We evaluate the impact of a web-based collaborative system on the referral of possible organ donors from outside of the intensive care unit (ICU).
Study designCohort prospective study.
SettingsUniversity hospital.
Patients and interventionIn 2015 a virtual collaborative system using a cross-platform instant messaging application replaced the previous 2014 protocol for the referral of patients outside of the ICU with a severe brain injury in whom all treatment options were deemed futile by the attending team to the donor coordination (DC). Once the DC evaluated the medical suitability and likelihood of progression to brain death (BD), the option of intensive care to facilitate organ donation (ICOD) was offered to the patient's relatives. This included admission to the ICU and elective non-therapeutic ventilation (ENTV), where appropriate.
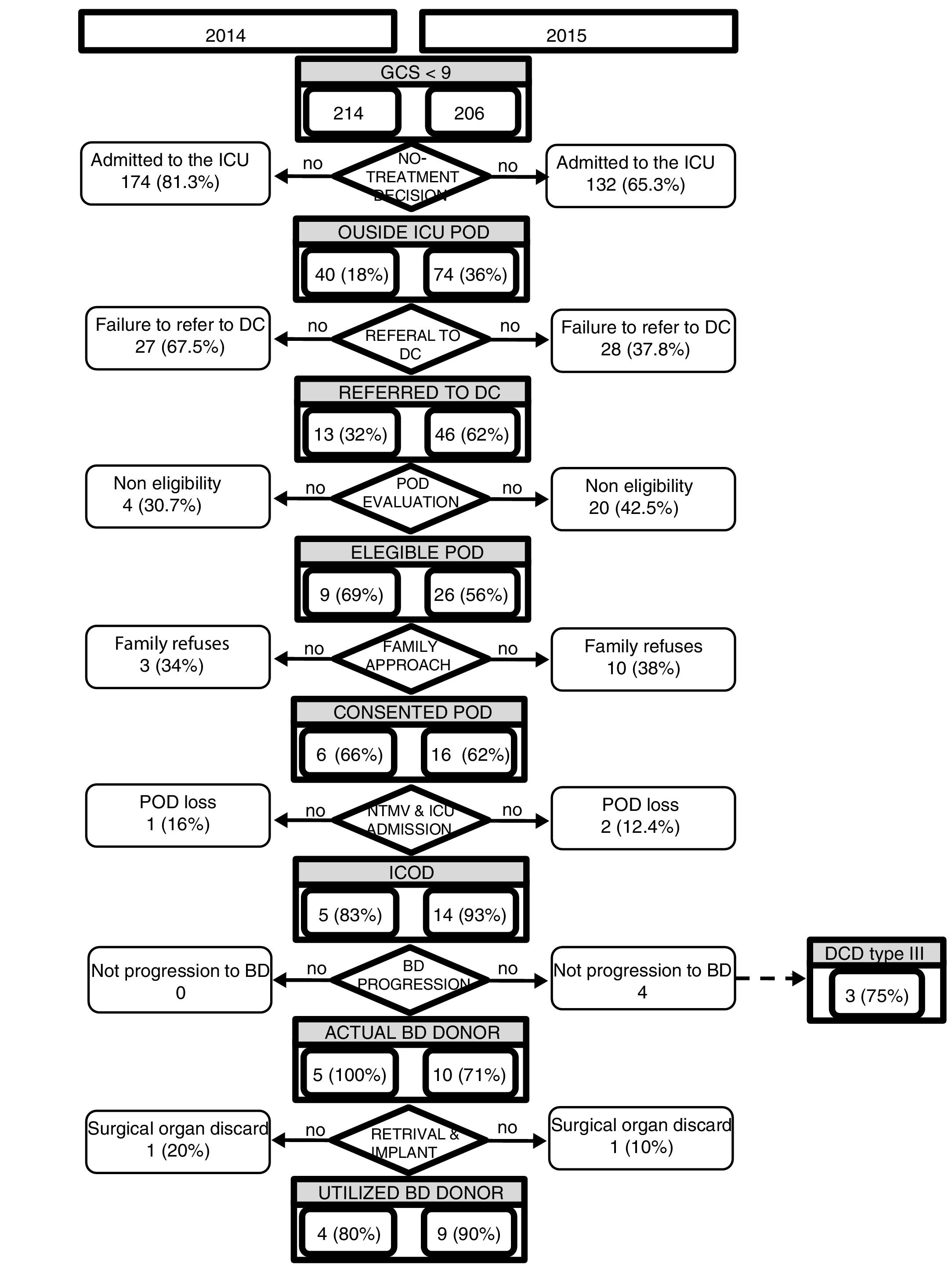
ResultsA two-fold increase of referrals was noted in 2015 [n=46/74; (62%)] compared to 2014 [n=13/40; (32%)]; p<0.05. Patients were mostly referred from the stroke unit (58.6%) in 2015 and from the emergency department (69.2%) in 2014 (p<0.01). Twenty (2015: 42.5%) and 4 (2014: 30.7%) patients were discarded as donors mostly due to medical unsuitability. Family accepted donation in 16 (2015: 62%) and 6 (2014: 66%) cases, all admitted to the ICU and 10 (2015: 62.5%) and 3 (50%) being subject to ENTV. Ten (2015: 66.6%) and 5 (2014: 83.3%) patients progressed to BD, 60.5±20.2 and 44.4±12.2h after referral respectively. Nine (2015) and 4 (2014) of these patients became utilized donors, representing 29.0% (2015) and 13.0% (2014) of the BD donors in the hospital during the study period (p<0.05).
ConclusionThe implementation of a virtual community doubled the number of patients whose families were presented with the option of donation prior to their death.
Evaluación del impacto de un sistema de colaboración por red en la detección de posibles donantes fuera de la unidad de cuidados intensivos (UCI).
DiseñoEstudio prospectivo de cohortes.
ÁmbitoHospital universitario.
Pacientes e intervenciónEn 2015 se creó una comunidad virtual mediante mensajería multiplataforma que reemplazó al anterior sistema de notificación (2014) al coordinador de trasplantes (CT) de aquellos pacientes fuera de la UCI con lesiones neurológicas graves en los que el equipo tratante había considerado fútil cualquier opción terapéutica. Tras determinar la ausencia de contraindicaciones médicas y la probabilidad de progresión a muerte encefálica (ME) el CT ofrecía a los familiares la opción de cuidados intensivos orientados a la donación incluyendo el ingreso en la UCI y la ventilación electiva no terapéutica (VENT).
