To describe the main factors associated with proper recognition and management of patient–ventilator asynchrony (PVA).
DesignAn analytical cross-sectional study was carried out.
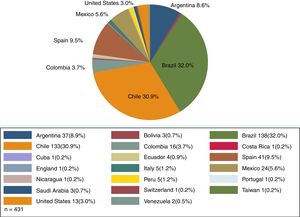
SettingAn international study conducted in 20 countries through an online survey.
ParticipantsPhysicians, respiratory therapists, nurses and physiotherapists currently working in the Intensive Care Unit (ICU).
Main variables of interestUnivariate and multivariate logistic regression models were used to establish associations between all variables (profession, training in mechanical ventilation, type of training program, years of experience and ICU characteristics) and the ability of HCPs to correctly identify and manage 6 PVA.
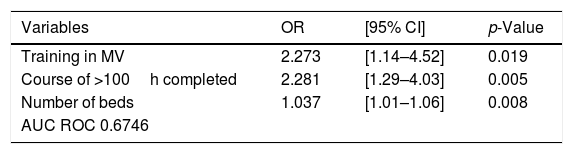
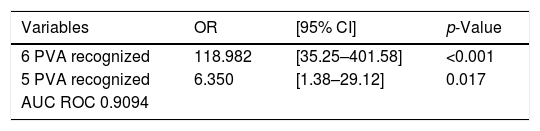
ResultsA total of 431 healthcare professionals answered a validated survey. The main factors associated to proper recognition of PVA were: specific training program in mechanical ventilation (MV) (OR 2.27; 95%CI 1.14–4.52; p=0.019), courses with more than 100h completed (OR 2.28; 95%CI 1.29–4.03; p=0.005), and the number of ICU beds (OR 1.037; 95%CI 1.01–1.06; p=0.005). The main factor influencing the management of PVA was the correct recognition of 6 PVAs (OR 118.98; 95%CI 35.25–401.58; p<0.001).
ConclusionIdentifying and managing PVA using ventilator waveform analysis is influenced by many factors, including specific training programs in MV, the number of ICU beds, and the number of recognized PVAs.
Describir los factores asociados al correcto reconocimiento y manejo de la asincronía paciente-ventilador (APV).
DiseñoEstudio analítico transversal.
ÁmbitoEstudio internacional realizado en 20 países mediante una encuesta a través de Internet.
ParticipantesMédicos, terapeutas respiratorios, enfermeras/os y fisioterapeutas que trabajan actualmente en unidades de cuidados intensivos (UCI).
Principales variables de interésSe utilizó un análisis uni y multivariado para describir la asociación entre todas las variables (profesión, formación en ventilación mecánica, tipo de programa de formación, años de experiencia y características de la UCI en la cual trabajan los profesionales) con la correcta identificación y manejo de 6 APV.
ResultadosUn total de 431 profesionales respondieron una encuesta validada previamente. Los factores asociados a una correcta identificación de 6 APV fueron: haber completado un programa de formación específico sobre ventilación mecánica (OR: 2,27; IC 95%: 1,14-4,52; p=0,019), programa de formación con más de 100h (OR: 2,28; IC 95%: 1,29-4,03; p=0,005) y el número de camas de UCI (OR: 1,037; IC 95%: 1,01-1,06; p=0,005). El principal factor asociado a un adecuado manejo de la APV fue la correcta identificación de 6 APV (OR: 118,98; IC 95%: 35,25-401,58; p<0,001).
ConclusionesLa identificación y el manejo de la asincronía paciente-ventilador, mediante el análisis de las curvas del ventilador está influenciada por programas de formación, específicos sobre ventilación mecánica, el número de camas de la UCI y el número de asincronías identificadas correctamente.
Patient-ventilator asynchrony (PVA) is a common phenomenon that occurs in a significant percentage (25%) of mechanically ventilated patients.1 PVA is defined as “a lack of coordination between two events (initiation of the patient's effort and the mechanical ventilator assistance) that are supposed to occur at the same time.”2 The lack of coordination between these two events has a negative impact on patient's outcome such as longer duration of mechanical ventilation (MV)3 and higher hospital and ICU mortality.4,5
Accurate detection of PVA is challenging at the bedside. Inspection of pressure/time and flow/time waveforms, displayed at the mechanical ventilator screen, is the most common available way to identify different types of PVA.6 However, this method has shown to be neither accurate nor sensitive. For instance, in a recent observational study conducted for our group, only 21% of total healthcare professionals (HCPs) included were able to proper identify different types of PVA.7 In addition, Colombo et al.,8 observed that the ability of intensive care unit physicians to recognize PVA was low and decreased at higher prevalence when breath by breath analysis was performed.
Currently, few studies support the idea that expertise and specific training in MV are able to increase the ability of HCPs to identify PVA.7,9 The latter becomes an important fact to consider since some types PVA (e.g. reverse triggering) are very difficult to recognize and require specific training and clinical experience.10 Further, to the best of our knowledge, there are no reports describing other factors that may potentially affect the ability to recognize and manage different types of PVA such as type of training program in mechanical ventilation, type of Intensive Care Unit (ICU), number of ICU beds, number of mechanically ventilated patients, profession or academic degree, and years of experience. Therefore, we aimed to describe the association between all the previously mentioned variables with the ability of HCPs to identify and manage different types of PVA using waveform analysis.
Material and methodsThe study was approved by the Ethics Committee of the Hospital Clinico Universidad de Chile (file number 1006/18).
