To analyze outcomes and factors related to mortality among very elderly trauma patients admitted to intensive care units (ICUs) participating in the Spanish trauma ICU registry.
DesignA multicenter nationwide registry. Retrospective analysis. November 2012–May 2017.
SettingParticipating ICUs.
PatientsTrauma patients aged ≥80 years.
InterventionsNone.
Main variables of interestThe outcomes and influence of limitation of life sustaining therapy (LLST) were analyzed. Comparisons were established using the Wilcoxon test, Chi-squared test or Fisher's exact test as appropriate. Multiple logistic regression analysis was performed to analyze variables related to mortality. A p-value <0.05 was considered statistically significant.
ResultsThe mean patient age was 83.4±3.3 years; 281 males (60.4%). Low-energy falls were the mechanisms of injury in 256 patients (55.1%). The mean ISS was 20.5±11.1, with a mean ICU stay of 7.45±9.9 days. The probability of survival based on the TRISS methodology was 69.8±29.7%. The ICU mortality rate was 15.5%, with an in-hospital mortality rate of 19.2%. The main cause of mortality was intracranial hypertension (42.7%). The ISS, the need for first- and second-tier measures to control intracranial pressure, and being admitted to the ICU for organ donation were independent mortality predictors. LLST was applied in 128 patients (27.9%). Patients who received LLST were older, with more severe trauma, and with more severe brain injury.
ConclusionsVery elderly trauma ICU patients presented mortality rates lower than predicted on the basis of the severity of injury.
Analizar el desenlace y los factores relacionados con la mortalidad de los pacientes traumáticos muy ancianos ingresados en las Unidades de Cuidados Intensivos (UCI) participantes en el Registro Español de Trauma en las UCI (RETRAUCI).
DiseñoRegistro multicéntrico nacional. Análisis retrospectivo. Noviembre de 2012-mayo de 2017.
ÁmbitoLas UCI participantes.
Pacientes o participantesPacientes traumáticos con edad ≥80 años.
IntervencionesNinguna.
Variables de interés principalesAnalizamos el desenlace y la influencia de la limitación de los tratamientos de soporte vital (LLST). Las comparaciones entre grupos se realizaron mediante la prueba de Wilcoxon, la prueba de Chi-cuadrado y la prueba exacta de Fisher según estuviera indicado. Se realizó un análisis multivariante mediante regresión logística para analizar las variables asociadas a la mortalidad. Un valor de p<0,05 se consideró el límite de la significación estadística.
ResultadosLa edad media fue de 83,4±3,3 años. Varones 281 (60,4%). La causa principal del traumatismo fueron las caídas de baja energía en 256 pacientes (55,1%). El Injury Severity Score (ISS) medio fue de 20,5±11,1. La estancia media en las UCI fue de 7,45±9,9 días. La probabilidad de supervivencia, de acuerdo con la metodología TRISS fue de 69,8±29,7%. La mortalidad en las UCI fue del 15,5%. La mortalidad hospitalaria fue del 19,2%. La causa principal fue la hipertensión intracraneal (42,7%). El ISS, la necesidad de medidas de primer o segundo nivel para controlar la presión intracraneal y el ingreso en las UCI orientado a la donación de órganos fueron predictores independientes de mortalidad. Se documentó la LLST en 128 pacientes (27,9%). Los pacientes con LLST fueron mayores, con una mayor gravedad lesional y un traumatismo craneoencefálico más grave.
ConclusionesLos pacientes traumáticos muy ancianos en las UCI presentaron menor mortalidad de la predicha por la gravedad del traumatismo.
