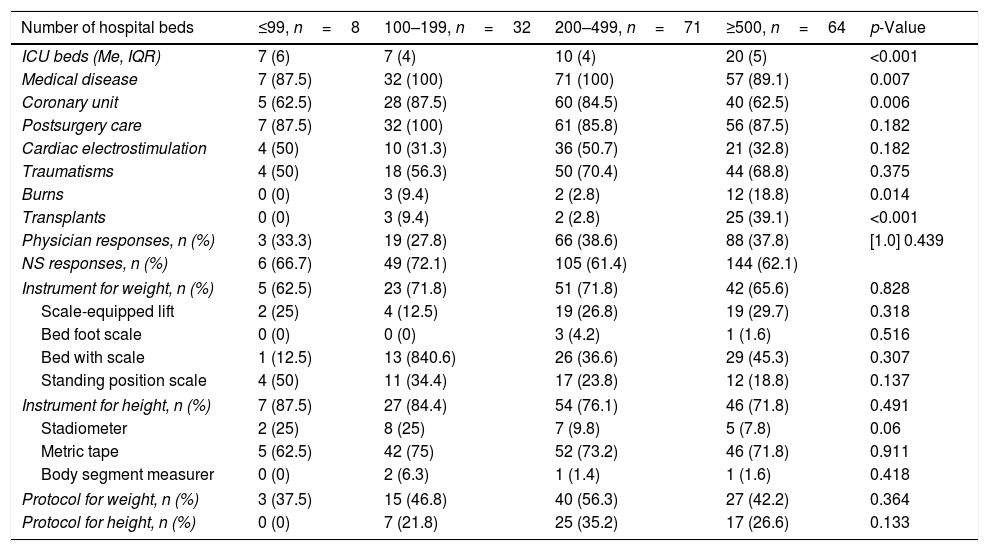
Hospitals of different sizes and with ICUs characterized by different care competences participated in the study (Table 1); 62 hospitals had <10 beds (35.2%), 60 had between 10 and 15 beds (34.1%), and 54 had >15 beds (30.7%). There were no significant differences in the number of responses according to the size of the hospital or among the different interviewed professional groups.
Distribution of the type of medical care, ICU beds, responses, protocols and measurement instruments according to hospital size.
| Number of hospital beds | ≤99, n=8 | 100–199, n=32 | 200–499, n=71 | ≥500, n=64 | p-Value |
|---|---|---|---|---|---|
| ICU beds (Me, IQR) | 7 (6) | 7 (4) | 10 (4) | 20 (5) | <0.001 |
| Medical disease | 7 (87.5) | 32 (100) | 71 (100) | 57 (89.1) | 0.007 |
| Coronary unit | 5 (62.5) | 28 (87.5) | 60 (84.5) | 40 (62.5) | 0.006 |
| Postsurgery care | 7 (87.5) | 32 (100) | 61 (85.8) | 56 (87.5) | 0.182 |
| Cardiac electrostimulation | 4 (50) | 10 (31.3) | 36 (50.7) | 21 (32.8) | 0.182 |
| Traumatisms | 4 (50) | 18 (56.3) | 50 (70.4) | 44 (68.8) | 0.375 |
| Burns | 0 (0) | 3 (9.4) | 2 (2.8) | 12 (18.8) | 0.014 |
| Transplants | 0 (0) | 3 (9.4) | 2 (2.8) | 25 (39.1) | <0.001 |
| Physician responses, n (%) | 3 (33.3) | 19 (27.8) | 66 (38.6) | 88 (37.8) | [1.0] 0.439 |
| NS responses, n (%) | 6 (66.7) | 49 (72.1) | 105 (61.4) | 144 (62.1) | |
| Instrument for weight, n (%) | 5 (62.5) | 23 (71.8) | 51 (71.8) | 42 (65.6) | 0.828 |
| Scale-equipped lift | 2 (25) | 4 (12.5) | 19 (26.8) | 19 (29.7) | 0.318 |
| Bed foot scale | 0 (0) | 0 (0) | 3 (4.2) | 1 (1.6) | 0.516 |
| Bed with scale | 1 (12.5) | 13 (840.6) | 26 (36.6) | 29 (45.3) | 0.307 |
| Standing position scale | 4 (50) | 11 (34.4) | 17 (23.8) | 12 (18.8) | 0.137 |
| Instrument for height, n (%) | 7 (87.5) | 27 (84.4) | 54 (76.1) | 46 (71.8) | 0.491 |
| Stadiometer | 2 (25) | 8 (25) | 7 (9.8) | 5 (7.8) | 0.06 |
| Metric tape | 5 (62.5) | 42 (75) | 52 (73.2) | 46 (71.8) | 0.911 |
| Body segment measurer | 0 (0) | 2 (6.3) | 1 (1.4) | 1 (1.6) | 0.418 |
| Protocol for weight, n (%) | 3 (37.5) | 15 (46.8) | 40 (56.3) | 27 (42.2) | 0.364 |
| Protocol for height, n (%) | 0 (0) | 7 (21.8) | 25 (35.2) | 17 (26.6) | 0.133 |
NS: nursing staff; Me: median; IQR: interquartile range.