Subjects and study designWe conducted an analytical cross-sectional international study in which an online survey was designed in two languages (Spanish and English) using Google forms (Google LLC. Mountain View, CA, USA). The survey was distributed in different countries through an online link. The online link was posted on three major websites dedicated to MV, and also sent by email to HCPs affiliated to Intensive Care Medicine Societies from Chile, Brazil and Spain. The Chilean Intensive Care Society send the survey to physicians, nurses and physiotherapists. The Brazilian Society send the survey only to physiotherapists and the Spanish Society only to physicians. It is important to mention that in most Latin American countries physiotherapists and nurses are specially trained in MV (as respiratory therapist and physicians), which is the reason why they were included in the study.
SurveyThe survey included a description of the topic, the main goals of it, a disclaimer that all information provided by HCPs would remain anonymous and 22 questions. The multiple-choice and written questions that HCPs had to answer in the survey were: (1) email address, (2) profession (respiratory therapist, physician, nurse, physiotherapist), (3) country, (4) years of experience, (5) Have you completed successfully at least one course focused on mechanical ventilation with a specific curriculum that included patient–ventilator asynchrony (yes, no), (6) type of training (Course, MSc, PhD, Clinical Internship), (7) number of hours dedicated to the course that included the PVA topic, (8) type of ICU in which the HCP works (medical ICU (MICU), surgical ICU (SICU), coronary (ICU), pediatric ICU (PICU), neonatal (NICU)); (allowance of more than 1 answer in this question), (9) number of beds available in the ICU and (10) number of mechanically ventilated patients in the ICU.
From question 11 to 22, the survey was related to identification and management of different types of PVA based on six different videos displaying the pressure/time and flow/time waveforms. All PVA videos were recorded from a Puritan Bennett 840 mechanical ventilator (Covidien. Carlsbad, CA, USA) connected to a test lung. For each video, there was a multiple-choice question (MCQ) regarding identification of the displayed asynchrony and another MCQ regarding the management of PVA. Possible choices for the identification questions were: (a) double triggering, (b) auto triggering, (c) ineffective effort, (d) flow starvation (flow asynchrony), (e) premature cycling, (f) delayed cycling, and (g) overshooting. Possible choices regarding PVA management were: (a) Switch to a pressure controlled ventilatory mode, (b) Increase inspiratory time from 0.80s to 1.20s, (c) Modify rise time from 50ms to 150ms, (d) Modify the inspiratory trigger sensitivity from 8L/min to 2L/min, (e) Decrease inspiratory time from 1.20s to 0.80s, and (f) Inflate cuff from 10mmHg to 25mmHg.
Definitions and events of interestProper identification and management of different type of PVA was based on experts’ answers. Each video was validated by 10 experts in the field of MV with an inter-observer agreement of 100%. The number of correctly recognized and managed PVA (0–6 PVA) by HPCs was obtained.
The different types of PVA were defined as following: double-triggering was defined as “2 consecutive inspirations occurring within an interval of less than half of the mean inspiratory time.”11 Autotriggering as “a delivery of a breath that is neither scheduled (based on the set respiratory frequency) nor initiated by the patient.”11 Ineffective effort as “patient efforts that are not sensed by the ventilator.”11 Flow starvation (flow asynchrony) as “the PVA that occurs when gas delivery fails to meet patient's flow demand.”12 Premature cycling as a type of PVA that occurs “when the patient's neural inspiratory time exceeds the ventilator inspiratory time.”11 Delayed cycling as “type of PVA that occurs when the ventilator inspiratory time exceeds the patients neural inspiratory time.”11 Overshooting as “type of PVA that occurs because of an exaggerated delivery of inspiratory flow.”13
Professionals were further categorized according to previous training in MV (trained and non-trained) defined based on our previous study7 as: “HCPs who had successfully completed at least one course entirely focused on mechanical ventilation from a formal educational institution (university or college) and with a specific curriculum that included modes of mechanical ventilation, patient–ventilator synchrony, and ventilator waveform analysis among the topics.” Type of training programs were also categorized as courses completed with less than 100h (courses<100h), courses completed with 100h or more (courses>100h), Master degree (MSc), Doctorate degree (PhD) or clinical internship), type of ICU where HCPs worked (MICU,SICU,CICU,PICU,NICU), profession (physiotherapist, physician, respiratory therapist, nurse).
Years of experience, number of ICU beds and the percentage of mechanically ventilated patients (% MV patients) at the ICU were considered continuous variables.
The percentage of mechanically ventilated patients was defined as the reported number of mechanically ventilated patients/reported number of ICU beds×100%.
Statistical analysisAbsolute and relatives (%) values were used for qualitative nominal variables. Median and interquartile range [p50 (p25−p75)] were used to express non normal, continuous and ordinal distribution variables. Whilst, arithmetic mean and standard deviation were used [X±SD] for normal distribution variables. To describe and explore the association between all variables and proper PVA recognition and management, univariate and multivariate logistic regression models were used. Identifying 6 PVA was considered the outcome variable. The proper management of 6 PVA was, also, considered the outcome variable. Association between the number of, correctly identified, PVA, and proper PVA management was also studied. Odds ratio (OR), 95% confidence interval (95%CI) and p-value were reported for all analysis. For multivariate analysis we also reported the area under the curve (AUC) of the receiver operator curve (ROC). A p-value of <0.05 and a 95% CI was considered statistically significant for all analysis. The group of nurses was considered the reference category for HCPs. Models were adjusted by years of experience and profession. STATA 15.1 SE (StataCorp, College Station, TX, USA) was use for all data analysis.