ResultadosEn 2015 (n=46/74; 62%) se dobló el número de notificaciones con respecto a 2014 (n=13/40; 32%); p<0,05. Los pacientes procedían mayoritariamente de la unidad de ictus (2015: 58,6%) y urgencias (2014: 69,2%); p<0,01. Un total de 20 (2015: 42,5%) y 4 (2014: 30,7%) pacientes se desestimaron como donantes por contraindicación médica. Los familiares aceptaron la donación en 16 (2015: 62%) y 6 (2014: 66%) casos; todos ingresaron en la UCI y 10 (2015: 62,5%) y 3 (50%) de ellos recibieron VENT. Diez (2015: 66,6%) y 5 (2014: 83,3%) pacientes progresaron a ME, 60,5±20,2 y 44,4±12,2h después de su notificación, respectivamente. Nueve (2015) y 4 (2014) de estos pacientes fueron donantes utilizados, representando el 29,0% (2015) y el 13,0% (2014) de los donantes en ME (p<0,05).
ConclusiónLa implementación de una comunidad virtual duplicó el número de pacientes cuyas familias recibieron la opción de donación antes de su muerte.
Organ and tissue transplantation is an increasingly common procedure worldwide, being the only treatment for some end-stage organ diseases as well as improving the quality of life of many tissue recipients.1–5 Its acceptance by society and the health care community is rising, as reflected by the inclusion of the donation process as part of the end-of-life-care of the critical patient in several guidelines.6,7 Nonetheless, the disparity between patients awaiting transplantable organs and the availability of donor organs continues to increase,8–10 making necessary the optimization of old strategies and the implementation of new ones aimed at enhancing the detection of all possible organ donors.11
Early detection and referral of possible organ donors, defined as patients with a severe brain injury (GCS<9) and apparently medically suitable for donation,12 to the donor coordination (DC), has shown to increase the number of actual donors and improve the quality of transplantable organs.1,13,14 In fact there have been many national15 and supranational9 initiatives to implement strategies aimed at increasing the detection of possible donors.