A total of 36.8% of those interviewed were specialists in Intensive Care Medicine, with an average professional experience of 16.5 years (SD 9.8); 23.3% were nursing supervisors with an experience of 14.8 years (SD 9.8); and 39.8% were nurses with an experience of 10.8 years (SD 7.1).
Patient body weight and height were not jointly compiled: 48.8% of the hospitals claimed to record weight while only 28.4% recorded height. Recording of the measurements was based on a protocol in 57.7% of the centers in the case of body weight and in 41.3% of the centers in the case of height. However, only 62.8% of those interviewed considered adherence to the protocol to be correct.
In the absence of a protocol, body weight was recorded upon physician request (28.2%) and according to the disease of the patient (14.1%). The main cited reason for such measurement was the need to adjust treatment (70.4%), followed by patients on dialysis (44.4%), resuscitation measures with large fluid volumes (33.3%), burn victims (7.4%), and organ donation and transplantation (22.2%).
Visual estimation of the measurements was the most frequent way of obtaining the data, and most centers used different sources in the course of patient admission. A total of 65.8% of the centers estimated weight and 64.8% estimated height. The next most important data source was the information provided by the patient or relatives (61.8% in the case of weight and 62.5% in the case of height). Measurement instruments were the third most frequent source (41.5% in the case of weight and 33% in the case of height).
A total of 30.7% of the centers lacked tools for measuring weight and 23.3% had no instruments for measuring height. The number of beds in the ICU was not related to the existence of weight (χ2=2.138; p=0.343) or height measuring instruments (χ2=0.99; p=0.61). Likewise, the existence of such instruments did not necessarily imply that they were actually used: 48.5% of the centers with weighing instruments and 68% of the centers with tools for measuring patient height did not use them. The most frequent tools for measuring weight were a scale-equipped bed (45.3%) and a scale-equipped lift (27.8%), while metric tapes were the most common instruments for measuring height (72.1%) (Table 1).