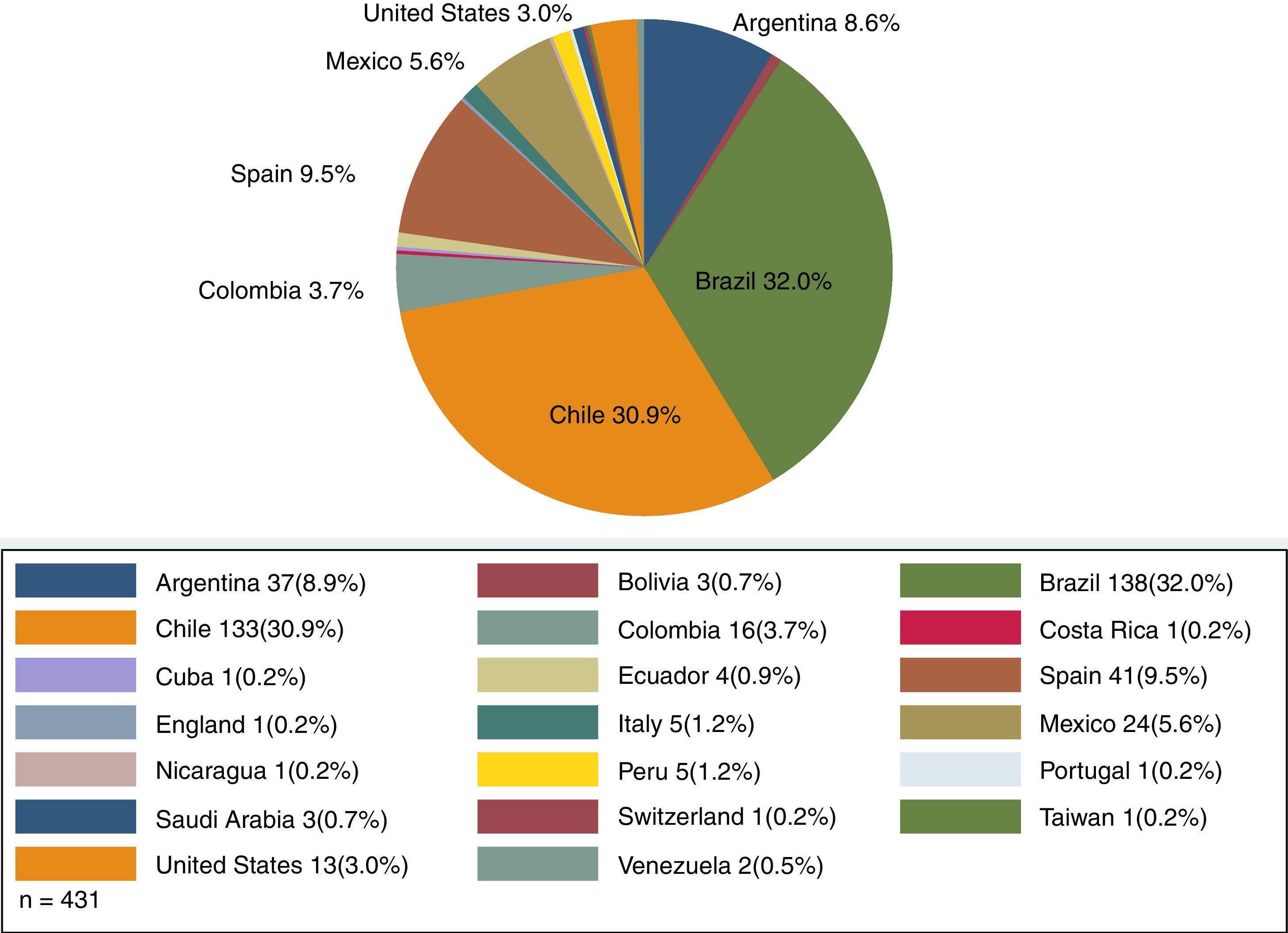
ResultsA total of 431 HCPs, including 252 physiotherapists (58.5%), 112 physicians (26.0%), 36 respiratory therapists (8.4%), and 31 nurses (7.2%) from 20 different countries answered the survey. Distribution of HCPs according to country is summarized in Fig. 1.
A total of 103 HCPs (23.9%) completed the survey using the link provided by the Intensive Care Societies, whereas 328 HCPs (76.1%) answered the survey using the link provided by the online websites. A total of 150 surveys invitations were sent, in total, by the Intensive Care Societies which means that the response rate was 68.6% (103 HCPs).
The median years of experience working in the ICU were 5 (2–10). A successfully completed training program in MV, with a specific curriculum that included PVA among the topics, was reported by 307 HCPs (71.2%). Median duration of training programs was 22h (12–50). The distribution of HCPs according to the type of training program variables was: courses<100h were completed by 250 HCPs (58.0%), courses>100h by 81 HCPs (18.8%), MSc degree by 11 HCPs (2.6%), PhD degree by 6 HCPs (1.4%), and Clinical Internship by 65 HCPs (15.1%).
The distribution of HCPs according to the type of ICU where they worked was 340 HCPs (78.9%) working at a Medical ICU, 171 HCPs (39.7%) at a Surgical ICU, 109 HCPs (25.3%) at a Coronary ICU, 50 HCPs (13.7%) at a Pediatric ICU and 35 HCPs (8.1%) working at a Neonatal ICU.
The median number of beds per unit was 12 beds (10–19) and the percentage of mechanically ventilated patients was 50% (37.5–66.7) per unit.
Identifying patient–ventilator asynchronyA median of 4 (2–5) PVA were correctly identified. Distribution of HCPs according to the number of correctly identified PVA was: eighty-four HCPs (19.5%) identified the 6 different types of PVA, 63 HCPs (14.6%) identified 5 PVA, 98 HCPs (22.7%) identified 4 PVA, 68 HCPs (15.8%) identified 3 PVA, 58 HCPs (13.5%) identified 2 PVA, 47 HCPs (10.9%) identified correctly 1 PVA, and 13 HCPs (3.0%) did not identify any PVA. Distribution of HCPs according to the type of PVA identified showed that 357 HCPs (82.8%) identified double triggering, 197 HCPs (45.7%) identified delayed cycling, 282 HCPs (65.4%) identified auto triggering, 231HCPs (53.6%) identified flow starvation (flow asynchrony), 275 HCPs (63.8%) identified ineffective effort and 236 HCPs (54.8%) identified overshooting.