The progressive aging of the population expected in the following decades will also represent an increased number of trauma admissions of geriatric patients.1,2 Specifically, geriatric trauma patients represent up to one-fifth of trauma intensive care unit (ICU) admissions in our environment.3
Elderly patients usually present low-energy mechanisms of injury (ground-level falls) complicated with the use of antiplatelets or anticoagulants.4 Whilst age itself is not the only determinant of outcome,1 aging is strongly associated with worst outcomes.4 The changing pattern of epidemiology of trauma patients has resulted in an increased mortality related to preexisting medical conditions and markedly fewer deaths resulted from the complications of injury.5
Care of very elderly ICU patients (those aged ≥80 years-old) will be a key issue in the following years6 and constitute an area of uncertainty, especially in trauma patients. In this setting, clinical guidelines from The Eastern Association for the Surgery of Trauma suggest that in the very old trauma patient, the presence of multiple comorbidities is not necessarily an indicator of poor outcome and, with the exception of the moribund geriatric trauma patients, the initial treatment approach must follow the same principles that in younger counterparts.7 The final outcomes of very elderly trauma patients are a matter of debate,8–10 but recent evidence supports an initial aggressive approach and admission to specialized trauma ICUs.11,12
Our objective was to analyze the outcomes and factors related to mortality of very elderly trauma patients admitted to the ICUs participating in the Spanish Trauma ICU Registry (RETRAUCI), taking into consideration the influence of the limitation of life sustaining therapies (LLST).
MethodsRETRAUCI is an observational, prospective and multicenter nationwide registry initiated on November, 2012. It has the endorsement of the Neurointensive Care and Trauma Working Group of the Spanish Society of Intensive Care Medicine (SEMICYUC). It currently includes 50 registered ICUs with 124 investigators collecting data from trauma patients on a web-based system (www.retrauci.org). Ethics Committee approval for the registry was obtained (Hospital Universitario 12 de Octubre, Madrid: 12/209).
We included in this study all traumatic patients aged ≥80 years-old in the participating ICUs from November, 2012 to May, 2017 with complete medical records (death or hospital discharge). Data on epidemiology, acute management, type and severity of injury, resources utilization, complications and outcomes were recorded. The list of definitions used is shown in the Electronic Supplementary Material, as previously published.3 As per protocol, LLST (withholding or withdrawing therapy) is noted in the registry as a dichotomous variable (yes/no). Patients were followed-up until hospital discharge.
Data used for calculating the Revised Trauma Score (RTS) (respiratory rate, systolic blood pressure and Glasgow coma scale score) were obtained from the first medical attention before initiating resuscitation and/or mechanical ventilation. Data used for calculating the Injury Severity Score (ISS) were prospectively collected by the intensivist at charge of the patient after ICU admission according to the Abbreviated Injury Scale (AIS) updated in 2008. Probability of survival was calculated using the Trauma and Injury Severity Score (TRISS) methodology.13 The expected mortality for the whole sample was calculated as the sum of the individual probabilities of mortality.
Incomplete data to obtain hospital outcome was the exclusion criteria.
Statistical analysisQuantitative data were reported as median±standard deviation and categorical data as number (percentage). Comparison of groups with quantitative variables was performed using Wilcoxon test and differences between groups with categorical variables were compared using the Chi-squared test or Fisher's exact test as appropriate. A multiple logistic regression analysis was performed to analyze clinical variables related to mortality. The variables entered in logistic regression analysis were those significantly associated with mortality in the univariate analysis. A p value <0.05 was considered significant. We reported all results as stated in the RECORD statement.14 Statistical analysis was performed with STATA 15 (StataCorp. 2017).
