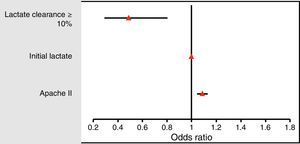
Sepsis is one of the leading causes of mortality worldwide.1 However, mortality rates widely vary among different countries when patients have been enrolled in prospective septic shock trials.2 For this and other reason, including sepsis recognition, new definitions of septic shock were launched. Now, shock is a clinical condition defined by a vasopressor requirement to maintain a mean arterial pressure of 65mm Hg or greater and serum lactate level greater than 2mmol/L (>18mg/dL) in the absence of hypovolemia.3 Our hypothesis is that lactate level is not sufficient for defining shock progression but timing within the first 24h of resuscitation. The aim of the present study is to determine the prognostic value of a predefined lactate clearance in the first 24h of sepsis. A total of 544 consecutive patients with sepsis were included from a tertiary University Hospital (Parc Tauli Hospital, Sabadell, Spain). The vast majority presented an abdominal (37.9%) or respiratory source of sepsis (31.3%) and 62.8% were admitted through emergency department. Patients presented were 66.6 (SD 14.8) years old, 63.2% male and presented an APACHE II score of 18.4 (SD 7.7) with a mortality rate of 29.8%. We calculated the optimal cutoff for a lower mortality during the first 24h of sepsis using the Youden index. With our data, this optimal cutoff was 10%, with a sensitivity of 51% and specificity of 71%. Patients with a lactate clearance≥10% within the first 24h of sepsis had a lower mortality in a univariate analysis than patients without that clearance (21.2% vs. 39.1%; p<0.001). We adjusted lactate clearance for confounding factors, as initial lactate value and severity (APACHE II score), and we observed that lactate clearance≥10% during the first 24h of sepsis was identified as a protective factor for mortality (OR 0.49: 95% CI 0.30–0.81; p<0.05) (Fig. 1). We, therefore, analyzed the relationship between lactate clearance and the fulfillment of the Surviving Sepsis Campaign (SSC) bundles. The group of patients with a lactate clearance≥10% trended toward a better fulfillment of SCC bundles (5.1% vs. 2.2%; p=0.12). We performed a multivariate analysis including all the SCC bundles (antibiotic treatment, fluid administration, vasopressors and initial lactate value and fluid administration) and lactate clearance≥10% (OR 6.41; 95% CI 2.01–20.45; p<0.05) was associated independently with a lower mortality. Despite the new incorporation of serum lactate levels for shock definition, we consider that the most important approach to reflect current ICU mortality would be the use of lactate clearance in the definition.4 Therefore, a personalized approach is lacking in the current definitions and a lactate clearance equal or greater than 10% within the first 24h of sepsis evolution is independently associated with lower mortality. Nguyen et al.5 discovered that early lactate clearance within the first 6h was associated with a decrease mortality however the 10% decrease was chosen after analyzing sensitivity and specificity of different thresholds. In our study, the implementation of a mathematical model (Youden index) helped us to find the “ideal threshold”. Interestingly, in accordance with recently published studies, in our cohort, fluid administration during the first hours of sepsis is independently associated with lactate clearance.6 Effort should be done to identify patients with shock and determinant of response, rather than to flag them only shocked.
FundingNone declared.
Conflict of interestThe authors have no conflict of interest to disclose.