Communication technologies have proved useful in different teamwork scenarios, enhancing multidirectional communication and facilitating the decision-making process.16 These features make them ideal tools for the referral of possible donors from outside the intensive care unit (ICU), allowing physicians responsible for the patient the possibility to contact the DC and receive real-time feedback, especially in large hospitals and complex infrastructures where communication is a difficult task.
To our knowledge, strategies using virtual messaging platforms as a tool to improve the detection of possible donors have not been previously reported.
We evaluate the impact of the creation of a virtual collaborative community for the referral of possible donors from outside the ICU at a University hospital.
Patients and methodsProspective analysis comparing two cohorts before and after the implementation of a new referral strategy for possible donors located outside the ICU.
Valld’Hebrón University Hospital (VHUH) Barcelona is a third level university health-care complex organized in three independent areas: Trauma Hospital, Maternity-Pediatric Hospital and General Area. It is one of the largest hospitals in the region attending a 450,000 population of the Barcelona metropolitan area with 1072 beds (172 dedicated to the care of critical care patients) and 7177 health care professionals. VHUH is an authorized transplant center since 1988 and accounts for active pediatric heart, lung, liver and kidney as well as kidney, lung and liver adult transplant programs, and is currently one of the leading transplant hospitals in Europe registering 31 and 47 deceased donors in 2014 and 2015 respectively.17
VHUH DC team was composed of two full-time senior donor coordinators (intensive care specialists), 1 nurse, and 2 administrative personnel as well as 5 trained medical students18 at the time of the study. The DC team is in charge of the organ donation and procurement process on a 24/7 schedule, consisting of a proactive identification of all possible organ and tissue donors admitted to the hospital, evaluation of their medical eligibility, approaching the family (and coroner if necessary) as well as guaranteeing their appropriate management while organizing the logistics required for the organ/tissue retrieval. They are also responsible for the development and implementation of strategies directed at improving the number and quality of organ donors as well as optimizing the management and outcome of the recipients. The DC team takes care of the promotion of all education, training and research activities around organ donation and transplantation in the hospital and its influence area.
Donor detection and referral is one of the critical issues for the success of any transplant program. For that reason and with the aim of covering such a large and complex infrastructure as is VHUH, several donor detection programs have been put in place by the DC. All hospital deaths are notified by hospital porters to the DC for their evaluation as tissue donors and retrospectively identify non-referred possible organ donors. Since 2009 all patients admitted to the hospital presenting with a severe brain injury with a GCS<9, are prospectively followed until death or discharge (PR(AG)11/2009) in order to detect and evaluate all possible organ and tissue(s) donors likely to evolve to brain death (BD) or in whom the decision has been made to withdraw life-sustaining therapy (WLST) on the grounds of futility of further care. The follow up of these patients is performed by the DC that attends the daily rounds with the critical care physicians in all of the six ICUs of the complex or through the implementation of different referral strategies for those donors located outside the ICUs.
Before 2015, referral of all out-of-ICU patients presenting with a GCS<9 and a severe brain injury leaned on a phone call to the DC by the attending clinician based on their own criteria regarding patient's medical suitability for organ donation and the likelihood of progression to BD. The DC would proceed to confirm donor suitability and approach the patient's relatives to offer the possibility of intensive care to facilitate organ donation (ICOD). Informative posters and educational sessions were delivered to neurologists and emergency care professionals, as those responsible for the initial management of neurocritical patients before admission to the ICU. All hospital deaths were reviewed on a daily basis with subsequent feedback to the physicians responsible for the non-referred cases.
In 2015 Using a Plan-Do-Study-Act methodology19 within the ACCORD project,9 an intervention was devised to increase efficiency in the identification and referral of possible donors outside of the ICU. This new intervention was accepted by the Ethics committee of our center (PR(AG)13/2013).