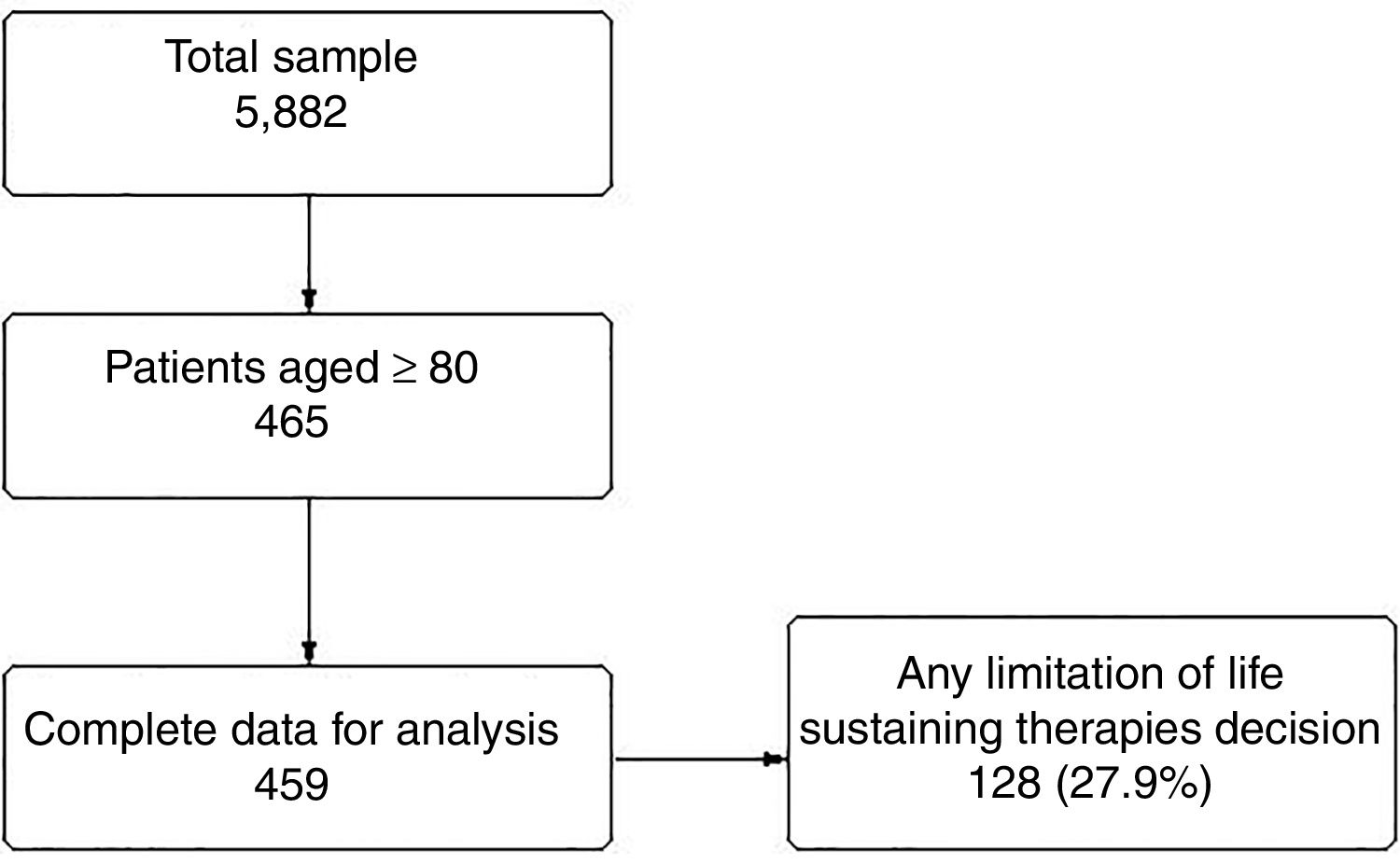
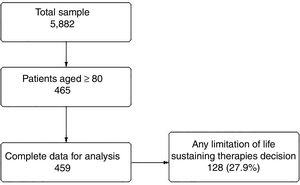
ResultsA total of 465 patients (8% of the whole sample) aged ≥80 years-old were included. Six patients were excluded from the final analysis because of incomplete data or unknown outcome at hospital discharge (Fig. 1).
