To evaluate the effect of parenteral β-lactam antibiotics on outcomes related to ventilator-associated pneumonia (VAP) in adult patients in coma due to acute brain injury (ABI).
DesignSystematic review and meta-analysis.
SettingRandomized controlled trials (RCTs) published up toSeptember 30, 2024.
Patients or participantsAdult patients in coma due to ABI.
InterventionsParenteral β-lactam antibiotics.
Main variables of interestIncidence and outcomes related to VAP.
ResultsThree RCTs involving 483 patients met inclusion criteria; 231 patients received β-lactam prophylaxis. Among these, there were 115 cases of early-onset VAP (EO-VAP), 49 of late-onset VAP (LO-VAP), and 102 deaths. All studies were conducted in Europe. Causes of coma included trauma, stroke, and CO poisoning. Intravenous β-lactams (ampicillin/sulbactam, cefuroxime, and ceftriaxone) reduced EO-VAP risk by 57% (RR 0.43; 95% CI 0.30–0.61), and all-VAP by 35% (RR 0.65; 95% CI 0.53–0.80).
No impact was observed on LO-VAP (RR 0.95; 95% CI 0.54–1.67), 28-day mortality (RR 0.76; 95% CI 0.53–1.09), intubation duration (SMD -0.13; 95% CI −0.46–0.21), or ICU length of stay (SMD −0.22; 95% CI −0.55–0.12). Heterogeneity and the risk of bias were low, with high overall evidence certainty.
ConclusionsIn adult patients in coma due to ABI, intravenous β-lactam antibiotics reduce EO-VAP and all-VAP risk.
Evaluar el efecto de los antibióticos β-lactámicos parenterales en los resultados relacionados con la neumonía asociada a ventilación mecánica (NAV) en pacientes adultos en coma debido a lesión cerebral aguda (LCA).
DiseñoRevisión sistemática y metaanálisis.
ÁmbitoEnsayos controlados aleatorizados (ECA) publicados hasta el 30 de septiembre de 2024.
Pacientes o participantesPacientes adultos en coma debido a LCA.
IntervencionesAntibióticos β-lactámicos parenterales.
Variables de interésprincipalesIncidencia y desenlaces relacionados con la NAV.
ResultadosIncluimos tres ECA, 483 pacientes, de los cuales, 231 recibieron profilaxis con β-lactámicos. Hubo 115 casos de NAV de inicio temprano (NAV-IT), 49 de NAV de inicio tardío (NAV-ITD) y 102 muertes. Todos los estudios se realizaron en Europa. Las causas de coma incluyeron traumatismo, accidente cerebrovascular e intoxicación por CO. Los β-lactámicos intravenosos (ampicilina/sulbactam, cefuroxima y ceftriaxona) redujeron el riesgo de NAV-IT en un 57% (RR 0,43; IC 95% 0,30–0,61), y de NAV total en un 35% (RR 0,65; IC 95% 0,53–0,80).
No se observó impacto en NAV-ITD (RR 0,95; IC 95% 0,54–1,67), mortalidad a 28 días (RR 0,76; IC 95% 0,53–1,09), duración de la intubación (DMS -0,13; IC 95% -0,46–0,21) o estancia en UCI (DMS -0,22; IC 95% -0,55–0,12). La heterogeneidad y el riesgo de sesgo fueron bajos, con una alta certeza en la evidencia.
ConclusionesEn pacientes adultos en coma debido a LCA, los antibióticos β-lactámicos intravenosos reducen el riesgo de NAV-IT y de NAV total.
Ventilator-associated pneumonia (VAP), defined as pneumonia that develops within 48 h after invasive mechanical ventilation (IMV),1 remains the leading cause of nosocomial and healthcare-associated infections in intensive care units (ICUs).2 VAP is linked to several adverse outcomes, including increased days of IMV, prolonged ICU and hospital stays, higher healthcare costs, infections with multidrug-resistant (MDR) pathogens, and increased morbidity and mortality.2–4
Early-onset VAP (EO-VAP), presenting within the first five days of hospitalization, is typically caused by antibiotic-susceptible bacteria and is associated with a better prognosis. In contrast, late-onset VAP (LO-VAP), occurring five days or more after admission, is more likely to involve MDR pathogens and carries a higher risk of morbidity and mortality.5–7 Patients in coma due to acute brain injury (ABI), regardless of the cause, are at a high risk of EO-VAP.2,8,9 In these patients, EO-VAP develops primarily due to microaspirations caused by glottic dysfunction.10 VAP is particularly concerning in acute neurological patients, as it is associated with higher mortality rates.11,12 Evidence from a meta-analysis indicates that preventive antibiotic therapy may reduce the incidence of infections in patients with acute stroke from 36% to 22%. However, it does not significantly affect the number of dependent or deceased patients.12 On the other hand, another meta-analysis found that antibiotic prophylaxis following cardiac arrest did not improve survival rates, neurological outcomes, critical care length of stay, or the incidence of pneumonia.13
To date, at least four meta-analyses have explored the role of prophylactic antibiotics in preventing VAP in patients in coma due to ABI. Although these studies arrive at similar conclusions, their significant clinical and methodological heterogeneity limits the comparability and generalizability of their findings.14–17 Most of these studies combined randomized clinical trials (RCTs) with non-randomized or observational studies,14–17 included different routes of administration (respiratory tract,14,15,17 intrathecal,15 or intravenous15,16), and examined antibiotic families14–17 making their conclusions challenging to apply universally.