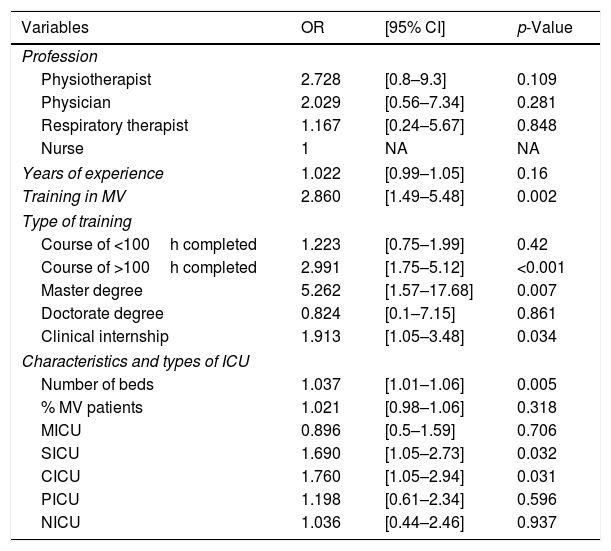
Univariate logistic regression model analysis showed a statistically significant association between specific training in MV [OR 2.86; 95% CI 1.49–5.48; p=0.002], courses>100h [OR 2.99; 95% CI 1.75–5.12; p<0.001], MSc [OR 5.26; 95% CI 1.57–17.68; p=0.007], clinical internship [OR 1.91; 95% CI 1.05–3.48; p=0.034], number of ICU beds [OR 1.03; 95% CI 1.01–1.06; p=0.005], HCPs working at the SICU [OR 1.69; 95% CI 1.05–2.73; p=0.032], CICU [OR 1.76; 95% CI 1.05–2.94; p=0.031] and the ability of HCPs to identify the 6 PVA correctly (see Table 1).
Factors associated with proper recognition of 6 PVA using Univariate Logistic Regression Analysis.
| Variables | OR | [95% CI] | p-Value |
|---|---|---|---|
| Profession | |||
| Physiotherapist | 2.728 | [0.8–9.3] | 0.109 |
| Physician | 2.029 | [0.56–7.34] | 0.281 |
| Respiratory therapist | 1.167 | [0.24–5.67] | 0.848 |
| Nurse | 1 | NA | NA |
| Years of experience | 1.022 | [0.99–1.05] | 0.16 |
| Training in MV | 2.860 | [1.49–5.48] | 0.002 |
| Type of training | |||
| Course of <100h completed | 1.223 | [0.75–1.99] | 0.42 |
| Course of >100h completed | 2.991 | [1.75–5.12] | <0.001 |
| Master degree | 5.262 | [1.57–17.68] | 0.007 |
| Doctorate degree | 0.824 | [0.1–7.15] | 0.861 |
| Clinical internship | 1.913 | [1.05–3.48] | 0.034 |
| Characteristics and types of ICU | |||
| Number of beds | 1.037 | [1.01–1.06] | 0.005 |
| % MV patients | 1.021 | [0.98–1.06] | 0.318 |
| MICU | 0.896 | [0.5–1.59] | 0.706 |
| SICU | 1.690 | [1.05–2.73] | 0.032 |
| CICU | 1.760 | [1.05–2.94] | 0.031 |
| PICU | 1.198 | [0.61–2.34] | 0.596 |
| NICU | 1.036 | [0.44–2.46] | 0.937 |
Nurses were considered the reference category. MV: Mechanical ventilation; ICU: Intensive care unit; % MV patients: percentage of mechanically ventilated patients; MICU: Medical Intensive Care Unit; SICU: Surgical Intensive care unit; CICU: Coronary Intensive Care Unit; PICU: Pediatric Intensive Care Unit; NICU: Neonatal Intensive Care Unit; OR: Odds Ratio; 95% CI: 95% confidence interval; NA: not applicable.
