Primary: To evaluate the level of sedation, use, daily doses, and duration of analgosedative drugs in COVID-19 patients on mechanical ventilation (MV) using a standardized protocol, comparing survivors and non-survivors. Secondary: To identify independent predictors of hospital mortality.
DesignRetrospective cohort study.
SettingMedical-surgical ICU.
PatientsAdults with SARS-CoV-2 infection requiring invasive MV and continuous infusion of analgosedation and/or neuromuscular blocking agents (NMBAs) for at least 48 h.
InterventionsNone.
Main variables of interestLevel of sedation, use, daily doses, and duration of analgosedative drugs; hospital mortality and associated factors.
ResultsAmong 198 patients (nurse-to-patient ratio 1:2.4; 65% staff turnover), median global RASS was –4.5. Kaplan–Meier analysis showed lower survival with deeper sedation. Fentanyl (99%) and midazolam (97%) were the most used, followed by NMBAs (81%), propofol and dexmedetomidine (48%). Non-benzodiazepine sedatives were precribed more in survivors (88%) than non-survivors (53%) (p < 0.01). Survivors had more days of fentanyl, midazolam, and dexmedetomidine; no differences in NMBA use or drug doses were observed. Mortality was 63%. Independent predictors of mortality included APACHE II, SOFA24, Charlson score, median RASS, and non-benzodiazepine sedative use.
ConclusionsStandardized protocols emphasizing the ACD components of the ABCDEF bundle, along with appropriate use of analgosedation and NMBAs despite limited staffing, effectively supported the management of sedation without significant dose differences between survivors and non-survivors. Sedation level and the use of non-benzodiazepine sedatives were independently associated with better outcomes, highlighting the importance of the light sedation and the ABCDEF bundle.
Primario: Evaluar nivel de sedación, uso, dosis diarias y duración de fármacos analgosedantes en pacientes con COVID-19 en ventilación mecánica (VM) utilizando protocolos estandarizados, comparando sobrevivientes y no sobrevivientes. Secundario: Identificar predictores independientes de mortalidad hospitalaria.
DiseñoCohorte retrospectiva
ÁmbitoUCI médico-quirúrgica.
PacientesAdultos con SARS-CoV-2, VM invasiva e infusión continua de analgosedación y/o bloqueantes neuromusculares (BNMs) ≥48 horas.
IntervencionesNinguna.
Variables de interés principalesNivel de sedación, uso, dosis diarias y duración de analgosedantes; mortalidad hospitalaria y factores asociados.
ResultadosSe incluyeron 198 pacientes. Relación enfermero-paciente 1:2,4; recambio de enfermería 65%. El RASS global fue −4.5. La sedación profunda se asoció con menor supervivencia (Kaplan–Meier). Fentanilo (99%) y midazolam (97%) fueron los más utilizados; seguidos por BNMs (81%), propofol y dexmedetomidina (48%). Los sedantes no benzodiacepínicos se usaron en 88% de los sobrevivientes versus 53% de los no sobrevivientes (p < 0,01). Los sobrevivientes tuvieron significativamente más días con fentanilo, midazolam y dexmedetomidina, sin diferencias con BNMs ni en las dosis de todos los fármacos. Mortalidad 63%. Los predictores independientes de mortalidad incluyeron APACHE II, SOFA24, Charlson, RASS mediana y uso de sedantes no benzodiacepínicos.
ConclusionesProtocolos estandarizados que enfatizan los componentes ACD del paquete ABCDEF y el uso adecuado de la analgosedación y BNMs, incluso con personal limitado, permitieron una gestión efectiva de la sedación sin diferencias significativas en dosis entre sobrevivientes y no sobrevivientes. El nivel de sedación y los sedantes no benzodiacepínicos se asociaron independientemente con mejores resultados, destacando la importancia de sedación ligera paquetes ABCDEF.