Therefore, to clarify the role of antibiotic prophylaxis in patients in coma due to ABI, our study aims to conduct a systematic review focusing exclusively on studies with similar designs, involving comparable populations, subjected to similar interventions, and evaluating the same outcomes. The conclusions of this study are particularly relevant given the implications of acute brain injury as a risk factor for VAP and the critical importance of addressing VAP to reduce morbidity and mortality in these critically ill patients.
Materials and methodsThis systematic review adheres to the recommendations outlined in the Cochrane Handbook for Systematic Reviews,18 PRISMA,19 and AMSTAR 220 guidelines. We registered the protocol in PROSPERO (CRD42024506628).
Search strategyWe comprehensively searched five databases: MEDLINE (PubMed), Scopus, EMBASE, Web of Science, and Google Scholar. We screened each database using controlled language terms (MeSH, Emtree, etc.), free terms, and their synonyms, combined with Boolean operators, following a PICO strategy: Patients or participants: adult patients in coma due to ABI; Interventions: parenteral β-lactam antibiotics; Comparator: placebo or usual care; Outcomes: incidence and outcomes related to VAP. Keywords primarily focused on exposure, such as "β-lactams antibiotics" OR "ampicillin/sulbactam" "piperacillin/tazobactam" OR "ceftriaxone" OR "cefuroxime" OR "cefotaxime" OR "ceftazidime" OR "cefepime" OR "cefixime" OR "ceftaroline"; and outcome-related terms such as "ventilator-associated pneumonia" OR "early-onset ventilator-associated pneumonia" OR "late-onset ventilator-associated pneumonia." Additionally, we performed manual secondary searches of references in relevant studies and review articles. There were no restrictions on language or publication year. The search strategy is provided in the Supplementary materials, Table S1.
Inclusion and exclusion criteriaWe searched for randomized controlled trials (RCTs) published from inception until July 31, 2024. We excluded case reports, case series, and observational studies. All articles retrieved from the primary and secondary searches were compiled using Mendeley® 2.119.0. After removing duplicates, these documents were imported into the Rayyan® tool, screened, and individually examined by four blinded and independent researchers (MOP, MGAR, CGFN, and GAVT). All articles that were collected were evaluated using the terms of the PICO strategy and the inclusion and exclusion criteria.
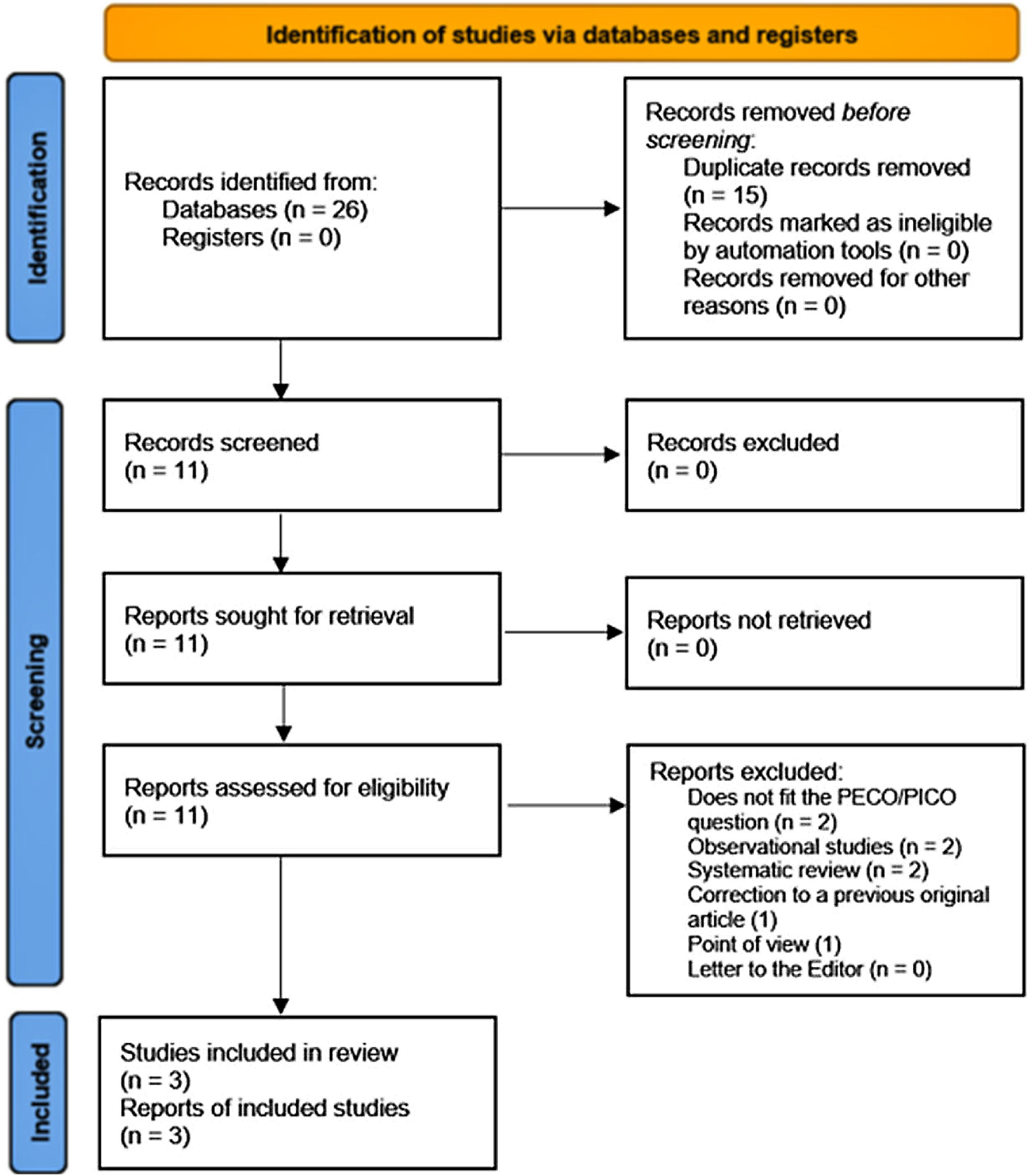