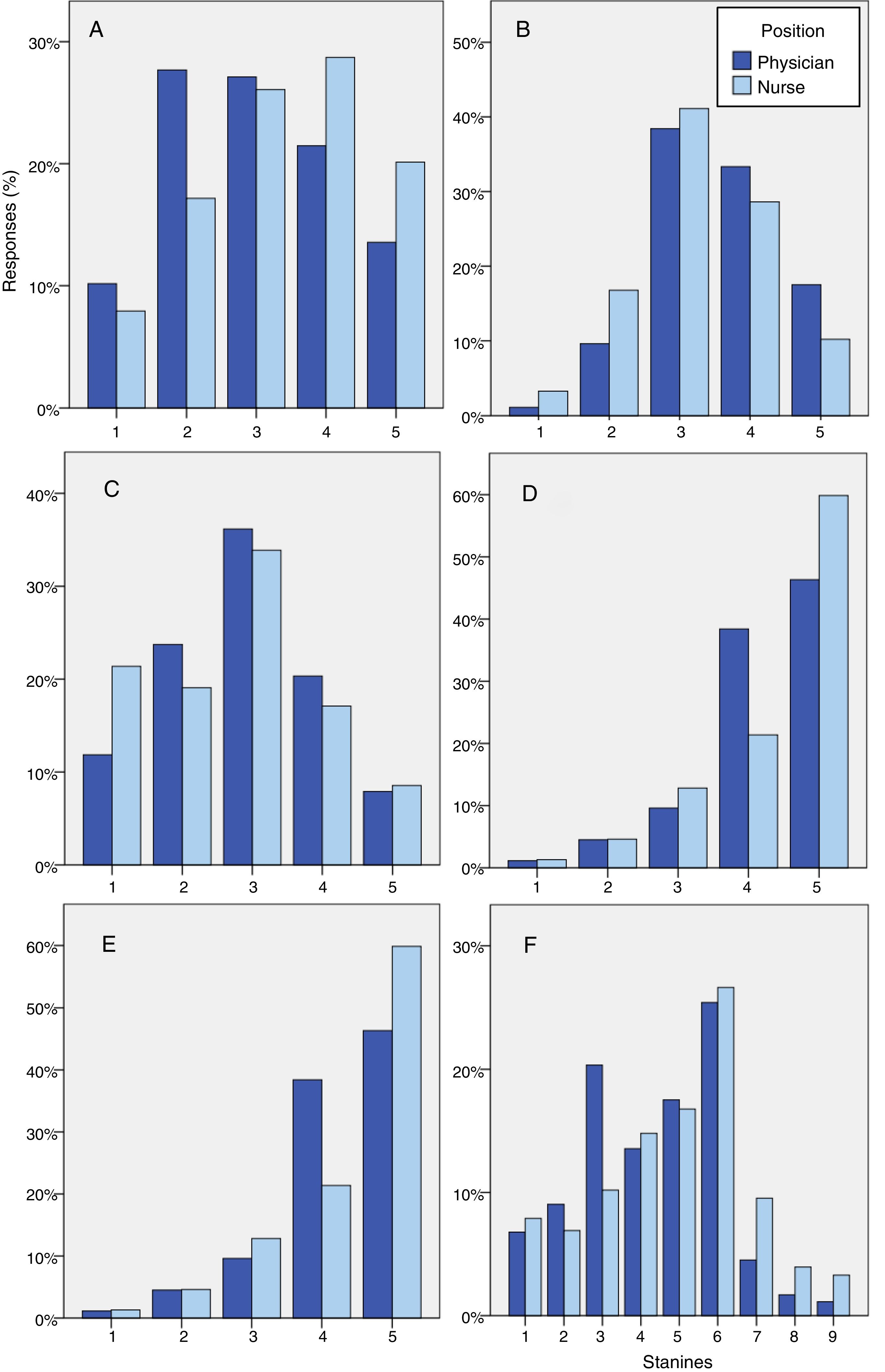
A total of 25.1% of the nurses and 37.8% of the physicians believed the measurements were not widely used in treatment decision making, and cumulative professional experience did not influence this opinion (Fig. 3A).
Tendency to use anthropometric measurements. Likert scale: (1) strongly disagree; (2) disagree; (3) neither agree nor disagree; (4) agree; and (5) strongly agree. (A) The measurement of weight and height is widely used in the ICU for treatment decision making. (B) There is a significant difference between the visually estimated values and the real measurements. (C) Knowing patient weight and height influences the total cost of admission to the ICU. (D) Having real instead of estimated measurements affects the safety of the patient admitted to the ICU. (E) Daily water balance recorded by the nursing chart is a reliable measure. (F) Grouping of answers B, C, D and E according to stanines.