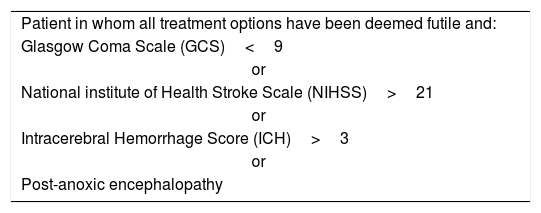
In 2015, 90% of the specialists playing a key role in the management of possible donors outside the ICU were voluntarily included in a virtual collaborative group using an instant messaging application (WhatsApp®) in order to refer to the DC all patients presenting with GCS<9 and who fulfilled any of the established by consensus criteria (Table 1). Once the DC has evaluated the medical suitability and likelihood of progression to BD, he/she would discuss donation opportunities with families of possible donors, explaining the need for ICOD, inclusive of elective non-therapeutic ventilation (ENTV) where appropriate. Relatives were informed of the ICOD procedure to follow after admission to ICU including the establishment of a neurological observation period of approximately 72h to allow the evaluation to be completed and for the progression of BD. They were also informed about the possible scenarios that may occur, including the finding of a medical condition that would preclude donation during the evaluation or the reconsideration of donation by the patient's family, in which case WLST should be considered to avoid futile treatment. DC would comment with the family that the option of DCD donation could be considered at anytime if they wish to shorten the observation period or once it has expired.
All members of the team would receive through the same communication system immediate feedback of the results of the possible donor clinical evaluation and the final outcome. To preserve the patient confidentiality, no personal information was reported through the virtual platform.
We report the impact of the strategy commenced in 2015 by comparing the referral of possible donors throughout that year with that in the previous one (2014). For the statistical analysis, SPSS 15.0 (SPSS Inc., Chicago, IL, USA) program was used. Continuous data are reported as mean and standard deviation or median and interquartile range where appropriate, and categorical data as numbers and percentages. Categorical variables underwent univariate analysis using Pearson's Chi-squared test and Fisher's test in case of lower frequencies than expected. Continuous variables were compared with the Student t test (normal distribution) and U-Mann–Whitney test, considering a p<0.05 value as statistically significant.
ResultsDuring 2015 a total of 206 patients presented a GCS<9 due to a severe brain injury during their hospital admission. Seventy-four (36%) were never admitted to the ICU. A similar number of patients (n=214) was reported in 2014, with 40 (18%) outside of the ICU.