Study selection and data extractionThe selected articles were exported to a spreadsheet for a second full-text screening. The study selection process is provided in Fig. 1. The same four blinded, independent researchers who performed the selection process also performed data extraction, examining articles, and collecting relevant details of each study, including the authors, country and year of publication, clinical and epidemiological characteristics of the population, the intervention (the type, dose, and duration of the β-lactams antibiotic used), the outcome and comparator (the number of events), the measures of association, confounding factors, and other relevant findings. Data from each paper were extracted and recorded in a spreadsheet. The initial screening of studies, the selection, and data extraction were made by consensus among the researchers, and in case of disagreement, the lead researcher served as the arbitrator (EDMR).
Data synthesis, meta-analysis, and meta-regressionThis meta-analysis was performed using R® 4.2.226. We used the generic inverse variance method (GIVM) with restricted maximum likelihood (REML) for tau2,21 and Hartung-Knapp adjustment for random effects model studies.21–23 For dichotomic outcomes, we pooled risk ratios (RRs), and for continuous outcomes, bias-corrected standard mean difference (SMDs) using exact formulae (Hedges’ g)21 and variances with their 95 percent confidence interval (95% CI). Since statistical heterogeneity among studies was not statistically significant (Cochran’s Q test and p > 0.10, Higgins I2 statistics <40%), we used a fixed effects model.18 Since we had few studies, we did not perform subgroup analysis, funnel plots, and trim-and-fill analysis. However, we conducted sensitivity, leave-one-out influence analyses, and meta-regression to assess heterogeneity, and we evaluated the publication bias.21
Risk of bias assessmentWe assessed the risk of bias using version 2 of the Cochrane risk-of-bias tool for randomized trials (ROB 2).24
GRADE assessmentWe assessed the certainty of the evidence (CoE) of the primary outcomes according to the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) criteria.25,26
ResultsWe identified 26 records, all retrieved from databases. After removing 15 documents, 11 reports remained. Subsequently, these 11 reports were assessed for eligibility. Of these studies, eight were excluded. Two reports were systematic reviews, two were observational studies, two did not meet our PICO question, one was a point of view, and one was a correction to a previous original article (Supplementary materials, Table S2). Finally, three papers, all RCTs, were included in our systematic review (Fig. 1 and Table 1).
General characteristics of included studies.