ARDS is one of the most severe conditions in critical illness and was present in the most severe patients with COVID-19. The management of analgesia and sedation in this population was a unique challenge. Clinical practice guidelines for analgesia and sedation in the ICU have consistently focused on early rehabilitation and quick ventilator liberation.1,2 However, some ARDS patients require deep sedation or even neuromuscular blockade especially during the early phase of admission.3,4 Until the pandemic, patients with severe ARDS may not be represented in studies on analgesia and sedation that aimed mostly at evaluating a minimal sedation strategy and only a few studies on analgesia/ sedation have evaluated patients with need of deep sedation.5 Moreover, the pandemic may have significantly altered the administration of drugs for analgesia, sedation, and neuromuscular blockade, leading to a loss of control. Cohort studies and surveys reported increased use of high sedation rates with midazolam and propofol, leading to sustained deep sedation.6,7 This may have occurred not only due to the need to optimize AS for the situation, but also because of the inability to make dynamic adjustments at the bedside due to the risk of contagion. Other contributing factors could include medication shortages, the anticipated longer duration of mechanical ventilation (MV), and the involvement of non-ICU-trained staff in the treatment of COVID-19 patients during the pandemic.8,9
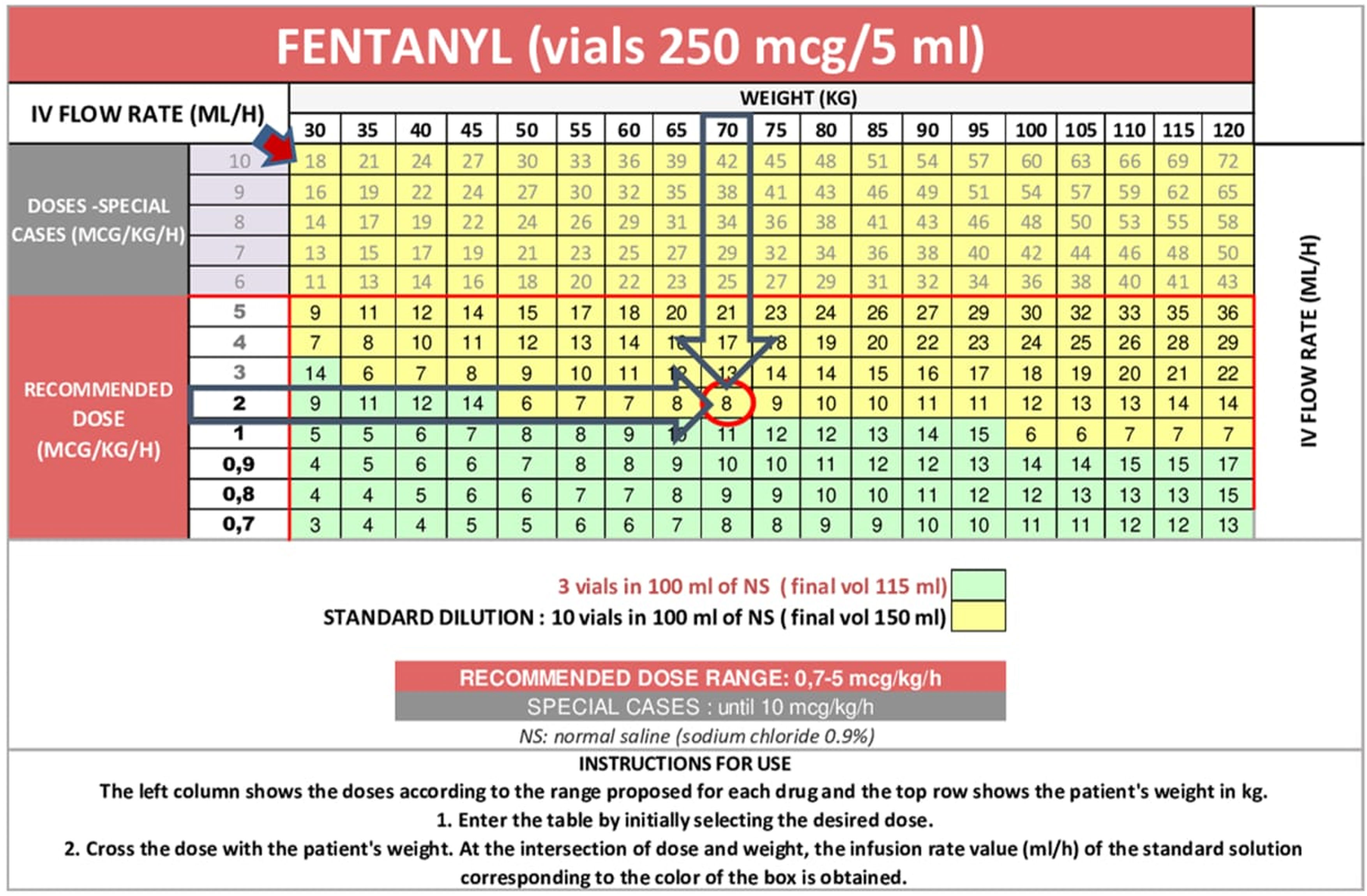
In our ICU, as part of a quality project aimed at standardizing prescriptions and reducing AS in accordance with established guidelines, we developed nomogram tools that have been in use since 2018.10,11 During the pandemic, their use was recommended by the Ministry of Health to guide and optimize AS practices in this context.
Our primary objective was to evaluate the level of sedation, as well as the use, duration, and daily doses of analgosedative drugs and neuromuscular blocking agents (NMBAs) in COVID-19 patients on mechanical ventilation, using a standardized protocol comparing survivors with non-survivors. A secondary objective was to identify independent predictors of hospital mortality.