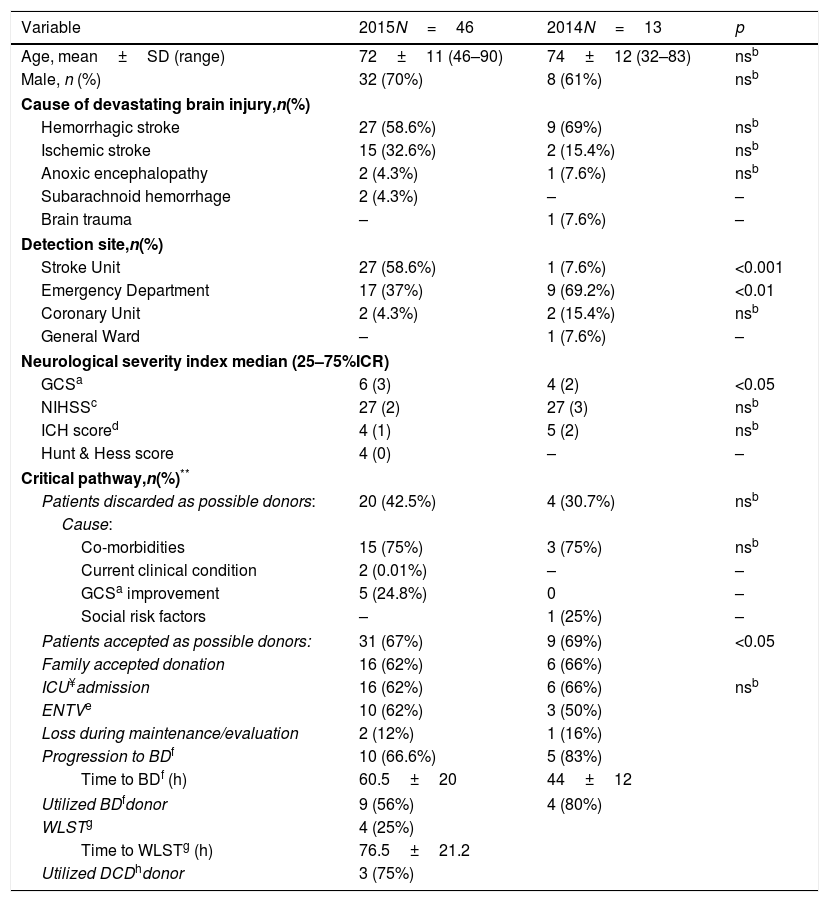
A 2-fold increase in the referral of possible donors from outside of the ICU was observed in 2015 [n=46/74; (62%)] compared with the previous year [n=13/40; (32%)], p<0.05 (Fig. 1). Patients in 2015 were referred mostly from the stroke unit (59%), while the emergency department (69%) was the most common referral site in 2014. There were no differences in mean age, gender and cause of the devastating brain injury of possible organ donors between both periods (Table 2).
Demographics and clinical data of possible donors referred to the donor coordination from outside of the ICU in 2015 and 2014.
| Variable | 2015N=46 | 2014N=13 | p |
|---|---|---|---|
| Age, mean±SD (range) | 72±11 (46–90) | 74±12 (32–83) | nsb |
| Male, n (%) | 32 (70%) | 8 (61%) | nsb |
| Cause of devastating brain injury,n(%) | |||
| Hemorrhagic stroke | 27 (58.6%) | 9 (69%) | nsb |
| Ischemic stroke | 15 (32.6%) | 2 (15.4%) | nsb |
| Anoxic encephalopathy | 2 (4.3%) | 1 (7.6%) | nsb |
| Subarachnoid hemorrhage | 2 (4.3%) | – | – |
| Brain trauma | – | 1 (7.6%) | – |
| Detection site,n(%) | |||
| Stroke Unit | 27 (58.6%) | 1 (7.6%) | <0.001 |
| Emergency Department | 17 (37%) | 9 (69.2%) | <0.01 |
| Coronary Unit | 2 (4.3%) | 2 (15.4%) | nsb |
| General Ward | – | 1 (7.6%) | – |
| Neurological severity index median (25–75%ICR) | |||
| GCSa | 6 (3) | 4 (2) | <0.05 |
| NIHSSc | 27 (2) | 27 (3) | nsb |
| ICH scored | 4 (1) | 5 (2) | nsb |
| Hunt & Hess score | 4 (0) | – | – |
| Critical pathway,n(%)** | |||
| Patients discarded as possible donors: | 20 (42.5%) | 4 (30.7%) | nsb |
| Cause: | |||
| Co-morbidities | 15 (75%) | 3 (75%) | nsb |
| Current clinical condition | 2 (0.01%) | – | – |
| GCSa improvement | 5 (24.8%) | 0 | – |
| Social risk factors | – | 1 (25%) | – |
| Patients accepted as possible donors: | 31 (67%) | 9 (69%) | <0.05 |
| Family accepted donation | 16 (62%) | 6 (66%) | |
| ICU¥admission | 16 (62%) | 6 (66%) | nsb |
| ENTVe | 10 (62%) | 3 (50%) | |
| Loss during maintenance/evaluation | 2 (12%) | 1 (16%) | |
| Progression to BDf | 10 (66.6%) | 5 (83%) | |
| Time to BDf (h) | 60.5±20 | 44±12 | |
| Utilized BDfdonor | 9 (56%) | 4 (80%) | |
| WLSTg | 4 (25%) | ||
| Time to WLSTg (h) | 76.5±21.2 | ||
| Utilized DCDhdonor | 3 (75%) | ||
Median Glasgow Coma score (GCS)20 at referral was significantly higher in 2015 when compared with that of patients referred during the previous year. However similar Intracerebral Hemorrhage Score – ICH21 and National Institute of Health Stroke Scale – NIHSS22,23 were reported in patients referred during both periods.