| Study, Participants, and Interventions | Outcome and other essential findings |
|---|---|
| Dahyot-Fizelier et al.8 2024, France. PROPHY-VAP: a multicenter, double-blinded RCT conducted in 9 ICUs in 8 French hospitals. From October 2015 to May 2020. Patients ≥18 in coma (GCS ≤ 12). of both sexes. Inclusion criteria: brain trauma, ischemic or hemorrhagic stroke, and SAH. Exclusion criteria: tumor, infectious disease, cardiac arrest; high risk of death within the first 48 h after admission; ongoing antibiotic treatment; previous hospitalization within the past month; antibiotic prophylaxis expected within the first 24 h after randomization; ETI by nasal route; subglottic secretion drainage; MV on tracheostomy; etc.Patients were randomly assigned (1:1) stratified by center and severity of unconsciousness at the time of inclusion (GCS < 8 or ≥8) to account for differences in patient treatment between centers and heightened VAP risk in patients with GCS < 8. Enrolled patients received a single 30-minute. IV administration of ceftriaxone 2 g or saline once within the 12 h following ETI. Participants did not receive selective oropharyngeal and digestive tract decontamination. | Primary outcome: EO-VAP from the 2nd to the 7th day of MV (ATS definition). Secondary outcomes at discharge from ICU or day 28 if the patient was still in the ICU: LO-VAP (>7 days after ETI) or VAP regardless of the time of occurrence; type of microorganism-induced VAP; exposure to MV and antibiotics (number of ventilator-free or antibiotic-free days); ventilator-associated events according to the CDC definition; comparison with global incidences of VAP according to the ATS and CDC definitions; the time between inclusion and the first spontaneous ventilation test; the proportion of patients with the digestive acquisition of ESBL-producing Enterobacteriaceae; neurological outcome according to the MRS and GOS; mortality; and safety. Secondary outcomes at day 60 were: exposure to ICU and hospital (number of ICU-free and hospital-free days); neurological outcome according to the MRS and GOS; and mortality. N = 345 patients were randomly assigned (1:1) to receive ceftriaxone (n = 171) or placebo (n = 174); 330 received the allocated intervention, and 319 were included in the analysis (162 in the ceftriaxone group and 157 in the placebo group). The analysis's 166 (52%) participants were men, and 153 (48%) were women. After randomization, 15 patients did not receive the allocated intervention, and 11 withdrew their consent. Ninety-three cases of VAP, including 74 early infections. The incidence of EP-VAP was lower in the ceftriaxone group than in the placebo group (23 [14%] vs. 51 [32%]; HR 0.60 [95% CI 0.38–0.95], p = 0.030), with no microbiological impact and no adverse effects attributable to ceftriaxone. On day 28, there were 12 patients with late VAP in the ceftriaxone group and 7 cases in the placebo group. Those receiving ceftriaxone were at lower risk of developing all types of VAP (20% vs. 36%; HR 0.62 [0.42–0.98]); incidences of LO-VAP were similar between groups. Mortality was 32 (20%) of 161 patients receiving ceftriaxone versus 46 (30%) of 157 receiving placebo (HR 0.66 [0.42–1.04], p = 0.074. |
| Acquarolo et al.28 2005, Italy. Single center, prospective, open-label, RCT. From September 2001 to October 2002. Adult patients (≥18 y.), in coma (GCS ≤ 8) MV patients. Inclusion criteria: head trauma, SAH, cerebral hemorrhage, cardiac arrest, ischemic stroke, and CO poisoning. Exclusion criteria: pneumonia or pulmonary contusion on admission to the ICU; antibiotics administration in the previous 48 h; multiple trauma; clinical indication to antibiotic prophylaxis or treatment (i.e., open craniocerebral wound or extensive soft tissue facial lesion); an estimated duration of MV or coma of <48 h; hopeless prognosis; immunocompromised; and pregnancy. Patients were randomly assigned to receive either AS (3 g every 6 h for 3 days) plus standard treatment or standard treatment alone. Patients in the standard treatment group did not receive a placebo. AS was started in all cases within 6 h of ICU admission. Patients in the standard treatment group did not receive antibiotics in the first 3 ICU days unless it was clinically dictated. Physicians and paramedics were not blinded to treatment allocation; the outcome adjudicators and the data analysts were. | VAP was defined as pneumonia occurring >48 h after ETI and initiation of MV. EO-VAP was defined as VAP occurring during the first 4 days of MV, whereas LO-VAP was defined as VAP developing ≥5 days after the initiation of MV. EOP was suspected if a new and persistent CXR infiltrate was associated with one of the following criteria: (1) purulent tracheobronchial secretions; (2) fever > 38.3 °C or hypothermia; (3) leukocytosis or leucopenia (>10,000/mm3 and, respectively, <5000/mm3). EO-VAP was confirmed by the isolation of a potentially pathogenic microorganism from bronchoscopic BAL (>104 CFU/mL) or non-bronchoscopic protected mini-BAL (>104 CFU /mL). All patients had CXR examination and pulmonary secretion sample taken with bronchoscopic BAL or non-bronchoscopic protected mini-BAL immediately after enrollment into the study and then every 48 h or more frequently if clinically indicated for the first 5 ICU days. N = 38. Males: 12 (63.2%) in the standard treatment group and 13 (68.4%) in the experimental group. Mean age: 54.6 ± 17.7 years in the standard treatment group and 54.8 ± 18.0 years in the experimental group. 