MethodsThis retrospective, single-centre cohort study carried out in a 22-bed medical-surgical ICU, included patients aged 18 years and older with RT-PCR-confirmed SARS-CoV-2 infection who required invasive mechanical ventilation and received continuous infusion of analgosedation and/or NMBAs for at least 48 h. All patients had moderate to severe ARDS, as defined by the Berlin criteria, and were classified as having critical disease according to WHO guidelines.12,13 Patients were excluded from the analysis if SARS-CoV-2 infection was not confirmed, or if they required MV due to another cause. Patients were also excluded if no baseline data were recorded or if no details of sedation, analgesia or NMBAs use were available. Patients were followed until death in hospital or hospital discharge, whichever occurred first, allowing a complete case analysis. The local institutional review board approved the study and defined the requirement for informed consent was not necessary.
At ICU admission, we recorded patient demographics and characteristics, including date of admission, age, sex, body-mass index (BMI); comorbidities (hypertension, diabetes) and Charlson score; Acute Physiology and Chronic Health Evaluation II (APACHE II) and Sequential Organ Failure Assessment (SOFA) scores. We also registered use of prone positioning, including number of sessions, and requirement for renal replacement therapy (RRT). Duration of MV and length of ICU and hospital stay, in days, were also recorded.
Prescribed doses of continuous midazolam (MDZ), propofol (PROPO), dexmedetomidine (DEXME), fentanyl (FNT), remifentanil (R-FNT), and neuromuscular blocking agents (NMBAs) such as atracurium (ATRA), rocuronium (ROCU), and vecuronium (VECU), expressed in µg/kg/hour, mg/kg/hour or µg/kg/min, along with the duration of treatment for each drug, were collected daily for up to 28 days following ICU admission.
The Behavioral Pain Score (BPS)14 and the Richmond Agitation-Sedation Scale15 (RASS) were recorded daily as part of our local protocol for up to 28 days, with RASS values of –5 and –4 indicating deep sedation. Measurements taken while patients were under neuromuscular blocking agents (NMBAs) were not considered, as we did not have access to objective monitoring devices such as BIS (Bispectral Index), ANI (Analgesia Nociception Index), or NOL (Nociception Level Index).
Delirium was identified when the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU)16 was positive or when the patient required antipsychotics due to psychomotor agitation.
Since 2016, our unit has had a protocol for analgesia, sedation, and delirium, incorporating the latest evidence-based recommendations. Its goal is to administer the minimum necessary analgesia and sedation to keep patients comfortable, communicative, synchronized with mechanical ventilation and also to prevent post-ICU syndrome. The most important principles of our protocol are included in the supplementary material. This protocol ensures effective pain and sedation management, minimizes risks, optimizes patient outcomes, and enhances the standardization and safety of drug administration, especially in patients with organ dysfunction.
The primary outcome measures were level of sedation, use, daily doses and days of use of analgosedative drugs and NMBAs. All patients were followed until death or discharge, whichever occurred first. Secondary outcomes were hospital mortality, 28-day mortality and independent predictors of mortality.
Use of nomogram toolTo calculate the exact dose of each drug used for continuous AS, we utilized nomogram tools. These tools were developed in our ICU by clinical pharmacists as part of a quality project aimed at standardizing prescriptions and reducing AS in accordance with established guidelines. The nomograms provide information on drug dosing, dilutions, and acceptable ranges. For some drugs, there is an option to use them undiluted. The information is provided in dose/kg/hour to facilitate the precise calculation of the infusion rate for the infusion pump. Fig. 1 shows the nomogram template for fentanyl, with additional templates for all drugs available in Supplemental Fig. S1. The nomogram works as follows: the X-axis represents the drug dose, expressed in µg/kg/hour, µg/kg/min or mg/kg/hour depending on the drug, and the Y-axis represents the patient’s weight in kilograms. The intersection of these two values determines the infusion rate.
StatisticsVariables are reported as absolute numbers and percentages, or medians and interquartile range (IQRs). Differences between survivors and non-survivors in recorded variables were analysed with the χ² test or Fisher’s exact test, or the t test or Wilcoxon rank-sum test, as appropriate. All tests were two-sided, and a p value of <0·05 was considered to be statistically significant.