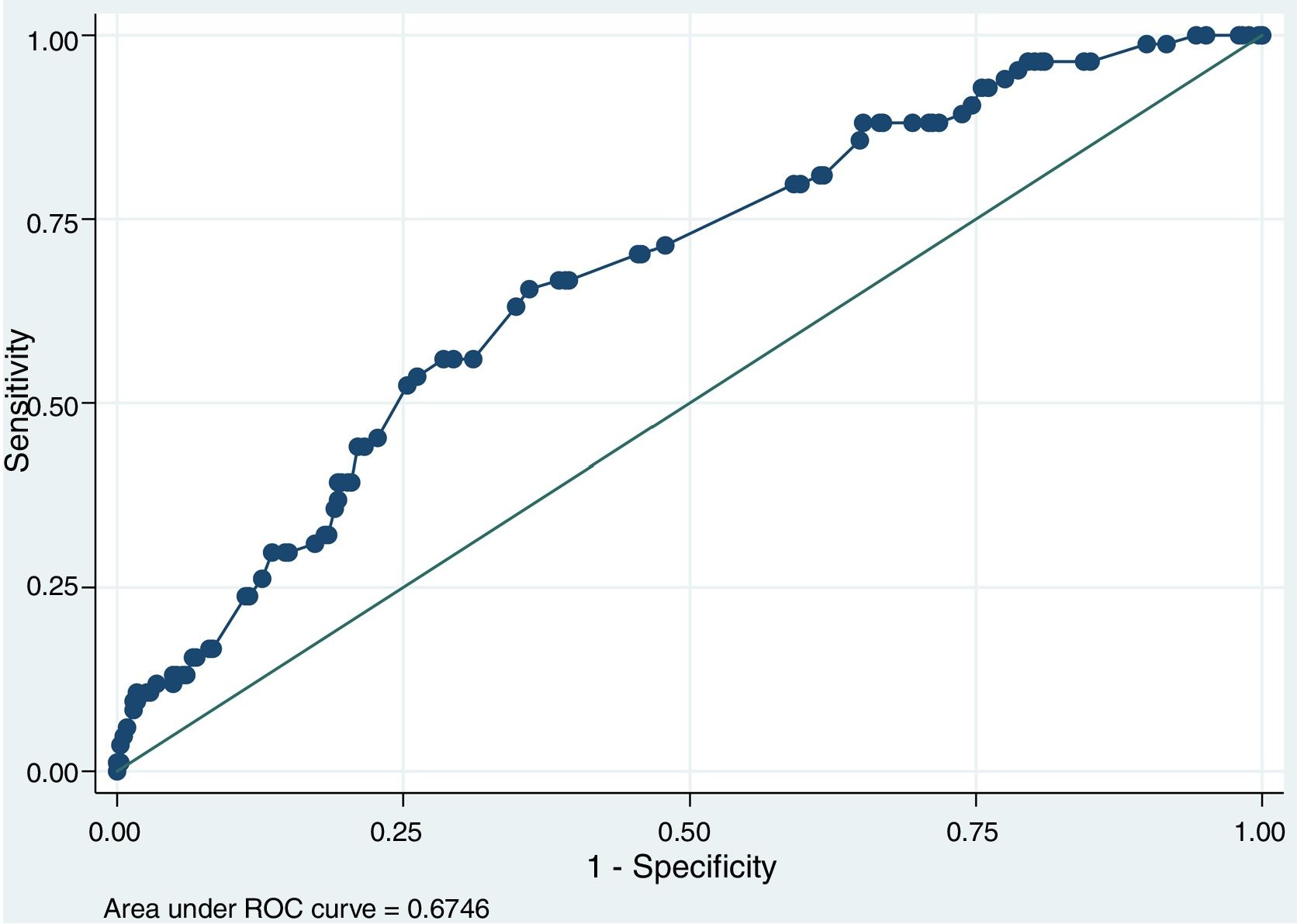
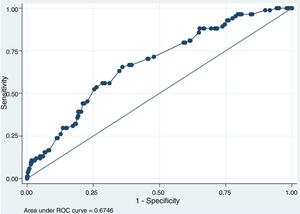
Multivariate logistic regression model, adjusted for profession and years of experience, showed that specific training in MV, courses>100h and number of ICU beds are factors associated with the ability of HCPs to identify PVA properly (see Table 2). Multivariate logistic regression analysis also showed an AUC ROC of 0.67 (Fig. 2).
Factors associated with proper recognition of 6 PVA using Multivariate Logistic Regression Analysis.
| Variables | OR | [95% CI] | p-Value |
|---|---|---|---|
| Training in MV | 2.273 | [1.14–4.52] | 0.019 |
| Course of >100h completed | 2.281 | [1.29–4.03] | 0.005 |
| Number of beds | 1.037 | [1.01–1.06] | 0.008 |
| AUC ROC 0.6746 | |||
MV: Mechanical Ventilation; PVA: Patient–Ventilator Asynchronies; AUC ROC: Area under the ROC Curve; OR: Odds Ratio; 95% CI: 95% confidence interval.
A median of 3 (2–4) PVA were managed correctly by HCPs. The 6 types of PVA were managed correctly by 54 HCPs (12.5%), 45 HCPs (10.4%) managed 5 PVA, 70 HCPs (16.2%) managed 4 PVA, 73 HCPs (16.9%) managed 3 PVA, 92 HCPs (21.3%) managed 2 PVA, 60 HCPs (13.9%) managed 1 PVA and 37 HCPs (8.9%) did not solve any PVA. Distribution of HCPs according to the type of correctly managed PVA showed that 265 HCPs (61.5%) managed double triggering correctly, 237 HCPs (55.0%) delayed cycling, 181 HCPs (42.9%) auto triggering, 188 HCPs (43.6%) flow starvation (flow asynchrony), 254 HCPs (58.9%) ineffective effort, and 168 HCPs (39.0%) overshooting.
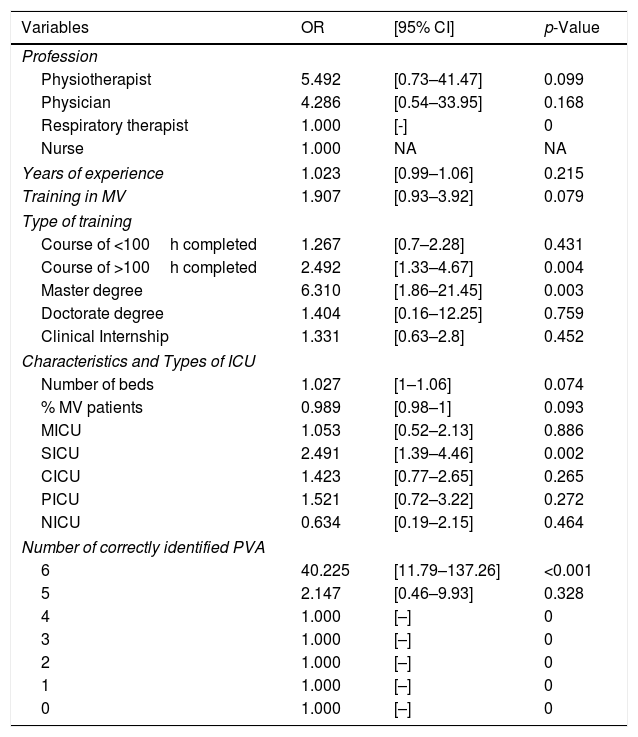
Univariate logistic regression analysis showed a statistically significant association between the ability of HCPs to manage PVA, properly, with courses>100h [OR 2.49; 95% CI 1.33–4.67; p=0.004], MSc degree [OR 6.31; 95% CI 1.86–21.45; p=0.003] and working at the SICU [OR 2.49; 95% CI 1.39–4.46; p=0.002]. Univariate logistic regression analysis also showed a statistically significant association between the number of PVA identified correctly (6 PVA) and the proper management of 6 PVA [OR 40.22; 95% CI 11.79–137.26; p<0.001)] (see Table 3).
