Acute appendicitis (AA) is one of the most common childhood surgical entities.1 Anamnesis, physical examination, blood tests and imaging provide an accurate diagnosis in 98% of patients. However, there is a lack of reliable instruments to predict evolution and anticipate complications.2,3 To this aim, recent studies using flow cytometry (FC) have been done to evaluate expression profile in patients with acute abdomen. The FC is a laboratory technique that allows to evaluate immune status or response of an individual based on marking leukocyte populations with monoclonal antibodies. One of the biomarkers that have demonstrated clinical applicability is CD64. Increasing of its density on surface is directly related to the intensity of stimulation received by inflammatory cytokines. It could be quantified by flow cytometry as mean fluorescence intensity (MFI).4 The main objective of this preliminary study was to describe the CD64 expression in pediatric patients after appendectomy and pediatric critical care unit (PICU) admission. For this purpose, the percentage of CD64-positive cells and the degree of expression (MFI) of CD-64 on monocytes (mCD64) and granulocytes (gCD64) were determined. Afterwards, it was analyzed its association with common biomarkers, the therapeutic care, the hospitalization time and complications.
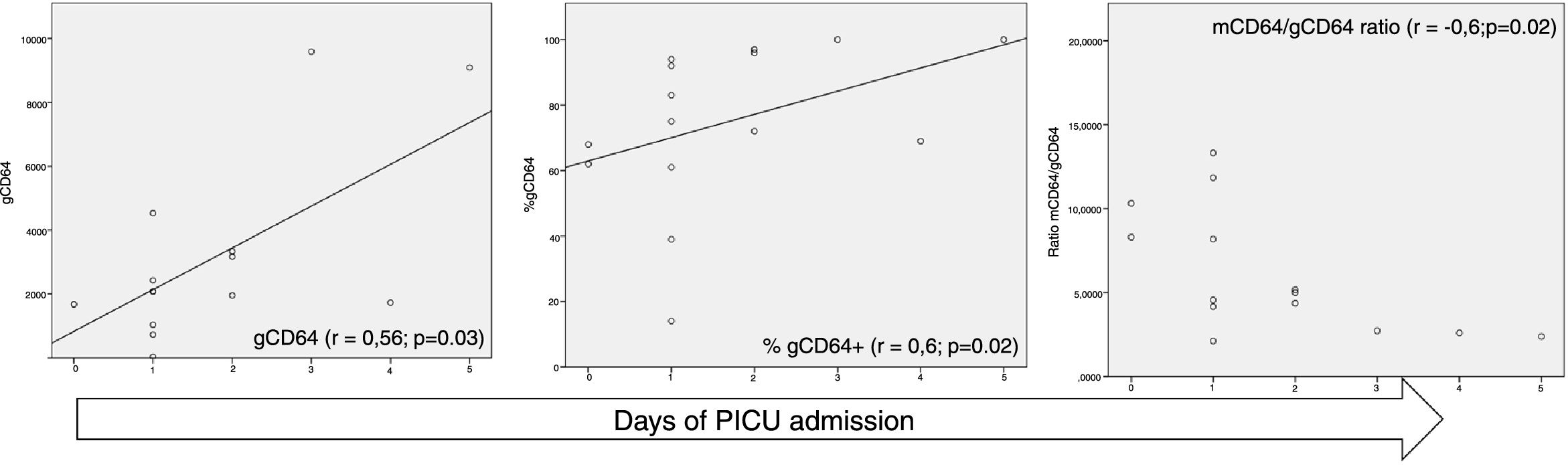
The study was prospectively conducted from November 2016 to January 2017. Peripheral blood samples were extracted after parents or legal guardians consent at PICU admission. The PICU admission was done by surgeon criteria and not protocoled. Samples were collected at first 24h after surgery in sterile EDTA at room temperature or refrigerated at 4°C, used for CD45+ cells marking and analyzed by flow cytometry in a time period shorter than 24h. Fifteen patients (6 female and 9 male) were recruited with a median age 7.3±4.2 years. Median PICU stay was 1±1.4 days with a median hospitalization of 5.5±4.4 days. The CD64 expression on neutrophils and monocytes were mCD64 median MFI of 16,366±6762 and gCD64 median MFI of 2071±2791.8 with a percentage of CD64+ granulocytes (%gCD64+) 75±24.4% and a mCD64/gCD64 ratio of 5±1.7. Non-parametric test were applied. Time of stay in the PICU correlated with gCD64 (r=0.56; p=0.03), % gCD64+ (r=0.6; p=0.02), and mCD64/gCD64 ratio (r=−0.6; p=0.02) (Fig. 1). Also the hospitalization time showed correlation with mCD64/gCD64 ratio (r=0.5; p=0.04). The use of nasogastric tube, as an expression of bowel movement, was correlated with gCD64 (r=0.5; p=0.03) and % gCD64+ (r=0.5; p=0.05). Finally, Granulocytes of patients with parenteral nutrition necessity (PNT) showed greater positivity for CD64 (% gCD64+ – TPN 90±14 vs not TPN 68±27, p=0.045). Among the classical parameters, none of them showed correlation or statistically significant association with the clinical data except for the C-reactive protein (CRP). At PICU admission leukocytes, C reactive protein and procalcitonin were obtained and there was observed a positive correlation with no signification with CD64 expression.
