A 20-year-old woman without any past medical issues suffered cardio-respiratory arrest in the street. Resuscitation maneuvers were performed for 40min, regaining normal cardiac function. During resuscitation, the patient was intubated using direct laryngoscopy, and airway was clear and unobstructed. Ten minutes after the intubation, however, a large quantity of foamy, serohemorragic fluid emerged from the endotracheal tube.
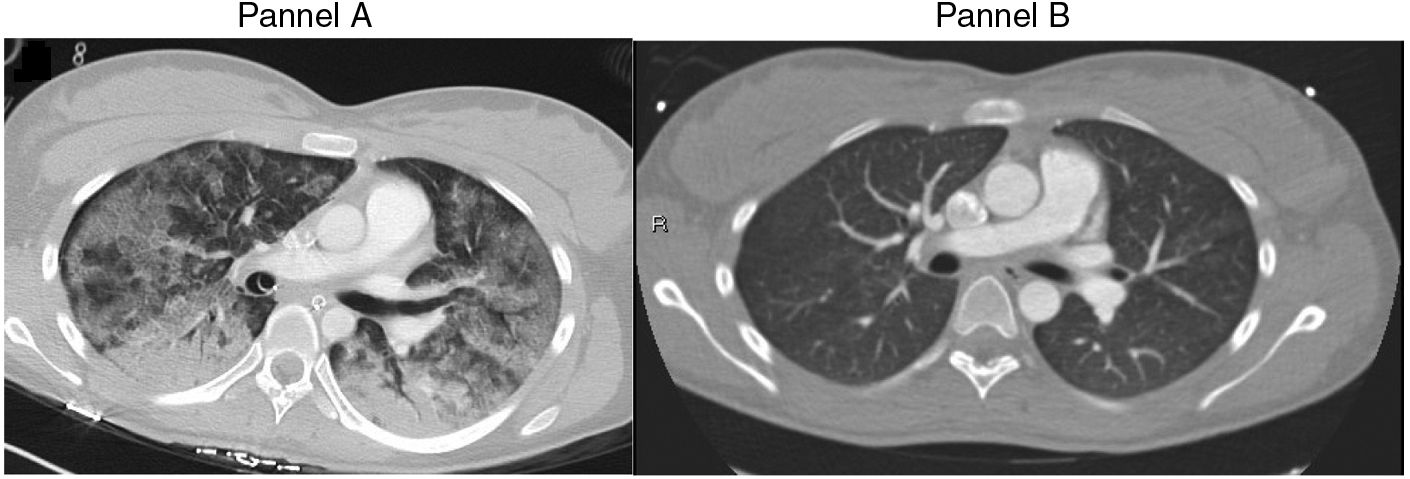
A CT scan was obtained immediately after arrival to the hospital, showing areas of ground-glass opacification and bilateral alveolar infiltrates (Fig. 1A). Given the results, urgent fibrobronchoscopy was performed, revealing bilateral alveolar hemorrhage in pulmonary bases, whilst the bronchial tree was clear. Autoimmune studies were negative. The patient showed good oxygenation and CO2 exchange. Twelve days after the cardio-respiratory arrest, a coronary angio-CT was obtained, which ruled out coronary disease as a cause for the arrest. The patient was subsequently diagnosed with wide QT syndrome. In the coronary angio-CT scan, pulmonary parenchyma was normal, with no signs of active hemorrhage or residual blood (Fig. 1B). In the light of these findings, the alveolar hemorrhage was attributed to the cardiac massage received during the cardio-respiratory arrest.