Factors associated with proper management of 6 PVA using Univariate Logistic Regression Analysis.
| Variables | OR | [95% CI] | p-Value |
|---|---|---|---|
| Profession | |||
| Physiotherapist | 5.492 | [0.73–41.47] | 0.099 |
| Physician | 4.286 | [0.54–33.95] | 0.168 |
| Respiratory therapist | 1.000 | [-] | 0 |
| Nurse | 1.000 | NA | NA |
| Years of experience | 1.023 | [0.99–1.06] | 0.215 |
| Training in MV | 1.907 | [0.93–3.92] | 0.079 |
| Type of training | |||
| Course of <100h completed | 1.267 | [0.7–2.28] | 0.431 |
| Course of >100h completed | 2.492 | [1.33–4.67] | 0.004 |
| Master degree | 6.310 | [1.86–21.45] | 0.003 |
| Doctorate degree | 1.404 | [0.16–12.25] | 0.759 |
| Clinical Internship | 1.331 | [0.63–2.8] | 0.452 |
| Characteristics and Types of ICU | |||
| Number of beds | 1.027 | [1–1.06] | 0.074 |
| % MV patients | 0.989 | [0.98–1] | 0.093 |
| MICU | 1.053 | [0.52–2.13] | 0.886 |
| SICU | 2.491 | [1.39–4.46] | 0.002 |
| CICU | 1.423 | [0.77–2.65] | 0.265 |
| PICU | 1.521 | [0.72–3.22] | 0.272 |
| NICU | 0.634 | [0.19–2.15] | 0.464 |
| Number of correctly identified PVA | |||
| 6 | 40.225 | [11.79–137.26] | <0.001 |
| 5 | 2.147 | [0.46–9.93] | 0.328 |
| 4 | 1.000 | [–] | 0 |
| 3 | 1.000 | [–] | 0 |
| 2 | 1.000 | [–] | 0 |
| 1 | 1.000 | [–] | 0 |
| 0 | 1.000 | [–] | 0 |
Nurses were considered the reference category. MV: Mechanical ventilation; ICU: Intensive care unit; % MV patients: percentage of mechanically ventilated patients; MICU: Medical Intensive Care Unit; SICU: Surgical Intensive care unit; CICU: Coronary Intensive Care Unit; PICU: Pediatric Intensive Care Unit; NICU: Neonatal Intensive Care Unit. PVA: Patient–Ventilator Asynchronies. OR: Odds Ratio; 95% CI: 95% confidence interval; NA: not applicable.
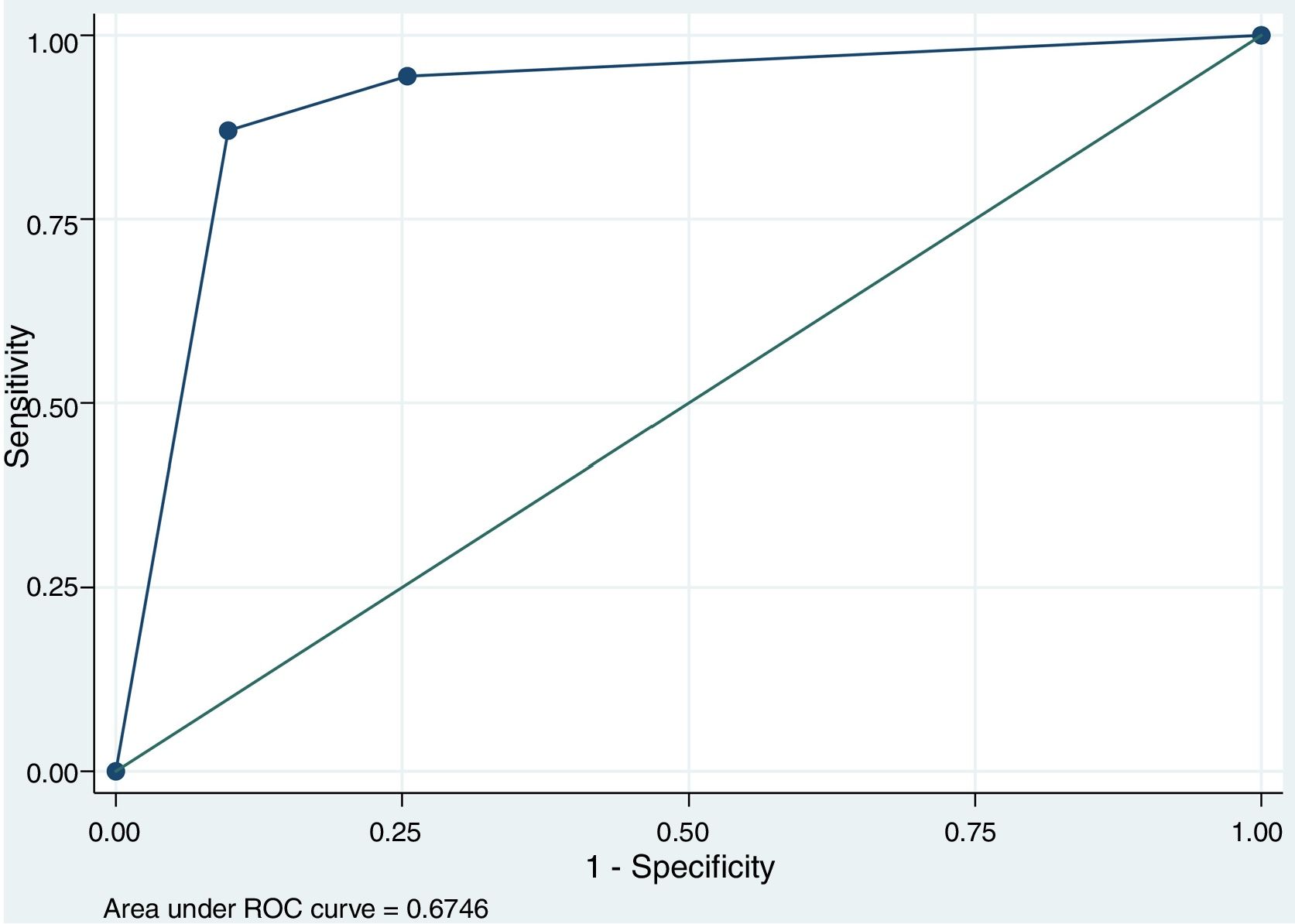
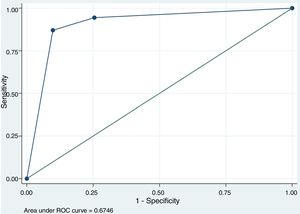
Multivariate logistic regression analysis, adjusted for years of experience and profession, showed a statistically significant association between the ability of HCPs to recognize 5–6 PVA with proper management of PVA (see Table 4). An AUC ROC of 0.90 value was obtained (Fig. 3).
Factors associated with proper management of 6 PVA using Multivariate Logistic Regression Model Analysis.
| Variables | OR | [95% CI] | p-Value |
|---|---|---|---|
| 6 PVA recognized | 118.982 | [35.25–401.58] | <0.001 |
| 5 PVA recognized | 6.350 | [1.38–29.12] | 0.017 |
| AUC ROC 0.9094 | |||
PVA: Patient–Ventilator Asynchronies; AUC ROC: Area under the ROC Curve; OR: Odds Ratio; 95% CI: 95% confidence interval.
The major findings of our study were: First, a specific training program in MV (course>100h, MSc, Clinical Internship) that includes PVA training, the number of available ICU beds and the type of ICU (SICU, CICU) are factors associated with a correct recognition of PVA. Several studies have mentioned the importance of training to assess and understand patient–ventilator interaction properly by using waveform analysis.7,9,12,14 A study conducted by Chacon et al.,9 also showed that specific training is a key factor for proper PVA recognition. In their study 2 nurses were trained 2h/day for 20 days to detect