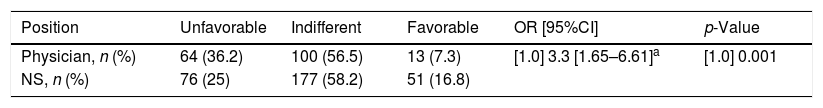
We explored the opinion of the participants regarding the reliability of the estimations, the impact of the measurements upon the cost of admission and on patient safety, and the reliability of the water balance chart in establishing real water weight gain (Fig. 3B–E). The possible answers reflected a tendency to obtain and use real measurements, indifference, or rejection. There were practically no differences in indifference toward the use of anthropometric measurements (58.2% of the NS and 56.5% of the physicians). In contrast, differences were noted in positive attitude or a tendency to use real measurements on the part of the NS (16.8% versus 7.7% among the physicians). The NS also showed less rejection (25%) than the physicians (36.2%) (OR 3.3, 95%CI: 1.7–6.6; p<0.001) (Table 2) (Fig. 3F). An unfavorable attitude was the most frequent finding among the participants with the longest professional experience (15.8 versus 10.6 years; p<0.001).
Tendency to obtain and use measurements.
| Position | Unfavorable | Indifferent | Favorable | OR [95%CI] | p-Value |
|---|---|---|---|---|---|
| Physician, n (%) | 64 (36.2) | 100 (56.5) | 13 (7.3) | [1.0] 3.3 [1.65–6.61]a | [1.0] 0.001 |
| NS, n (%) | 76 (25) | 177 (58.2) | 51 (16.8) |
The present study constitutes the largest survey published to date on anthropometry practices in the ICU and covers a large part of Spain. The study revealed scant protocolization of anthropometric measurements, deficient availability of measurement instruments, and scant acknowledgment among the professionals of the need for exact measurements of patient body weight and height.
The only previous experience attempting to assess anthropometry practices in the ICU involved a partial sample of 20 hospitals in the southern part of the United Kingdom, and consisted of a telephone interview of the physician or nurse of greatest experience available at the time of the call. Only 10% of the interviewees weighed their patients, while 75% recorded height. The study offered no explanation of the factors underlying this notorious difference in the prevalence of both measurements.4
Rational anthropometry use a priori seems to be essential in the ICU. Many studies have commented on the lack of precision of the measurement estimates made by health professionals in the ICU,1,5,6 with underestimates and overestimates of 33% and 45%, respectively, referred to body weight, and of 9% and 18% referred to height. Such lack of precision has also been described in pediatric7 and surgical patients,8 and in the emergency care setting.9 Despite these data, measurement estimation constitutes routine practice in up to 65% of the Spanish ICUs surveyed in the CAMIES study. No studies involving adequate methodology have examined the effect of error in estimating the measurements upon critically ill patients. Likewise, no studies have been made of how the precision of such estimates on the part of healthcare professionals may be influenced by factors such as professional experience or the age, gender and body mass index (BMI) of the patient, or the duration of hospital stay prior to admission to the ICU.
The literature advocates the use of adjusted weight particularly in obese patients and of ideal weight in the indexed calculation of hemodynamic parameters, for example. The relevance of knowing the real patient weight upon admission to the ICU is therefore questionable, though it is mandatory to have an exact measure of height in order to calculate the different derived weights. In this regard, the CAMIES study found 64.8% of the hospitals to estimate height, and a small error in this parameter is associated to a proportional variation in ideal weight. In the equation developed by Hamwi – one of the most widely used for calculating ideal weight – an error of only 1cm in mean height (160–180cm) causes the ideal weight to vary by more than 1kg.10 Such equations are moreover limited in situations of extreme height values. Other approaches to the calculation of ideal weight capable of improving the results for any height value have not been studied to date in the critical patient context.11
In a proprietary series of 362 critical patients with a normal BMI (18.5–24.8kg/m2), the calculation of ideal weight using the Hamwi formula yielded a greater percentage of tolerable estimates (error ≤5% with respect to real weight), specifically 53.8% versus 32.8% in the case of the estimates made by a physician (data not published).