15 of 38 patients (39.5%) developed EO-VAP; 11 (57.9%) in the standard treatment group and 4 (21.0%) in the AS group. There were 19 LO-VAP episodes (50.0%), 9 (47.4%) in the standard treatment group, and 10 (52.6%) in the AS. In standard treatment, the mean number of days of MV was 10.6 ± 9.4 days, whereas, in the AS group, the mean number of days of MV was 9.9 ± 6.9 days. In the standard treatment, the mean ICU stay was 12.6 ± 9.7 days, while, in the AS group, the mean ICU stay was 12.8 ± 8.7 days. In standard treatment, there were 8 (42.1) events of ICU mortality, while, in the AS group, there were 7 (36.8) events of ICU mortality. The two groups were also comparable in terms of the duration of mechanical ventilation (t = 0.3431, p = 0.7355, duration of ICU stay (t = −0.1070, p = 0.9160, and ICU mortality (p = 0.740). |
| Sirvent et al.27 1997, Spain. Single center, open-label RCT. Between June 1, 1992, and September 31, 1994 (28 mo).Patients in coma (GCS ≤ 12). Inclusion criteria: head injury, medical stroke, or undergoing surgery for space-occupying head lesions. The time lapse between ETI and the beginning of the study protocol was <6 h in all cases. All patients were put on ETI and MV > 72 h. Upon hospital admission, all patients were included in the study and did not receive antibiotics before entry. Patients enrolled in the study were free from pulmonary infection and did not present suspicion of gross aspiration into lower airways at the time of inclusion. Exclusion criteria: immunosuppression, HIV infection, parenteral drug addicts, transplanted, hematologic malignancies, insulin-dependent DM, CKD, CLD, COPD, etc. Patients were randomly assigned to a prophylaxis group (IV cefuroxime group: two 1500-mg doses 12 h apart after intubation) or a control group. Each group had 50 patients. Patients did not receive any other antibiotics before the endpoint determination. Control Group: These subjects did not receive cefuroxime for prophylaxis. | The diagnosis of VAP was confirmed by isolating a pathogenic microorganism from the blind-protected BAL specimen in counts ≥104 CFU/mL. During the first 24 h of admission, endotracheal aspirate samples were obtained using sterile tubes from all patients. Non-bronchoscopic protected BAL was done on the day of the suspicion of VAP. In addition, blood cultures and serology were performed on all patients who developed pulmonary infections. EOP was diagnosed when VAP developed within the first 4 d of MV. LOP was defined as pneumonia developing after the fourth day of MV.The global incidence of microbiologically confirmed VAP was 37% (n = 37); 12 (24%) belonged to the cefuroxime group, and 25 (50%) belonged to the control group (p = 0.007). EO-VAP accounted for 70% of all the VAP episodes (n = 26), eight (67%) belonging to the cefuroxime group, and 18 (72%) belonging to the control group (p = 0.02). In the control group, four of 17 (23%) patients receiving prior antibiotics developed VAP, whereas 21 of 33 (64%) patients who did not receive antibiotics developed VAP (p = 0.016). The multivariate analysis revealed that the duration of MV (per day) was an independent risk factor significantly associated with VAP development. Furthermore, before the VAP episode, cefuroxime or prior antibiotics in the control group had a protective effect against its development.No difference in mortality and morbidity was found when comparing the study population with the control group. Nevertheless, when comparing patients with VAP (from both study and control groups) with those without it, there was a decrease in total hospital stay (35 ± 13 vs 25 ± 14 d, p = 0.048) and ICU stay (20 ± 11 vs 11 ± 7 d, p = 0.001). This study demonstrated that the administration of two single high doses of 1500 mg each of cefuroxime after the intubation of patients in coma due to head injury or medical stroke is an effective prophylactic strategy to decrease the incidence of VAP. |
RCT: randomized controlled trial, MV: mechanical ventilation, VAP: ventilator-associated pneumonia, EOP: early-onset VAP, LOP: late-onset VAP, AS: ampicillin-sulbactam, ICU: intensive care units, GCS: Glasgow Coma Scale score, IV: intravenous, ETI: endotracheal intubation, ITT: intention-to-treat, ICU: intensive care unit, CDC: Centers for Disease Control and Prevention, MRSA: methicillin-resistant S. aureus, CKD: chronic kidney disease, CLD: chronic liver diseases, COPD: chronic obstructive pulmonary disease, CXR: chest X rays, BAL: bronchoalveolar lavage, CDC: Centers for Disease Control and Prevention, MRS: modified Rankin scale, GOS: Glasgow Outcome Scale, SAH: subarachnoid hemorrhage.
