When the lung parenchyma is exposed to cyclic stress, lung compliance inevitably begins to decrease.1 Respiratory rates higher than 25 per minute, generate a higher energy transfer,2 which leads to a higher heterogeneous strain mainly due to a lower lung resilience capacity.3 High respiratory rates produce hypocapnia and respiratory alkalosis, but also cause direct injury through chemical effects as a consequence of the alteration of mechanoreception reflexes, which is ultimately associated with greater morbidity and mortality.4
If the oscillatory frequency of the lung tissue exceeds the maximum limit of its elastic behavior, the heterogeneous variability of the strain5 and the affectation in the capacity of the parenchyma to assimilate the transmitted energy (stress), will result in a decrease of the tissue resistance with a tendency to zero, which will lead to the appearance of micro ruptures of the pulmonary cytoskeleton.6
The recent study published by the Mechanical Power Day [MPD] group,7 by applying the formula proposed by Gattinoni et al.,8 showed a mean mechanical power (MP) of 19.20 J/min (SD 8.44) for patients on pressure-controlled ventilation (PC-CMVs) and 16.01 J/min (SD 6.88) for those on volume-controlled ventilation (VC-CMVs). However, the researchers propose an interesting formula for the calculation of MP, using strain and strain-rate subrogates, based on solid concepts of materials engineering and thermodynamics, which have already been used in other clinical studies.9 A relevant point is the time factor, which is also implicit in the subrogation of the strain-rate according to the formula proposed by the MPD group. In VC-CMVs, the strain-rate corresponds to Flow ratio/PEEP and DP to strain; whereas in PC-CMVs, the strain-rate corresponds to subrogated strain (ETv/PEEP)/inspiratory time.
The authors reported a mean of 17 breaths per minute in both groups (PC-CMVs and VC-CMVs), with no significant difference (Welch, p = 0.12).
We performed an analysis post hoc of the MPD using frequentist statistics to evaluate the behavior of the respiratory rate, analyzing the variables that are part of the MP equation proposed by González-Castro et al.,7 of the multicenter and international cross-sectional cohort.7 We decided to dichotomize the sample between those with high-energy MP (>17 J/min) and compare them with those with low-energy MP (<17 J/min), as supported by current evidence.8
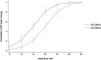
Bivariate analysis showed that respiratory rate behaved as a risk factor for high-energy MP, regardless of the ventilatory mode used (PC-CMVs; OR 1.56, 95% CI: 1.32–1.84; p < 0.01/VC-CMVs; OR 1.46; 95% CI: 1.29–1.65; p < 0.02). In the multivariate analysis [Table 1], although PEEP was the variable that showed the greatest association with risk of high-energy MP, the behavior of respiratory rate was very similar in both ventilatory modes, showing a greater probability of association with high-energy MP both in those patients ventilated in PC-CMVs (OR 1.96; 95% CI: 1.50–2.55; p < 0.01), as well as in those on VC-CMVs (OR 1.41; 95% CI: 1.23–1.62; p < 0.01) [Table 1 and Fig. 1].
Multivariate analysis of the MP according to the model proposed by the MPD group.
| Variable | PC-CMVs | VC-CMVs | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Strain subrogate | 1.09 | 0.97–1.2 | 0.15 | 1.20 | 1.06–1.35 | <0,01 |
| PEEP | 4.58 | 1.24–16.94 | <0.05 | 1.89 | 1.40–2.56 | <0.01 |
| Strain-rate subrogate | 1.02 | 0.97–1.06 | 0.44 | 1.29 | 1.05–1.58 | <0.05 |
| Respiratory rate | 2.08 | 1.52–2.84 | <0.01 | 1.41 | 1.23–1.62 | <0.01 |
| Expiratory tidal volume | 1.01 | 0.99–1.03 | 0.39 | – | – | – |
| Inspiratory time | 1.96 | 0.03–148.95 | 0.76 | |||
OR: odds ratio, CI: confidence interval.
For the PC-CMVs model, the total variance inflation factor (VIF) was 5.25, with strain subrogate being the variable with the highest value of concern, computed at the maximum limit of tolerance. For the VC-CMVs model, the VIF was 1.33, and there was no value of concern.
In PC-CMVs, for a respiratory rate >20 bpm, an ROC of 81% was obtained, corresponding to a specificity of 91.43% [LR(+) 5.02]. Likewise, in VC-CMVs, for the same respiratory rate range, an ROC of 82% and a specificity of 83.62% [LR(+) 3.63] was obtained.
The result of our analysis is similar to that reported by Azizi et al.,10 who report that high respiratory rates (>26 bpm) correlate with higher MP (pseudo R2: 0.021; p < 0.01) and consequently with higher mortality.
In conclusion, after performing a post hoc analysis of the MPD and using frequentist statistics, we observed that high respiratory rates were associated with a greater probability of generating high-energy MP, regardless of the ventilatory mode. This attractive hypothesis derived from the findings of our study highlights a gap in the current knowledge that will need to be addressed by further and more comprehensive research.
Authors’ contributionAF-C performed the study design, formal statistical analysis, wrote and edited the present manuscript; MI-E, AG-C, AC, JN-S performed the formal revision and edited this manuscript. All authors read and approved the final manuscript.
FundingThis work did not receive any funding.
Conflict of interestAll authors declare no conflict of interest.
WeVent®, International Mechanical Ventilation Group.
Please cite this article as: Fajardo-Campoverdi A, Ibarra-Estrada M, González-Castro A, Cortés A, Núñez-Silveira JM. Trauma relacionado a alta frecuencia: el nuevo orden mundial?. Med Intensiva. 2024. https://doi.org/10.1016/j.medin.2024.03.002