Spearman correlation between CD64 expression and days of PICU stay. %gCD64 is the percentage of CD64-positive cells, gCD64 is the CD64 degree of expression in granulocytes by mean fluorescence intensity and mCD64 is the CD64 degree of expression in monocytes by mean fluorescence intensity.
This pilot work describes, for the first time, the CD64 expression on peripheral blood monocytes and granulocytes from pediatric patients after appendectomy.5 Also, this is the first study that tries to correlate clinical and evolution data from acute appendicitis pediatric patients with CD64 values obtained by FC.
As said the FC interpretation may provide unique information letting know immunological changes in real-time. These properties would help to substantiate diagnostic suspicion, anticipate the evolution and modify therapeutic attitudes. In this study, CD64 expression in terms on granulocyte of MFI is lower, as our group has previously seen,6 than in other inflammatory and infectious contexts.7 These results could have two explanation. On the one hand, the AA is, with exceptions, a localized infection in which the systemic expression through CD64 quantification on granulocytes and monocytes in peripheral blood, may be underestimated. In this process, participating granulocytes would not be predominant in the bloodstream. At the same time, in this study, determination by FC was performed after surgery, so after having removed the inflammatory insult and having received, at least, one dose of antibiotic therapy. It is well known that CD64 reduces its expression once received appropriate antibiotic therapy. In the same way, it is known that the half-life of a human granulocyte in peripheral blood is 6h.8 Thus, in our experiment, leukocyte populations studied might not be under the same inflammatory context than those present at the onset of AA underestimating the value of MFI.5,6
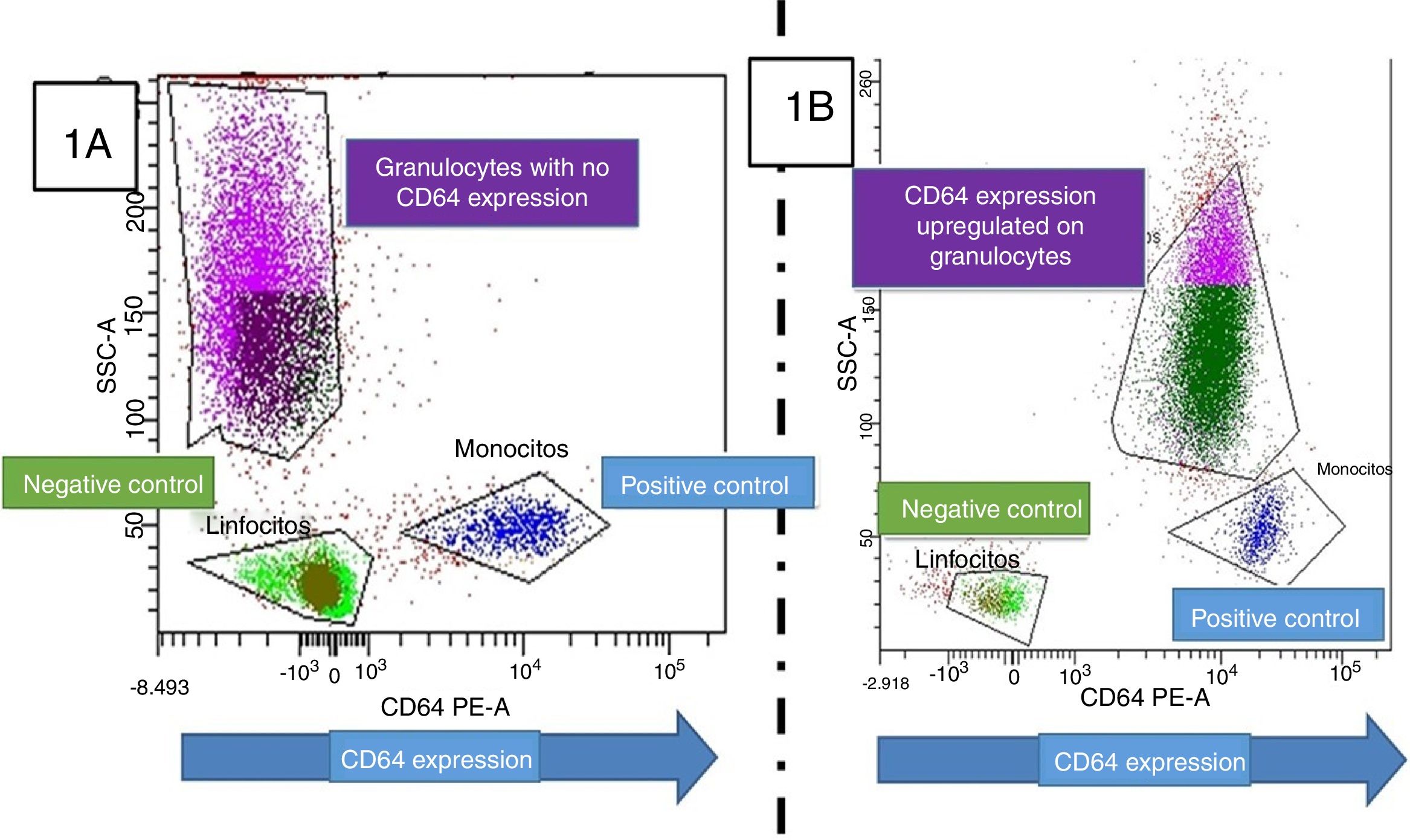