Mean age was 83.4±3.3 years, being male 281 (60.4%). Antiplatelets or anticoagulants were prescribed previously in 271 patients (59.3%). The main mechanisms of injury were low-energy falls in 256 patients (55.1%) and road traffic accidents in 153 patients (33.3%). Trauma was blunt in 99% of the cases. Hemodynamic instability was found in 189 patients (41.2%). Unilateral mydriasis was found in 37 patients (8.1%) and bilateral mydriasis in 36 patients (7.8%).
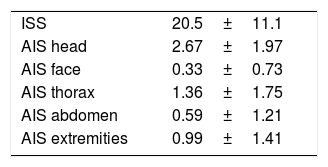
Mean ISS was 20.5±11.1. According to the AIS, the most severe injuries corresponded to the area of the head (Table 1). Up to 125 very elderly patients (27.3%) underwent urgent (<24h) surgical procedures, being the most frequent the neurosurgical interventions (57 out of 125 patients, 45.6% of the urgent surgeries performed).
Very elderly patients developed respiratory failure (paO2/FiO2<300) in 130 cases (28.3%) and required mechanical ventilation in 259 cases (56.4%). Tracheostomy was performed in 38 patients (8.3%). Different degrees of renal failure were found in 130 patients (28.3%) and only 11 patients (2.4%) were treated with continuous renal replacement therapy. Rhabdomyolysis was found in 52 patients (11.3%) and massive hemorrhage in 19 patients (4.1%). A total of 84 patients (18.1%) developed nosocomial infections and 70 patients (14%) developed multiorgan failure. Intracranial hypertension was found in 102 patients (22.2%).
Mean ICU length of stay was 7.45±9.9 days and mean length of hospital stay after ICU was 8.53±12.2 days.