ineffective inspiratory efforts, during expiration, by observing respiratory mechanics and pressure/time and flow/time waveforms. After the specific training program, the 2 nurses were able to identified ineffective efforts as accurately as critical care experts in MV. Second, according to multivariate analysis a specific training program in MV and the number of ICU beds were factors that allowed HCPs to identify 67% of all PVA. Third, a specific training program in MV (course>100h, MSc), type of ICU and the number of recognized PVA (6 PVA) were factors associated with the ability of HCPs to manage PVA properly. Fourth, HCPs who identified 5 or 6 PVA increased 6-fold and 118-fold (respectively) their odds of managing correctly 6 PVA. In fact, HCPs who identified 5 and 6 PVA were able to manage 90% of all PVA, showing the association between the number of recognized PVA and the proper management. Fifth, as in our previous study,7 neither profession nor experience influenced proper recognition and management. Sixth, the most recognized asynchrony was double triggering (82.8%) whilst the least recognized was delayed cycling (45.7%). On the other hand, double triggering was properly managed by most of HCPs (61.5%) whilst overshooting was the least managed (39.0%).
Identifying PVA by using waveform analysis is a challenging and difficult task. Partly, because there are no standard definitions which might lead to confusion and misinterpretation. Mireles-Cabodevila and Dugar15 also mentioned that none of the actual definitions guide us toward the etiology. This is an important point to mention because, the same PVA can be manage differently according to etiology. For example, ineffective efforts can be managed either by decreasing the level of support or by modifying the level of trigger sensitivity. For instance, if ineffective efforts are caused by an excessive level of support, modifying the level of trigger sensitivity will not solve it. The lack of knowledge about the PVA etiology may be an explanation for the low rate of proper management in our study. On the other hand, an explanation for the high rate of proper management of ineffective effort (58.9%) may be that modifying the trigger sensitivity is the most intuitive way to solve this type of PVA and was considered the correct answer in the survey.
Over the past few years an increasing number of studies have demonstrated a low percentage of PVA recognition using waveform analysis.7,8 Moreover, the rate of recognition is inversely related to the prevalence of PVA.16 In our study, the percentage of HCPs that were able to identify all PVA was quite low (19.5%). These results are similar to the previously published by our research group, were the percentage of HCPs that identified all PVA, using waveform analysis, was 21.3%.7 However, in the current study, we found that only 13 HCPs (3%) did not identify any PVA, while in our previous study 61 HCPs (16.7%) did not identify any PVA.7 The fact that in our previous study the percentage of HCPs without specific training was 43.4% versus a 28.8% of non-trained HCPs in the current study might explain this difference.