This review includes 483 patients, of which 231 received any β-lactam prophylactic antibiotic, 115 cases of EO-VAP, 49 cases of LO-VAP, and 102 deaths (Table 1). All three studies were conducted in Europe (Spain, France, and Italy). The studies were conducted from June 1992 to May 2020. The patient follow-up period varied from 60 days to 28 months. We only included articles that reported adjusted effect size and a control group. In 2 studies, the definition of coma based on the Glasgow Coma Scale (GCS) was ≤12.8,27 In contrast, the other study used an ECG ≤ 8 to define coma.28 The most common causes of coma in patients included brain trauma, ischemic or hemorrhagic stroke, and CO poisoning. Cardiac arrest was an inclusion criterion in one study28 and an exclusion in another.8 Similarly, undergoing surgery for space-occupying head lesions was a criterion of inclusion in one study27 and exclusion in another.8 Each included study used a different antibiotic in the experimental group: ceftriaxone,8 ampicillin/sulbactam,28 and cefuroxime.27
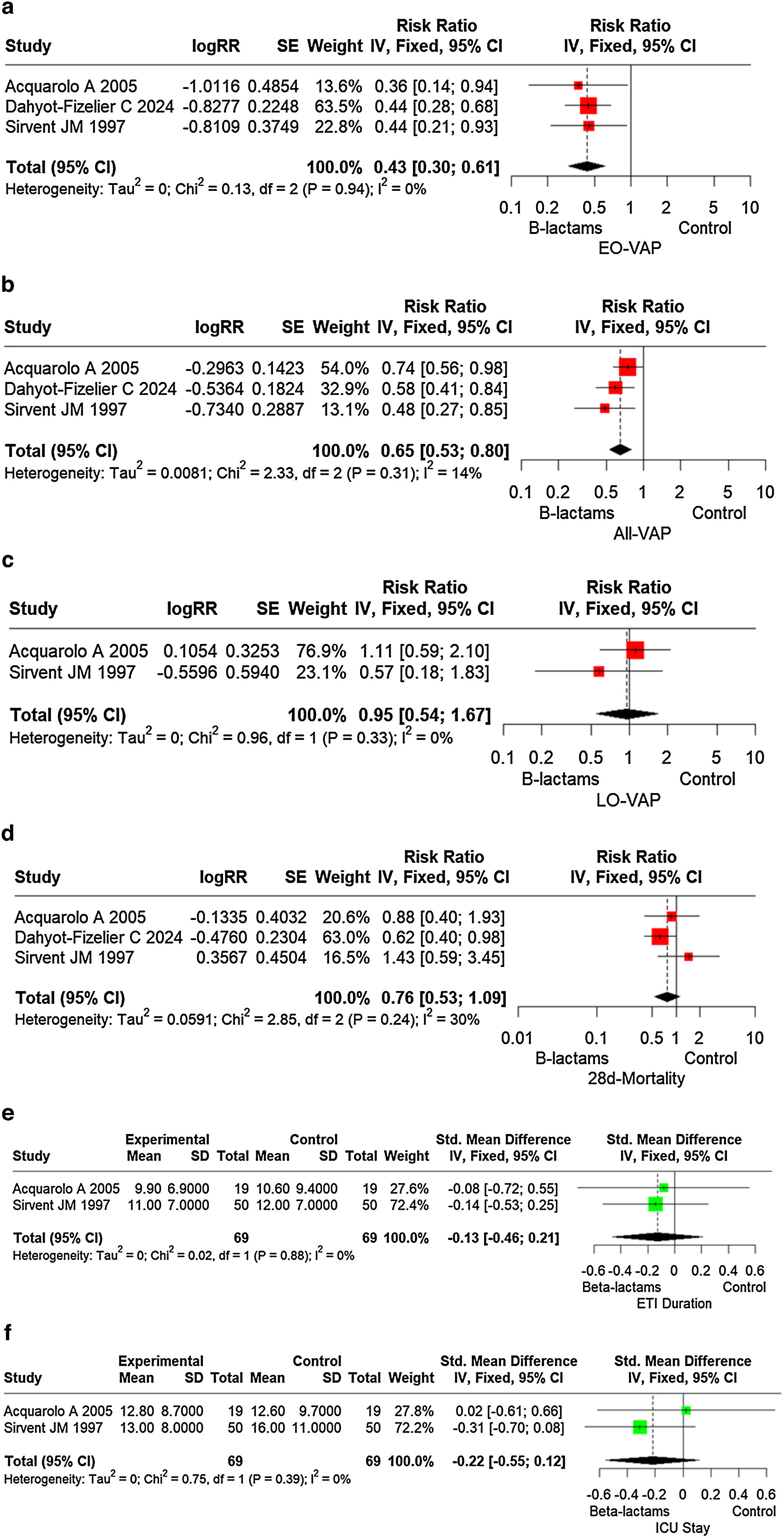
Effect of β-lactams antibiotics to prevent ventilator-associated pneumonia (VAP) and mortalityAccording to our findings, in patients in coma due to ABI, β-lactams antibiotics (ampicillin/sulbactam, cefuroxime, and ceftriaxone) reduce the risk of early-onset VAP (EO-VAP) by 57% (RR 0.43; 95% CI 0.30–0.61) (Fig. 2a) all (early and late) ventilator-associated pneumonia (all-VAP) by 35% (RR 0.65; 95% CI 0.53–0.80) (Fig. 2b). However, β-lactams antibiotics do not prevent late-onset ventilator-associated pneumonia (LO-VAP) (RR 0.95; 95% CI 0.54–1.67) (Fig. 2c). Similarly, β-lactams antibiotics did not reduce 28 day-mortality in 56 patients in coma due to ABI (RR 0.76; 95% CI 0.53–1.09) (Fig. 2d). We could not meta-analyze 60-day mortality because only one study8 assessed this outcome.