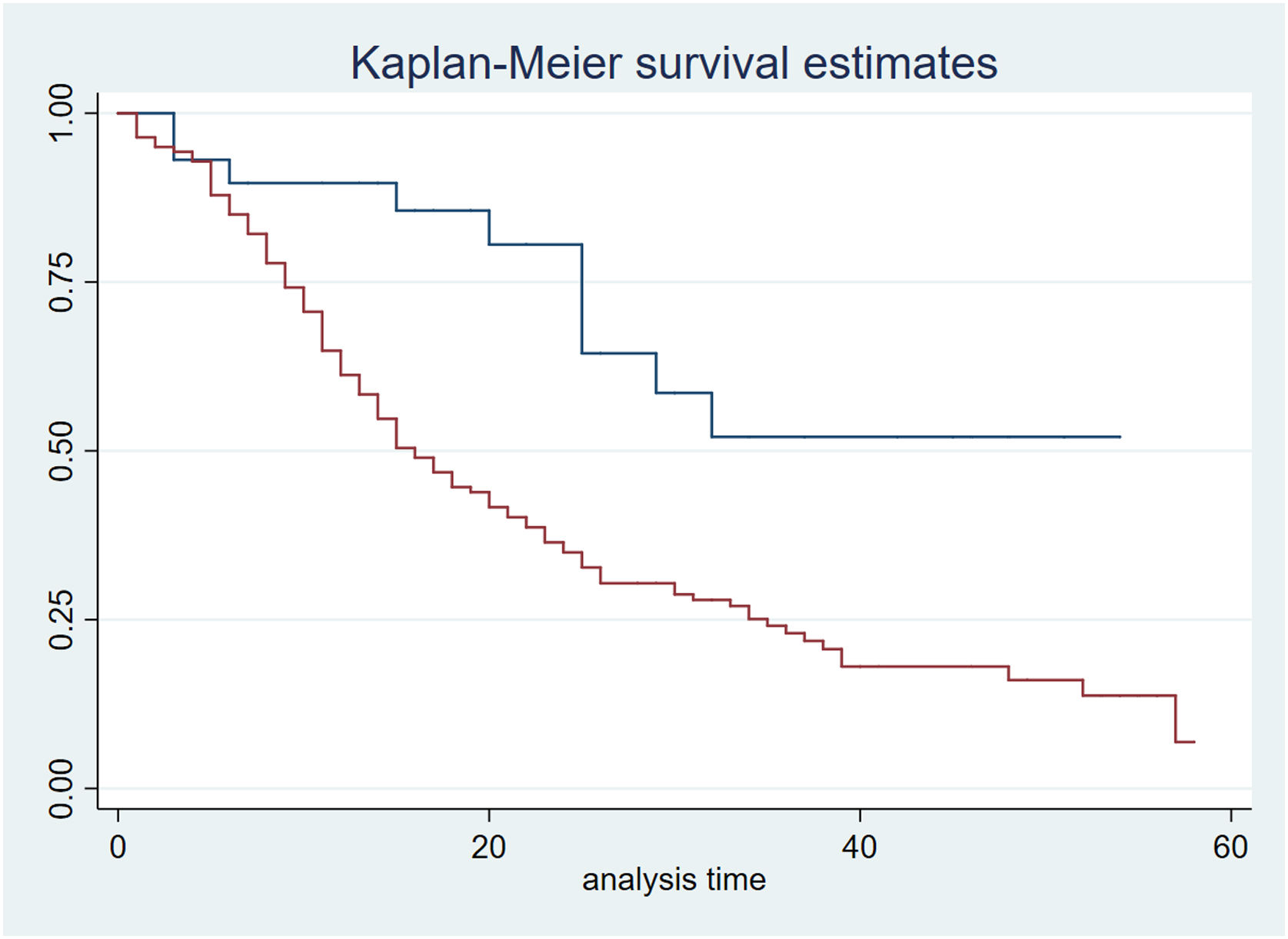
Hospital mortality was plotted as time-to-event curves. Kaplan–Meir survival function estimator method was constructed to compare time-to-event differences in patients according to level of sedation (deep sedation versus non-deep sedation). Differences in each case were analysed with the log-rank test.
Cox regression analysis was used to identify independent predictors of hospital mortality. Epidemiological and analgosedation variables that differed between survivors and non-survivors with a p-value < 0.20 were tested in the multivariable regression model. Variables with p < 0.05 were included as independent predictors of hospital mortality. Harrell’s C index was calculated to test the predictive capacity of the model. The proportional hazard assumption was tested by visual inspection of Schoenfeld residuals and by testing predicted versus observed values of model variables. Data were analysed with Stata 15.0 (Stata Corp LP, College Station, TX, USA).