Our study has some limitations. First, regarding to the survey. HCPs were assessed by using an online survey (outside the clinical context) where the guessing factor and unlimited time to answer it might bias the results. This is important to mention because in a live setting the answers of HCPs could be affected by anxiety, tension, time factor among other distractors. Also, there is no certainty about whether professionals used additional material to answer the questions. In terms of survey content, the survey included only one choice to manage double triggering (increase inspiratory time from 0.80s to 1.20s). However, we must consider that double triggering is a type of PVA that can be caused by autotriggering,17 flow asynchrony (flow starvation),18 reverse triggering18–20 and, as mentioned by Aquino Esperanza et al.,18 by a “diaphragmatic contraction (neural time) that exceeds the mechanical insufflation time and drives an ineffective effort that, if strong and long enough, generates a second mechanical breath.” Therefore, in order to properly manage double triggering, additional information about clinical condition and context of the patient should be provided in future survey questions. Also, identification and management of reverse triggering was not included in the survey. This is a poorly recognized PVA that occurs, in deeply sedated patients, when the patient's respiratory center is activated in response to a passive insufflation of the lungs which may lead to double triggering as previously mentioned.18–20 We decided not to include reverse triggering in the survey because it is a very difficult, PVA, to identify only by visual inspection of pressure time and flow time waveforms. There is, also, difficult to recognized without additional information regarding the clinical context of the patient (level of sedation) and the information provided by the esophageal pressure waveform or the electrical activity of the diaphragm. Increasing sedation or the use of neuromuscular blockers (NMBA) was not included in the survey as a strategy to manage PVA. The reason why sedation was not included among the choices to manage PVA was because it is a controversial topic where some studies have shown that PVA increases with deep sedation,21 whist other studies have shown improvement on patient–ventilator interaction.22 Also, the use of NMBA was not included as a choice to manage PVA because, theoretically, NMBA will correct any type of PVA regardless of etiology. Recently, de Haro et al.23 assessed the role of sedatives alone, sedatives plus opioids and opioids alone on PVA improvement. They found that in sedatives plus opioids days, the sedative dose was directly associated with the rate of PVA and with a lower level of consciousness, whereas higher opioid doses were associated with a lower asynchrony index without worsening the level of consciousness. These results suggest that opioids should be considered as a strategy to manage PVA in future survey questions.
Second, limitations regarding to professionals that answered the survey. A potential selection bias might be present, due to the nature of our study, since participation was voluntary and might not represent the whole population of HCPs working at ICU. However, participation rate was very high (68.6%) based on surveys sent by intensive care societies. There was an uneven distribution according to the HCP country (for example 138 and 133 HCPs from Brazil and Chile, respectively, answered the survey versus just, 1 HCP from Taiwan, Portugal, England, Cuba, Costa Rica, Nicaragua and Switzerland). This precludes a possible analysis of country as a potential factor associated with proper recognition and management of PVA. There was also an uneven distribution according to profession. The percentage of physicians who answered the survey was 26% which might be considered a low rate. Specially, because physicians are the professionals in charge of mechanical ventilation. However, it is important to mention that in some Latin American countries including Chile, Brazil, Argentina, physiotherapists and nurses are specially trained to manage mechanical ventilation along with the physician. An explanation for the uneven distribution according to profession could be the fact that only the Chilean and the Spanish Intensive Care Societies sent the survey to physicians whilst, the Brazilian society only sent the survey to physiotherapists. Finally, although our data base shows no multiple surveys answered by the same participant (e.g. same email address), we are not certain whether the same professional answered the survey more than once by using different email accounts.
Identifying patient–ventilator asynchrony is a key factor that increases the likelihood of managing this common phenomenon properly. Specific training programs in mechanical ventilation, with more than 100h completed and the number of available ICU beds are relevant factors that influence the ability of HCPs to identify PVA. The number of recognized PVA is the main factor that leads to proper, PVA, management.
Contribution of each authorIvan I. Ramirez PT contributed with literature search, study design, analysis of data, manuscript preparation.
Rodrigo S. Adasme PT CRT MSc contributed with study design, analysis of data, manuscript preparation, and review of manuscript.
Daniel H. Arellano PT CRT MSc contributed with study design, analysis of data and review of manuscript.
Angelo Roncalli M. Rocha PT MSc contributed with data collection and review of manuscript.
Flavio Maciel D. Andrade PT PhD contributed with data collection and review of manuscript.
Juan Núñez-Silveira PT contributed with data collection and review of manuscript.
Nicolás A. Montecinos PT CRT contributed with data collection and review of manuscript.
Sarah Dias PT contributed with data collection and review of manuscript.
L. Felipe Damiani PT MSc contributed with analysis of data, preparation and review of manuscript.
Ruvistay Gutierrez-Arias PT MSc contributed with analysis of data, preparation and review of manuscript.
Beatriz Lobo-Valbuena contributed with preparation and review of the manuscript.
Federico Gordo MD PhD contributed with data collection, preparation and review of manuscript.
Funding sourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestNone.
We thank to Sociedad Chilena de Medicina Intensiva (SOCHIMI), Associação Brasileira de Fisioterapia Cardiorrespiratória e Fisioterapia em Terapia Intensiva (ASSOBRAFIR), and Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (SEMICYUC) for helping with the promotion and distribution of the survey links. We also thank Alvaro Espinoza (Hospital Guillermo Grant Benavente, Concepcion, Chile) and Ignacio Lobos (Hospital Clinico de la Florida, Santiago, Chile) for helping with the distribution of the survey. L. Felipe Damiani acknowledges partial support from CONICYT-PFCHA/Doctorado Nacional/2017-folio 21171551.