In 2015 a total 20 referred patients (43%) were excluded as possible donors, and 4 (31%) of the referred patients were discarded in 2014. Medical unsuitability was the main reason for exclusion accounting for one third of all referred patients in both periods (32% (n=15) in 2015 vs 33% (n=3) in 2014) Five patients were excluded by the DC from the donation process due to the poor likelihood of progression to BD in 2015 while none of the referred patients in 2014 were discarded for this reason.
Family accepted donation in 16 (62%) and 6 (66%) cases in 2015 and 2014 respectively. ENTV was used in 10 (62.5%) and 3 (50%) possible donors. All consented patients (14 in 2015 and 5 in 2014) were subject to ICOD. Two (12%) patients in 2015 and 1 (16%) in 2014 were lost as donors during the process due to maintenance problems.
Ten patients (71%) in 2015 and 5 (100%) in the 2014 group finally progressed to BD at 60.5±20.2 and 44.4±12.2h after referral (p<0.05) respectively becoming actual donors. Nine (90%) and 4 (80%) of them became utilized donors, representing 29% and 13% of the total BD donors reported in our center in 2015 and 2014 respectively (p<0.05). One donor was lost in each period during the surgical retrieval final evaluation process (Fig. 1).
The implementation in 2015 of a program of donation after controlled circulatory death (DCD) allowed converting 3 of the 4 patients who did not progress to BD into actual DCD donors a mean of 73.0±15.1h after referral.
DiscussionTo the best of our knowledge, this is the first report assessing the impact of a cross-platform instant messaging application on the referral of possible donors from outside of the ICU.
In our experience the incorporation of a virtual collaborative platform as a communication tool and the definition of clear and concise criteria for referral, doubled the rate of patients referred from outside of the ICU and who were offered the possibility of organ donation as part of their end-of-life care. Thisnew approach increased by two-fold the number of possible donors referred from outside the ICU generating one of every three BD donors in our center and that represented a total of 11 donors/pmp for the reference area. Such achievement was obtainedwithout requiring complex and expensive investment of resources, using already existing simple-to-use technology.
The use of this multiplatform tool also facilitated multidirectional communication among DC and specialists involved in detection and initial management of possible donors outside of the ICU, promoting real time feedback and training to all members of the team.
The Madrid resolution on organ donation and transplantation highlighted the need to develop strategies directed to increase organ availability and achieve self-sufficiency in transplantation.24 However, despite all the efforts to reduce the gap between patients waiting for transplantable organs and donors, it continues to increase.
Usually most possible donors are managed in the ICU by critical care specialists trained in their detection and where well-established referral protocols are in place.25 However, as thepopulation ages, the accumulation of chronic diseases decreases the chance for their admission to ICUs in case of suffering a devastating brain injury. These patients are initially managed in the emergency departments and admitted to neurology or internal medicine wards where theattending physician, not familiar with the organ donor procurement process, will most likely not consider, or incorrectly discard them as donors, precluding these patients from being offered the chance to donate their organs and tissues as part of their end-of life care plan.26 According to a recently published study performed in sixty-eight Spanish hospitals authorized for organ procurement, 36% of possible donors dying outside of the ICU were not reported to the DC at any time during their evolutionary course. In over one-half of the cases the reason for not notifying the DC was failure by the treating physician to identify the patient as a possible organ donor, followed in order of frequency by the existence of medical contraindications to donation.27 In order to optimize donor detection and referral from outside the ICU, new models of cooperation and education should be developed. It is necessary to engage all staff directly or indirectly involved in the initial management of possible donors outside the ICU, since they will act as the key detection professional in these scenarios.28 Training and education should be provided on a regular basis and recognition and support should be given to their detection task. It is also important to develop new, cost/effective and innovative strategies directed to enhance communication between clinicians managing possible donors located outside the ICU and DC teams.29
Social networks currently play an important role in daily life, proposing new interactive communication models and enabling the multidirectional interchange of information in real time between persons and groups from different locations; these characteristics make them a useful tool in multidisciplinary work groups where a continuous high flux of multidirectional communication in real time is needed in settings where verbal communication is difficult, such as in hospitals with a high number of beds and complex structures.