(a) Forest plot of the effect of β-lactams antibiotics to prevent early onset ventilator-associated pneumonia (EP-VAP) in patients in coma due to acute brain injury. (b) Forest plot of the effect of β-lactams antibiotics to prevent all (early and late) ventilator-associated pneumonia (ALL-VAP) in patients in coma due to acute brain injury. (c) Forest plot of the effect of β-lactams antibiotics to prevent late-onset ventilator-associated pneumonia (LO-VAP) in patients in coma due to acute brain injury. (d) Forest plot of the effect of β-lactams antibiotics on 28 day-mortality in patients in coma due to acute brain injury. (e) Forest plot of the effect of β-lactams antibiotics on duration of endotracheal intubation (ETI). (f) Forest plot of the effect of β-lactams antibiotics on duration of ICU stay.
Our findings suggest that in patients in coma due to ABI, β-lactams antibiotics (ampicillin/sulbactam, cefuroxime, and ceftriaxone) do not affect the duration of endotracheal intubation (ETI) (SMD −0.13; 95% CI −0.46–0.21) (Fig. 2e).
Effect of β-lactams antibiotics on hospital stayOur findings show that in patients in coma due to ABI, β-lactams antibiotics did not impact the duration of ICU stay (SMD −0.22; 95% CI −0.55–0.12) (Fig. 2f).
HeterogeneityStatistical heterogeneity was not significant for all the outcomes assessed (I2 <40%, p > 0.10).18 Likewise, the sensitivity and leave-one-out influence analyses did not suggest any significant impact of heterogeneity on the overall estimate. In meta-regression, the moderators' test was not statistically significant according to the country of publication of the study (France, Italy, or Spain) (QM = 0.13, p = 0.94) or year of publication of the study (1997, 2005, 2024) (QM = 0.01, p = 0.93). That is, none of these moderators accounted for between-study heterogeneity. Similarly, the test for residual heterogeneity was also not statistically significant for any of these variables (QE = 0.00, p = 1 and QE = 0.12, p = 0.73, respectively), suggesting that our model was well specified. Then, no other moderating variables would be considered in our model (Supplementary materials, Table S3).
Publication biasBecause our meta-analysis only included three studies, we do not show a funnel plot. However, Egger’s test did not show a risk of publication bias (z = −0.26, p = 0.80). Likewise, considering a reference or threat criterion (5 × k + 10 = 25), the Rosenthal approach (observed significance level p < 0.0001, target significance level p = 0.05, Fail-safe N = 51) and the Rosenberg approach (observed significance level p < 0.0001, target significance level p = 0.1, Fail-safe N = 62) suggested that publication bias was not a threat to the existence of a significant effect size in this meta-analysis.
Risk of biasAll included studies had a low risk of bias (Supplementary materials, Figures S1a and S2).
GRADE assessmentWe upgraded the level of CoE as all the studies included had a low risk of bias. Indirectness (the included studies compared similar interventions, similar populations, and similar outcomes), imprecision (this review consists of 483 patients, of which 115 cases of EO-VAP, 49 events of LO-VAP, and 102 deaths), publication bias, and inconsistency (I2 < 40%) did not impact significantly the CoE. Therefore, the overall CoE was considered high (Supplementary materials, Table S4).
DiscussionTo our knowledge, this is the first meta-analysis that includes only RCTs and examines the effect of exclusively β-lactam antibiotics on clinical outcomes related to VAP in patients in coma due to ABI. Our findings show that in patients in coma due to ABI, intravenously β-lactam antibiotics (ampicillin/sulbactam, cefuroxime, and ceftriaxone) decrease the risk of EO-VAP by 57% and all-VAP by 35%.
Until today, four other meta-analyses have investigated the role of prophylactic antibiotics in preventing VAP in unconscious patients due to diverse causes. While all these studies generally concluded that antibiotics could reduce the rates of VAP, the significant clinical and methodological heterogeneity among them limits the comparability and generalizability of their findings.14–17 For example, most of these studies combined different study designs (experimental and observational studies),14–17 included various routes of administration (respiratory tract,14,15,17 intrathecal,15 or intravenous15,16), and examined multiple antibiotic families14–17 making it challenging to apply their conclusions universally. Due to these limitations, we considered that the studies by Póvoa et al.14 and Falagas et al.17 are less comparable to our meta-analysis.
Righy et al.16 conducted a meta-analysis to evaluate systemic antibiotic administration’s effectiveness in VAP prevention in patients in coma. They searched for studies in patients aged >16 that assessed the impact of systemic antibiotics at the time of intubation on EO-VAP compared to placebo or no prophylaxis. They included three studies (two RCTs and a cohort study) with 267 patients, most of them were in coma due to head trauma. They found that systemic antibiotic administration was associated with decreased incidence of EO-VAP and a shorter ICU length of stay, but did not affect mortality or duration of MV. The authors recommended conducting future trials to confirm these findings. Some aspects of this meta-analysis16 deserve special attention. However, the authors stated that "there was no heterogeneity among the studies in the main outcomes"; one of the outcomes reported (duration of MV) had a significant heterogeneity (I2 = 47.1%). Furthermore, in one of the included studies, the experimental group was a prospective cohort study, but the control group was a historical cohort. Additionally, the researchers administered various intravenous antibiotics, such as ceftriaxone, ertapenem, or levofloxacin, to the intervention group 16.