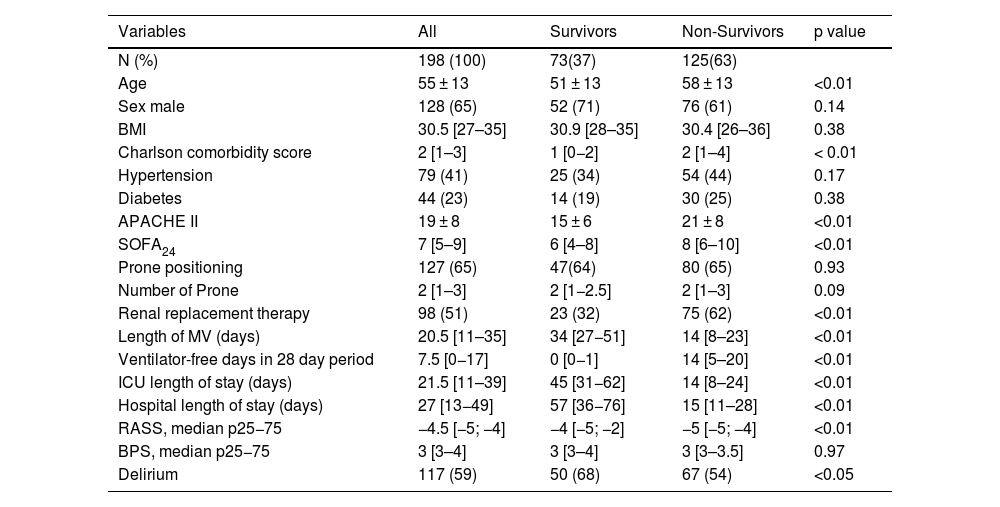
ResultsA total of 1,304 patients were admitted to our ICU from January 2020 to December 2022. Among these, 559 (43%) were diagnosed with COVID-19. Two hundred three required invasive mechanical ventilation and met ARDS criteria, and 198 were included for analysis. The flowchart illustrates an overview of patient selection (Suppl Fig. S2). Throughout the entire period, the nurse-to-patient ratio was 1:2.4, and the nurse staff turnover reached 65%. Baseline and evolving characteristics, along with median RASS, BPS scores, and delirium incidence for the total cohort, survivors, and non-survivors, are presented in Table 1. Briefly, the population was predominantly middle-aged and male, with comorbidities identified by the Charlson score, primarily hypertension and diabetes. Prone positioning was frequently utilized (64.8%) across the cohort, while the requirement for RRT was significantly higher among non-survivors. The study population experienced prolonged mechanical ventilation, extended ICU stay, and longer hospitalizations. Hospital mortality was 63% (125 patients), and 28-day mortality was 52.5%.
Epidemiological and outcome variables in invasively ventilated patients with COVID-19.
| Variables | All | Survivors | Non-Survivors | p value |
|---|---|---|---|---|
| N (%) | 198 (100) | 73(37) | 125(63) | |
| Age | 55 ± 13 | 51 ± 13 | 58 ± 13 | <0.01 |
| Sex male | 128 (65) | 52 (71) | 76 (61) | 0.14 |
| BMI | 30.5 [27–35] | 30.9 [28–35] | 30.4 [26–36] | 0.38 |
| Charlson comorbidity score | 2 [1–3] | 1 [0−2] | 2 [1–4] | < 0.01 |
| Hypertension | 79 (41) | 25 (34) | 54 (44) | 0.17 |
| Diabetes | 44 (23) | 14 (19) | 30 (25) | 0.38 |
| APACHE II | 19 ± 8 | 15 ± 6 | 21 ± 8 | <0.01 |
| SOFA24 | 7 [5–9] | 6 [4–8] | 8 [6–10] | <0.01 |
| Prone positioning | 127 (65) | 47(64) | 80 (65) | 0.93 |
| Number of Prone | 2 [1–3] | 2 [1−2.5] | 2 [1–3] | 0.09 |
| Renal replacement therapy | 98 (51) | 23 (32) | 75 (62) | <0.01 |
| Length of MV (days) | 20.5 [11–35] | 34 [27−51] | 14 [8–23] | <0.01 |
| Ventilator-free days in 28 day period | 7.5 [0−17] | 0 [0−1] | 14 [5–20] | <0.01 |
| ICU length of stay (days) | 21.5 [11–39] | 45 [31−62] | 14 [8–24] | <0.01 |
| Hospital length of stay (days) | 27 [13−49] | 57 [36−76] | 15 [11–28] | <0.01 |
| RASS, median p25−75 | −4.5 [−5; −4] | −4 [−5; −2] | −5 [−5; −4] | <0.01 |
| BPS, median p25−75 | 3 [3–4] | 3 [3–4] | 3 [3–3.5] | 0.97 |
| Delirium | 117 (59) | 50 (68) | 67 (54) | <0.05 |
Data are presented as n/N (%), median [IQR] or mean ± SD.
MV: mechanical ventilation; BMI: body mass index; APACHE II: Acute Physiology and Chronic Health Evaluation; SOFA: Sequential Organ Failure Assessment; RASS: Richmond agitation sedation scale; BPS: Behavioral pain scale.