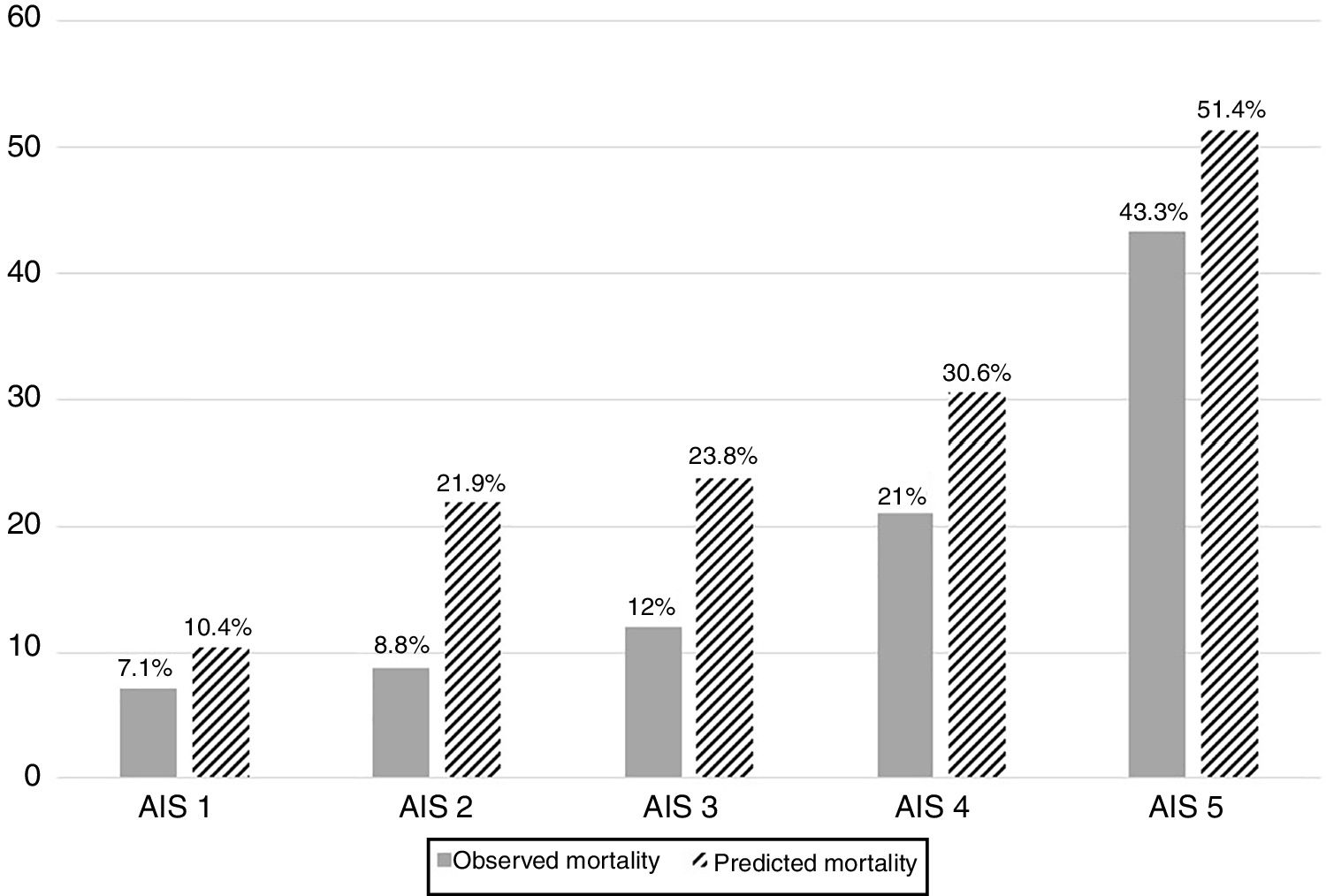
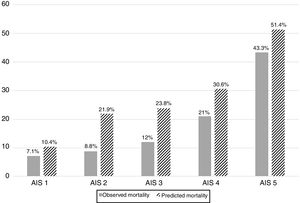
Probability of survival using the TRISS methodology was 69.8±29.7%. ICU mortality was 15.5% (71 patients). Hospital mortality after ICU was 3.7% (17 patients). Overall, in-hospital mortality was 19.2% (88 patients). The main reason was intracranial hypertension (42.7% of the cases). Multiple logistic regression analysis showed that the ISS (OR 1.02 95% CI 1.002–1.051, p=0.03), the need of first-tier measures to control intracranial pressure (OR 2.85 95% CI 1.143–7.142, p=0.02), the need of second-tier measures to control intracranial pressure (OR 4.56 95% CI 1.740–11.957, p=0.002) and being admitted to the ICU for intensive care oriented t organ donation (OR 6.61 95% CI 3.121–14.035, p<0.001) were independent predictors of death. Predicted and observed mortality distributed by severity of TBI is shown in Fig. 2.
Interestingly, 41 patients (9%) were admitted to the ICU for intensive care oriented to donation. Among them, 10 patients (24.4%) actually became organ donors. Additionally, 8 patients who received active ICU treatment also developed brain death and became effective organ donors.
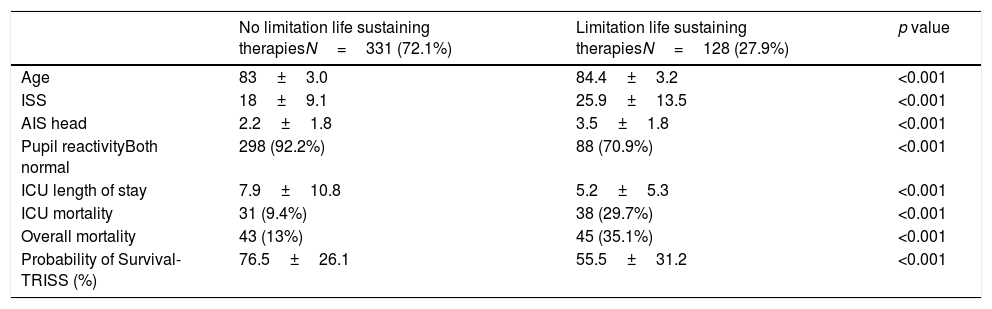
Limitation of life sustaining therapies occurred in 128 patients (27.9%). When distributing very elderly patients with or without LLST orders we found that patients with LLST were older, with higher severity of injury and with more severe brain injury, as stated by the number of patients with pupillary abnormalities and the AIS head score (Table 2).