Zha et al.15 conducted a network meta-analysis to compare the efficacy and safety of antibiotic prophylaxis in preventing VAP in an invasive MV (IMV) population in ICUs. They searched four databases and included 13 studies comprising 2144 patients remained. Of those 13 studies, 9 were RCTs, and 4 were cohort studies. The prophylactic antibiotic used, the dose, time, and the route of administration also varied widely among the studies. For example, nebulizing colistin for ten days,29 nebulizing ceftazidime for seven days,30,31 endotracheal injection of gentamicin until extubation,32,33 intravenous amoxicillin/clavulanate,34 ampicillin/sulbactam,28 or piperacillin/tazobactam35 daily for 1–3 days, intravenous cefuroxime for 3.5 days,27 intratracheal colistin for 15 days,36 intratracheal tobramycin from intubation to extubation 37, and intravenous ceftriaxone for single dose.38,39 The researchers reported that prophylactic antibiotic treatment resulted in a lower VAP rate compared to control groups but did not reduce mortality. Notably, despite significant heterogeneity among the studies regarding VAP incidence (I2 = 53%), the authors employed a fixed-effects model.
In addition to these crucial considerations mentioned above, these two meta-analyses15,16 share a critical methodological limitation: the combination of clinical trials and observational studies within a meta-analysis. The primary concern lies in the differences in study quality and design. Clinical trials typically provide more rigorous control over variables and minimize bias, offering reliable causal conclusions. In contrast, observational studies are more susceptible to biases and confounding factors, which can compromise the validity of their findings. Combining these two study types can dilute the scientific rigor of clinical trials, introduce significant heterogeneity, and result in less precise or potentially biased conclusions.18,40
This study has limitations, most of them derived from the scarce number of included studies: 1) We did not perform subgroup analysis, although this was not strictly necessary, because heterogeneity was not significant; 2) We did not examine the impact of multi-drug resistant bacteria on the primary clinical outcomes because this variable was not considered in most of the included studies between the intervention and control groups; 3) The timespan from the first to the most recent study was broad (27 years); therefore, there was a chance that evolution of critical care has impacted on clinical outcomes; however, meta-regression suggested that this was not the case.
Our study has limitations, most of them derived from the scarce number of included studies: 1) We did not perform subgroup analysis, although this was not strictly necessary, because heterogeneity was not significant; 2) We did not examine the impact of multi-drug resistant bacteria on the primary clinical outcomes because this variable was not considered in most of the included studies between the intervention and control groups; 3) The timespan from the first to the most recent study was broad (27 years); therefore, there was a chance that evolution of critical care has impacted clinical outcomes; however, meta-regression suggested that this was not the case; 4) Among the three RCTs included, the studies by Sirvent et al. and Dahyot-Fizelier et al. were the most relevant due to their larger sample sizes and the fact that prophylaxis did not exceed 24 h. In contrast, the study by Aquarolo et al. was less relevant due to its smaller sample size and the use of a broad-spectrum and potent beta-lactam (ampicillin-sulbactam) for three days, which may have introduced additional variability into the pooled results.
Conversely, our study also has significant strengths: 1) our search strategy was broad; 2) we included more recent studies than any other previous review; 3) we only included RCTs —not observational studies—assessing the effect of a single-family (β-lactams) of antibiotics administered by a unique route of administration (intravenously) compared to an adequate control group; 4) the clinical and statistically homogeneity among the studies was significant; and 5) risk of bias and publication bias was insignificant. Therefore, our results are more robust and rigorous than any previous meta-analysis examining similar outcomes and have a high level of evidence.
ConclusionsThis meta-analysis of RCTs shows that in adult patients in coma due to ABI, intravenous prophylaxis with a β-lactam antibiotic (ampicillin/sulbactam, cefuroxime, and ceftriaxone) reduces the risk of EO-VAP and all-VAP. However, this prophylaxis does not reduce mortality or the overall length of ICU stay. We emphasize the high certainty of evidence supporting our findings, though further evidence from well-conducted RCTs is still needed.
Supplementary materials: Table S1: Search strategy; Table S2: Excluded studies; Table S3: Meta-regression analysis of the studies included in the metanalysis; Table S4: GRADE assessment. Figure S1: Risk of bias assessment according to the domain of the Cochrane ROB2 tool. Figure S2: Traffic-light plots risk of bias assessment according to the study and domain using the Cochrane ROB2 tool.
CRediT authorship contribution statementEDMR: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing–original draft, Writing–review & editing. MOP: Data curation, Methodology, Validation, Visualization, Writing–review & editing. MGAR: Data curation, Methodology, Resources, Visualization, Writing–review &editing. CGFN: Conceptualization, Data curation, Investigation, Methodology, Resources, Software, Validation, Visualization, Writing–original draft, Writing-review & editing. GAVT: Methodology, Validation, Visualization, Writing-review & editing. All authors accepted the final manuscript.
FundingThe authors declare that we have not received any funding for the preparation of this work.
Data availability statementThe protocol is available at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=506628 (accessed on September 25, 2024).