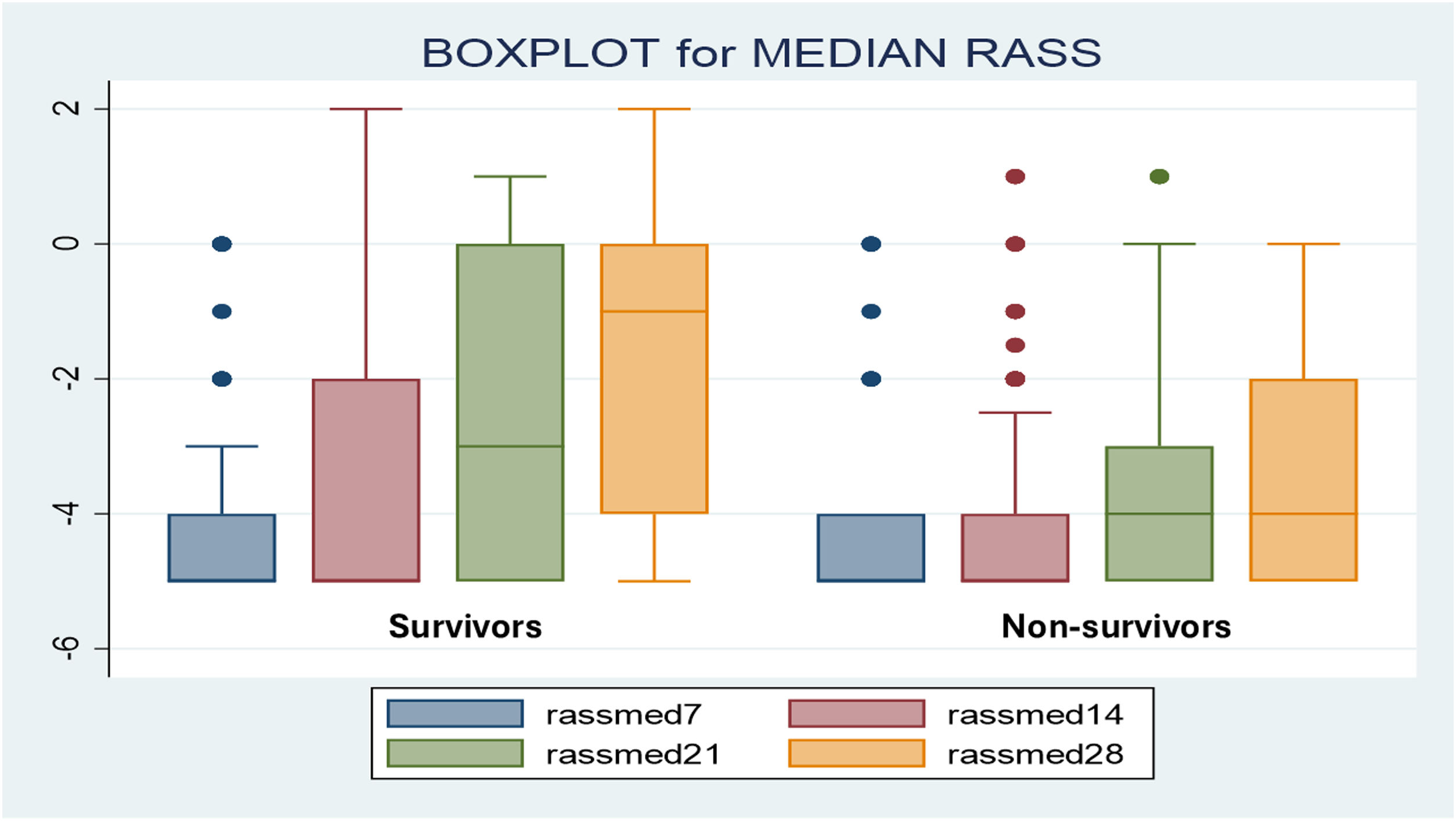
The global median RASS was −4.5, and the global median BPS was 3. The overall incidence of delirium was high (59%), with a higher incidence observed in survivors. Deep sedation was common across all patients; however, the median RASS was significantly more negative in non-survivors. Weekly analysis of the median RASS up to 28 days revealed significant differences at 21 and 28 days, with non-survivors consistently remaining in deep sedation (Fig. 2). The Kaplan–Meier curve indicated significantly lower survival in patients with deeper sedation (Fig. 3).