Comparison of characteristics and outcomes of very elderly patients with and without limitation of life sustaining therapies.
| No limitation life sustaining therapiesN=331 (72.1%) | Limitation life sustaining therapiesN=128 (27.9%) | p value | |
|---|---|---|---|
| Age | 83±3.0 | 84.4±3.2 | <0.001 |
| ISS | 18±9.1 | 25.9±13.5 | <0.001 |
| AIS head | 2.2±1.8 | 3.5±1.8 | <0.001 |
| Pupil reactivityBoth normal | 298 (92.2%) | 88 (70.9%) | <0.001 |
| ICU length of stay | 7.9±10.8 | 5.2±5.3 | <0.001 |
| ICU mortality | 31 (9.4%) | 38 (29.7%) | <0.001 |
| Overall mortality | 43 (13%) | 45 (35.1%) | <0.001 |
| Probability of Survival-TRISS (%) | 76.5±26.1 | 55.5±31.2 | <0.001 |
The main result of our study was that very elderly trauma patients presented mortality rates were lower than predicted.
The observed mortality found in our series of very elderly trauma patients admitted to the ICU supports the initial aggressive acute care of these patients, as outlined in the Eastern Association for the Surgery of Trauma practice management guideline.7 Mock et al. recently published a single center study of 192 trauma ICU patients with a mean age of 86 years-old and mean ISS 17. Their patients had a 22% mortality rate, similar to that predicted by the Geriatric Trauma Outcome Score.11 The results are comparable to ours, in a less aged population (83.4 years-old) but with most severe trauma, as stated by the mean ISS 20.5. Mock et al. performed a multivariate analysis analyzing factors related to mortality and found that the need of mechanical ventilation, days on mechanical ventilation and admission lactate were independent predictors of outcome. In our series, the severity of injury evaluated by the ISS and specially, the burden of brain injury as demonstrated by the need of first- and second-tier measures to control ICP and being admitted to the ICU oriented to organ donation were independent predictors of death. Consequently, intracranial hypertension was the main cause of death. In the study by Hwabejire et al. including nonagenarian and centenarian patients with an ISS 12, independent predictors of cumulative 1-year mortality were head injury and length of hospital stay. Cumulative 1-year mortality in patients with head injury was 51.1% and increased to 73.2% if the ISS was 25 or higher and to 78.7% if mechanical ventilation was required.12 Our results are in consonance with previous studies in very elderly patients admitted in mixed ICUs.15 A recent prediction tool has been developed for medical ICU very elderly patents. Factors related with mortality were age, serum creatinine, Glasgow Coma Scale and serum pH.16 However, this prediction tool has not been validated in very elderly patients with severe trauma yet.