The use of an inexpensive, widely available, simple-to-use instant messaging application significantly improved the number of possible donors detected outside of the ICU, contributing to early contact with DC and allowing the possibility to establish a multidirectional communication among all professional teams involved in referral, evaluation and management of possible donors and the DC team. It also promoted collective learning of all the team through the provision of immediate feedback of real cases, enabling all participants to see the impact of their contribution on the final outcome, allowing the opportunity for organ and tissue donation. This is in our opinion the main reason for the success of the program.
Although all interviews with possible donors’ relatives were carried out by the DC (with specific training in family approach), acceptance rate for ICOD was lower than that achieved for BD organ donation during the same period (76.2% in 2014 and 85% in 2015). Authors believe that the fact that many of those interviews were performed in places where privacy and tranquility were limited by the architectural and logistical characteristics of the center may explain this finding. Moreover, the inevitably short time frame period between bad prognosis and WSLT communication and ICOD interview may add to the families‘difficulties when taking such decisions.
Despite professionals in charge of detection and referral of possible donors outside the ICU being the same during the study period, the implementation of the new strategy led to an increase of patients referred from the stroke units during 2015, as opposed to 2014 where emergency was the main site of referral. The improvement of communication among all professionals involved in the detection, referral and evaluation process could have help to expand the detection activity to other areas of the study center.
Our study has some limitations. First, its unicentric nature may limit the application of our results to centers of different human and structural characteristics. Similarly, commitment with the donation activity which is indirectly reflected by the ICU admission criteria policies may vary among centers. HUVH is a tertiary center with a clear pro-donation philosophy and transplantation represents a big proportion of our daily activity. However, we must say that the implementation of this strategy represented only an increase of 0.89% in the ICU admission and the mean ICU length of stay was <60.5h in patients who progressed to BD and 73h in those who were donors in DCD leading to a 25% increase of the utilized donors.
Second, despite encryption of shared information and the limitation of the shared patient data in order to protect identities, the use of a commercial messaging platform might affect patient confidentiality.30 The use of customized or commercial platforms with higher levels of security could guarantee the preservation of patient confidentiality.
Finally, detection and referral of patients with severe brain injury in early stages may increase the risk of including possible donors who finally would not progress to BD; in our study patients referred in 2015 presented a higher GCS than the ones referred during 2014 and progressed to BD a mean of 16h later than the former ones. Furthermore, while in 2014 all referred possible donors progressed to BD, five possible donors in 2015 did not. The implementation of a DCD program in 2015 allowed the wish to donate of those who did not progress to BD to be fulfilled. Criteria used to refer possible donors to DC should be regularly reviewed according to the clinical31 and neuromonitoring32,33 evidence available in order to fine tune their predictive power.
The probability of not progressing to BD in possible donor candidates is a risk that should be taken into account and must be clearly transmitted to the patients’ relatives before ICU admission to facilitate donation. In these scenarios it is advisable to define a time frame of neurological observation after which the WLST should be considered to avoid futile treatment. A neurological observation period of 72h was proposed to relatives, based on the evidence reported by Escudero et al.34 describing the clinical characteristics of patients who were diagnosed of BD in 42 Spanish ICUs. Relatives should be informed that the donation process can be interrupted if during the evaluation a medical contraindication is found,35 at anytime according to their wish, or once the period agreed has expired. In the latter two scenarios, the possibility of DCD can be discussed with relatives.
In conclusion, creation of clear referral criteria and the use of an inexpensive, widely available and simple-to-use instant messaging application may have contributed to the increase in the number of possible donors detected and referred from outside the ICU, doubling the number of patients in whom the option of donation was offered as part of their end-of-life care, and generating one out of three BD donors in our center. This web-service tool also improved multidirectional communication among all professional teams involved in possible donor initial management, detection and referral, promoting collective learning through the provision of immediate feedback.
Author contributionAll authors discussed the results and contributed equally to this manuscript.
Conflict of interestThe authors declare no conflict of interest.