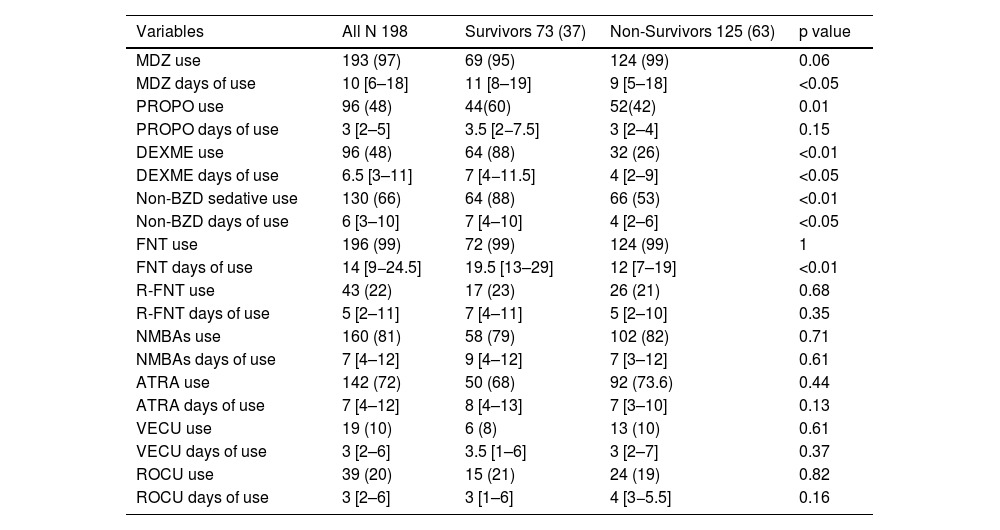
Regarding the use and duration of AS drugs, the use of midazolam (97%) and fentanyl (99%) was higher than other AS drugs and similar across both groups. Propofol and dexmedetomidine were used significantly more in survivors. When combined as nonbenzodiazepine sedatives, their use was observed in 88% of survivors compared to 53% of non-survivors (p < 0.01). Compared to non-survivors, survivors had a significantly higher median number of days with fentanyl (20 vs. 12 days), midazolam (11 vs. 9 days), and dexmedetomidine (7 vs. 4 days), likely reflecting their longer ICU length of stay and extended duration on MV. Neuromuscular blockade infusion was administered to 81% of patients for a median of 7 days, with atracurium being the most commonly used agent (72%), without differences between survivors and non-survivors. The details of usage and duration of all analgosedative drugs and NMBAs are presented in Table 2.
Sedative, analgesic and neuromuscular blocking agents, use and days of use.
| Variables | All N 198 | Survivors 73 (37) | Non-Survivors 125 (63) | p value |
|---|---|---|---|---|
| MDZ use | 193 (97) | 69 (95) | 124 (99) | 0.06 |
| MDZ days of use | 10 [6–18] | 11 [8–19] | 9 [5–18] | <0.05 |
| PROPO use | 96 (48) | 44(60) | 52(42) | 0.01 |
| PROPO days of use | 3 [2–5] | 3.5 [2−7.5] | 3 [2–4] | 0.15 |
| DEXME use | 96 (48) | 64 (88) | 32 (26) | <0.01 |
| DEXME days of use | 6.5 [3–11] | 7 [4−11.5] | 4 [2–9] | <0.05 |
| Non-BZD sedative use | 130 (66) | 64 (88) | 66 (53) | <0.01 |
| Non-BZD days of use | 6 [3–10] | 7 [4–10] | 4 [2–6] | <0.05 |
| FNT use | 196 (99) | 72 (99) | 124 (99) | 1 |
| FNT days of use | 14 [9−24.5] | 19.5 [13–29] | 12 [7–19] | <0.01 |
| R-FNT use | 43 (22) | 17 (23) | 26 (21) | 0.68 |
| R-FNT days of use | 5 [2–11] | 7 [4–11] | 5 [2–10] | 0.35 |
| NMBAs use | 160 (81) | 58 (79) | 102 (82) | 0.71 |
| NMBAs days of use | 7 [4–12] | 9 [4–12] | 7 [3–12] | 0.61 |
| ATRA use | 142 (72) | 50 (68) | 92 (73.6) | 0.44 |
| ATRA days of use | 7 [4–12] | 8 [4–13] | 7 [3–10] | 0.13 |
| VECU use | 19 (10) | 6 (8) | 13 (10) | 0.61 |
| VECU days of use | 3 [2–6] | 3.5 [1–6] | 3 [2–7] | 0.37 |
| ROCU use | 39 (20) | 15 (21) | 24 (19) | 0.82 |
| ROCU days of use | 3 [2–6] | 3 [1–6] | 4 [3−5.5] | 0.16 |
Data are presented as n/N (%) or median [IQR].
MDZ: midazolam; PROPO: propofol; DEX: dexmedetomidine; Non-BZD: nonbenzodiazepine; FNT: fentanyl; R-FNT: remifentanil; NMBAs: neuromuscular blocking agents; ATRA: atracurium; VECU: vecuronium; ROCU: rocuronium.