Controversy surrounding the ICU admission of very elderly patients exists.17,18 Our data support admitting these patients and perform an ICU trial. Thereafter, in non-responding trauma patients, LLST should be considered. In our sample, up to 27.9% of trauma patients over 80 years-old received LLST, a percentage very close to that found in a recent multicenter study in general ICU patients including trauma.19 In our study, LLST were more likely to occur in older patients, with higher severity of injury and with more severe brain injury, as stated by the number of patients with pupillary abnormalities and the AIS head score, similarly to the results found by Peñasco et al. in trauma patients ≥65 years-old.20
As known, TBI is a major concern in this population21 and plays a major role in outcomes, as seen in our series. However, neurosurgical interventions and modern neurointensive care have improved outcomes of geriatric TBI.22 In the series by Merzo et al., up to 55% of patients from 70 to 79 years-old and up to 30% of octogenarians with TBI had a favorable neurological outcome.23 Our results also point in this direction since mortality was markedly lower than predicted even in the group who received LLST. This can help to overcome past nihilism when approaching geriatric TBI, which was supported by the 60% mortality and more than 80% of severe neurological disability in patients aged >70 years-old reported by Hukkelhoven et al.23 and the ominous 6-month outcomes in moderate to severe geriatric TBI patients (none of them was living independently) shown by Utomo et al.24
Additionally, we must keep in mind the possibility that this group of patients might increase the pool of organ donors following the intensive care oriented to organ donation strategy.25,26 Up 9% of octogenarians were admitted to the ICU following this policy, but only 1 out of 4 among them finally developed brain death and became organ donors. Eight additional patients developed brain death after active ICU treatment. Overall, 3.9% of octogenarian trauma ICU patients were ultimately organ donors.
Our study has some limitations that must be acknowledged: the most important one is that our retrospective study is focused in survival rather than in quality of life and this is of special relevance in very elderly patients. In addition we did not take into consideration comorbidities or frailty, which are major determinants of different outcomes in this population,27 and we must acknowledge a selection bias, since we only studied octogenarians ICU patients and this may not represent the whole trauma octogenarian population. We did not evaluate predicted mortality using the specific Geriatric Trauma Outcome Score10 as did Mock et al. We used the conventional TRISS methodology since we previously compared the performance of the TRISS methodology and the Geriatric Trauma Outcome Score in our geriatric trauma ICU population and we found that the prediction ability of TRISS was higher, most likely due to severity of injury and the high percentage of patients with TBI.28 However, it must be considered that TRISS was created for a different population (younger patients with predominant high-energy mechanisms of injury), can be difficult to calculate and requires specific skills in the codification of injuries and continuous coefficient updates. Anyway, the mortality of our patients was markedly lower than predicted highlighting the need of newly geriatric-specific scores. Finally, when referred to the analysis of LLST, we did not differentiate between withholding or withdrawing therapies, and unfortunately, our registry cannot provide this information.
In conclusion, in Spanish ICUs, very elderly trauma ICU patients presented mortality rates lower than predicted by their severity of injury.
Author's contributionMario Chico-Fernández: Design of the study, collected data, critical review, approved the final version.
Marcelino Sánchez-Casado: Statistical analysis, critical review, approved the final version.
Jesús Abelardo Barea-Mendoza: Collected data, statistical analysis, critical review, approved the final version.
Iker García-Sáez: Collected data, critical review, approved the final version.
María Ángeles Ballesteros-Sanz: Collected data, critical review, approved the final version.
Francisco Guerrero-López: Collected data, critical review, approved the final version.
Manuel Quintana-Díaz: Collected data, critical review, approved the final version.
Ismael Molina-Díaz: Collected data, critical review, approved the final version.
Lorena Martín-Iglesias: Collected data, critical review, approved the final version.
José María Toboso-Casado: Collected data, critical review, approved the final version.
Jon Pérez-Bárcena: Collected data, critical review, approved the final version.
Juan Antonio Llompart-Pou: Design of the study, collected data, wrote the first and final draft, approved the final version.
FundingRETRAUCI was supported by a grant for the development of an electronic web-based system awarded to Dr. Chico-Fernández (Fundación Mutua Madrileña, reference number AP117892013).
PresentationA preliminary version of this manuscript was presented at the LIII CONGRESO NACIONAL SEMICYUC held in Granada, June 2018, obtaining the second prize in the “PREMIO DR. HELIODORO SANCHO RUIZ” to the best poster presentation.
Conflict of interestThe authors declare no conflict of interest.
The authors are indebted to Miguel Ángel Ferrero Fernández (Head of the IT Department SEMICYUC).