The results of our survey reveal poor perception of the need to obtain real and exact measurements. We understand that by exploring the tendency to use measurements we have identified the main factor underlying the lack of anthropometry protocols: the unexpected proportion of both physicians and nurses that express indifference or rejection of the use of basic anthropometric measures. A notorious observation in this regard is the fact that rejection increased with the number of years of professional experience of the interviewee. This finding in itself merits an in-depth analysis, since it proves easy to regard certain information needed to design many treatments and to monitor critical patients as being important. In calculating water balance, the differential water balance charts do not seem to be sufficiently exact.12,13 In the calculation of hemodynamic indices, ideal weight and body surface area require precise height measurements. Mechanical ventilation volume in turn is initially adjusted to patient weight, but proves vital in the case of using low tidal volumes in respiratory distress,14 or in the post-cardiac surgery setting,15 where height is again necessary for calculating recommended weight (ideal weight in such cases). Both ideal and real body weight are relevant to the initial dosing of drugs that can be monitored on the basis of their plasma levels, and to the use of drug substances that obligatorily require adjustment to patient weight in order to avoid toxicity problems. Error in planned dosing appears to be more frequent with anticoagulants or sedating agents, and in patient groups with higher BMI values.16 For calculating the nutritional requirements in the absence of calorimetry, regression equations used to estimate energy expenditure constitute the most widely adopted approach. The weight used in most equation validation studies has been current weight, even if the patients had spent up to 27 days in the ICU – this implying that the selected weight value was very likely far different from the patient weight at the time of admission.17,18
In addition to experience, professional position also acts as a modifying factor of attitudes toward anthropometry. In this regard, nurses were less inclined to reject the need for such measurements, and recognized that they influence the treatment prescribed by the physicians. In contrast, physicians showed greater rejection than the nurses regarding the need to obtain the mentioned measurements, and moreover considered that the latter do not affect the treatments they prescribe. This lack of coherence possibly may be attributed to communication problems within the care team, as has already been addressed in Intensive Care Medicine,19 and constitutes a key area for improvement in order to implement anthropometry in the critically ill patient setting in Spain.
The most common arguments cited in the literature to explain the low acceptance of the recommendation to measure the weight and height of critical patients are the lack of measurement instruments and also the difficulties of obtaining measurements in patients with limited mobility and subjected to multiple instrumental procedures.
The main limitation of the CAMIES study is the 18.5% sample loss rate attributable to a lack of response despite three attempts to establish contact. Some of the surveyed hospitals are hospital complexes, with monographic ICUs and with anthropometry practices that may differ from those of the rest of the Units in the complex. Lastly, the CAMIES study depicts the situation of anthropometry in Spanish ICUs during the last trimester of 2013, and over the subsequent years the practices may have changed to some degree. Nevertheless, we consider that no scientific evidence or recommendations have emerged in Intensive Care Medicine that may have significantly modified the surveyed practices.
We consider it necessary to issue specific recommendations addressed to the main societies of Intensive Care Medicine in order to standardize the recording of measurements. The data obtained by the CAMIES study constitute a starting point and may facilitate the re-evaluation of a relevant aspect requiring improvement in future.
AuthorshipAll the authors participated in the literature review of the subject, the design of the study and in drafting of the manuscript.
Dr. Miguel Ángel García-Martínez developed the questionnaire and database, and performed the statistical analysis.
Tetyana Cherednichenko, Yolanda Hidalgo-Encinas and Ana Isabel Catalá-Espinosa carried out the computer-assisted telephone interviews.
Conflicts of interestThe authors declare that they have no conflicts of interest, and have received no financial support for carrying out the study.
Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.medine.2018.05.011.
Please cite this article as: García-Martínez MA, Cherednichenko T, Hidalgo Encinas Y, Catalá Espinosa AI, Arrascaeta Llanes A, Acosta Escribano JA. Calidad de la medición antropométrica en las Unidades de Medicina Intensiva españolas (Estudio CAMIES). Med Intensiva. 2018;42:329–336.