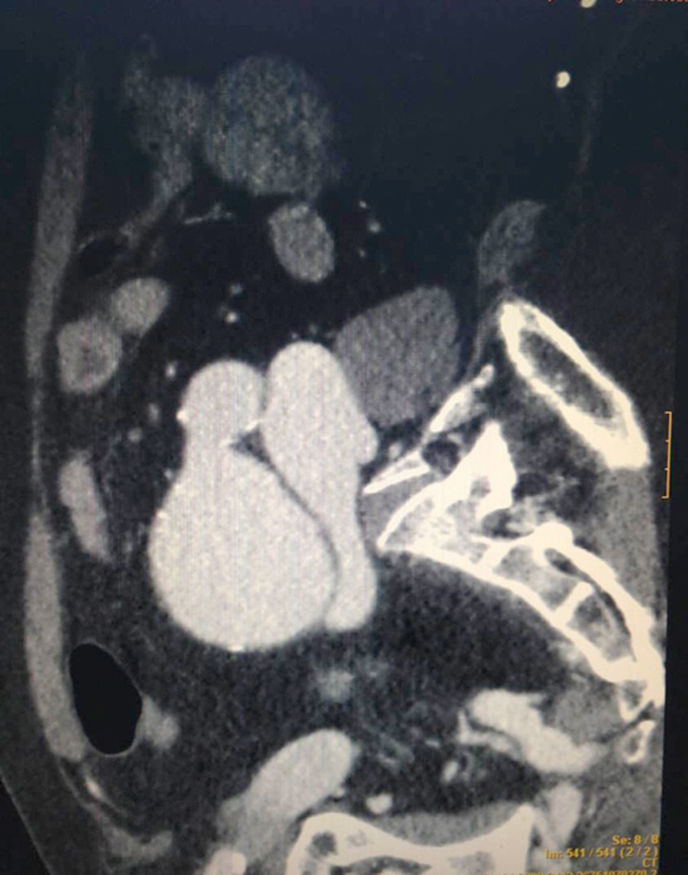
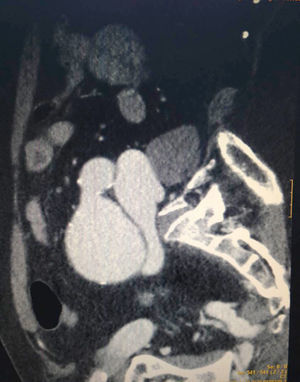
Seventy-five year-old-male with a history of hypertension and dyslipidemia. He presents to the ER with ischemic thoracic pain during the last forty-eight (48) hours. The ECG readings confirm a sinus rhythm of 110bpm, right bundle branch block, and ST-segment elevation in inferior leads; the blood tests show metabolic acidosis and slightly high troponin I levels (0.40ng/dl). The patient remains hypotensive and oligoanuric, with a correct oxygen-saturation. Physical examination: poor peripheral perfusion; tendency to tachypnea; poor pulse in the left groin area. On suspicion of acute coronary syndrome, an urgent coronary angiography procedure is conducted, but before that, one angio-CT scan (Fig. 1) is conducted to rule out aortic syndrome. There is presence of an iliac artery aneurysm on the left side, and an early inferior vena cava filling suggestive of possible arteriovenous communication due to complicated aneurysm. This led to canceling the coronary angiography procedure on suspicion of cardiogenic shock following right ventricular failure (RVF) due to sudden increase in the preload due to high-flow arteriovenous fistula. Here is what the echocardiography confirmed: RV dilation; severe tricuspid insufficiency; TAPSE <10mm; and preserved left ventricular function. After the urgent closure of the fistula, the vital signs, the ECG readings, and the echocardiography all came back to normal.
Please cite this article as: Ruiz de Gopegui Miguelena P, Zárate Chug P, Ruiz Frontera P. Inusual causa de shock cardiogénico. Med Intensiva. 2018;42:e3.