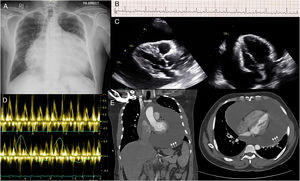
A 43-year-old man presented to the emergency department with a 2 week history of progressive breathlessness and fatigue. Physical examination revealed hypotension, tachycardia, jugular venous distension, pulsus paradoxus, and muffled heart sounds. His blood pressure was 90/60mm Hg, and the heart rate was 110 beats per minute. Chest x-ray showed a “water bottle configuration” suggestive of pericardial effusion (Fig. 1A). His electrocardiogram showed sinus tachycardia with small voltage QRS complexes and a degree of electrical alternans (Fig. 1B). Transthoracic echocardiography (TTE) revealed a large global pericardial effusion measuring>40mm in diameter with swinging of the heart freely in an anterior–posterior fashion (Fig. 1C, see video) and collapse of the right and left atria in end diastole, which was consistent with cardiac tamponade. Spectral Doppler demonstrated exaggerated respiratory variations of the mitral and tricuspid in-flow Doppler consistent with increased intrapericardial pressure and tamponade (Fig. 1D). A single axial, contrast-enhanced CT scan of the chest at the level of the heart showed a massive pericardial effusion (white arrows) surrounding the contrast-filled heart (LV=left ventricle) (Fig. 1E). The patient was immediately transferred to the coronary care unit where an emergency pericardiocentesis was performed which successfully drained 2.4 litres of serous pericardial fluid with immediate improvement of hemodynamics. Subsequent analysis showed a transudative pericardial fluid. All the connective tissue, cancer and infective markers were all negative and a diagnosis of idiopathic pericardial effusion was made. The patient was discharged well with resolution of the pericardial effusion on repeat TTE 4 days later. At 3 and 6 months follow-up, the patient was asymptomatic and well.
Declaration of InterestNone
DisclosureAll authors have contributed to the conception and design of the study, acquisition of data and analysis and interpretation of data. We drafted the article and revised it and approved the final version to be submitted.