In order to minimize the potential effect of this confusion factor, CD64 expression ratio (mCD64/gCD64) was studied knowing that the presence of CD64 on granulocytes should be null in case of no inflammation (Fig. 2). Changes in this ratio could be used to quantify upregulation of this molecule in granulocytes. Our study showed that mCD64/gCD64 ratio inversely correlated with total hospital stay. Also, and with the same objective, CD64+ granulocytes percentage was quantified. Since baseline percentage of positive CD64 granulocytes must be zero, any higher value would indicate activation. In the studied population CD64 positivity existed in all cases, being always superior to 45% in granulocytes. As said, the percentage of CD64+ granulocytes was higher in patients with prolonged PICU stay, days of hospital admission and need of PNT. This correlation with the need of PNT, is of great interest due to its novelty.2
(A) CD64 staining on granulocytes, monocytes and lymphocytes in a healthy child. From left to right the expression on them can be observed. CD64 is expressed in monocytes but not in lymphocytes and neutrophils. (B) CD64 staining in a child with bacterial infection, the granulocytes are CD64 positive (displaced from left to right) as a consequence on CD64 upregulation. The lymphocytes act as an internal negative control.
This study presents limitations. It was done in a single center, with a small number of patients and without strictly defined PICU admission criteria. At the same time, it cannot be assumed that CD64 is the only responsible for the clinical course in the case of AA patients. Their values should be compared with traditional biomarkers in larger samples. This aspect could also be attenuated with the inclusion of other cell surface markers in further analysis. Finally, just a single blood sample was obtained after the surgery. These values should be compared to previous surgery data and/or later samples. The study about CD64 dynamic variation should be included in future studies.
As conclusion, in our preliminary work, the expression of CD64 on granulocytes at PICU admission correlated with the hospitalization time and need of nasogastric tube and non-enteral nutrition. Based on these findings, it seems of interest to continue the study of CD64 in order to provide dynamic and reliable information about the actual utility of the flow cytometry in these patients.