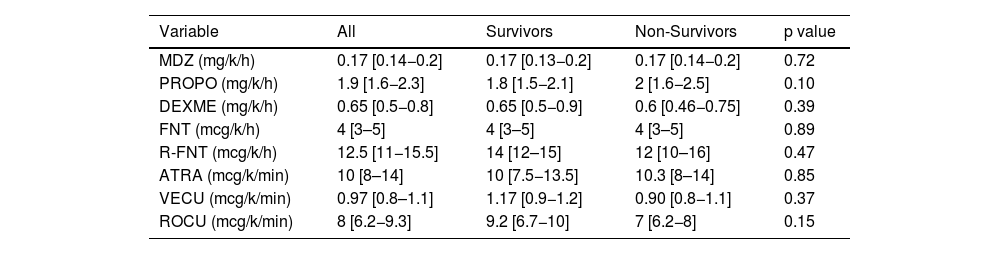
Regarding the doses of AS drugs, the median doses of sedatives, analgesics, and NMBAs remained within the range established by our ICU protocol, guided by clinical pharmacists. However, opioids were administered at high doses. Notably, no differences in doses of any drug were observed between survivors and non-survivors (Table 3).
Doses of sedative, analgesic and neuromuscular blocking agents in invasively ventilated patients with COVID-19.
| Variable | All | Survivors | Non-Survivors | p value |
|---|---|---|---|---|
| MDZ (mg/k/h) | 0.17 [0.14−0.2] | 0.17 [0.13−0.2] | 0.17 [0.14−0.2] | 0.72 |
| PROPO (mg/k/h) | 1.9 [1.6−2.3] | 1.8 [1.5−2.1] | 2 [1.6−2.5] | 0.10 |
| DEXME (mg/k/h) | 0.65 [0.5−0.8] | 0.65 [0.5−0.9] | 0.6 [0.46−0.75] | 0.39 |
| FNT (mcg/k/h) | 4 [3–5] | 4 [3–5] | 4 [3–5] | 0.89 |
| R-FNT (mcg/k/h) | 12.5 [11−15.5] | 14 [12–15] | 12 [10–16] | 0.47 |
| ATRA (mcg/k/min) | 10 [8–14] | 10 [7.5−13.5] | 10.3 [8–14] | 0.85 |
| VECU (mcg/k/min) | 0.97 [0.8–1.1] | 1.17 [0.9−1.2] | 0.90 [0.8−1.1] | 0.37 |
| ROCU (mcg/k/min) | 8 [6.2−9.3] | 9.2 [6.7−10] | 7 [6.2−8] | 0.15 |
Data are presented as median [IQR].
MDZ: midazolam; PROPO: propofol; DEX: dexmedetomidine; FNT: fentanyl; R-FNT: remifentanil; ATRA: atracurium; VECU: vecuronium; ROCU: rocuronium.
We first performed a bivariate analysis of each epidemiological or severity variable at admission, as well as analgosedation variables and drug usage. Variables with a p-value < 0.2 from Tables 1 and 2 were then entered into the multivariate model. The multivariate Cox regression model identified the following as independent predictors of mortality: APACHE II (HR 1.05, 95% CI 1.01–1.09), SOFA score (HR 1.09, 95% CI 1.01–1.18), Charlson score (HR 1.13, 95% CI 1.01–1.27), median RASS (HR 0.82, 95% CI 0.69–0.97), and nonbenzodiazepine sedative use (HR 0.24, 95% CI 0.15–0.38).
DiscussionThis is the first study to link the level of sedation and the analgosedative and NMBAs use with hospital mortality in COVID-19 patients on MV with moderate or severe ARDS. Hospital mortality was 63%, which was 10 percentage points higher than the 28-day mortality rate, highlighting the prolonged length of stay and the occurrence of mortality events several days later of ICU admission.
In the main cohort study of COVID-19 patients on MV conducted in Argentina during the first wave of the pandemic, 68% were men, with hypertension and obesity as the main comorbidities. Additionally, 88% developed ARDS, and 62% required prone positioning—findings similar to ours. Hospital mortality was 58%, slightly lower than the mortality rate observed in our study.17 Unlike this study, our research encompassed both pandemic waves and focused exclusively on patients with moderate or severe ARDS, representing the sickest patients. Although our mortality rate closely aligns with those reported in New York City (60%), Spain (59%), and Israel (56%),18–20 it was higher in similar cohorts of patients on MV in the region, such as in Mexico and Brazil (74% and 80%, respectively).21,22
By the other hand in our cohort, the level of sedation by each point of RASS augmentation, and the use of nonbenzodiazepine sedatives, lower mortality-, along with APACHE II, SOFA24 and Charlson scores, were independent predictors of mortality—the latter three being variables commonly reported in other cohorts, but the two first not assessed in others. It is important to highlight that, although midazolam was the most frequently used sedative, the use of nonbenzodiazepine sedatives was associated with lower mortality. Furthermore, in our study, three components of the ABCDEF bundle were addressed: “A” (Assessment, Prevention, and Management of Pain); “C” (Choice of Analgesia and Sedation); and “D” (Delirium Assessment, Prevention, and Management).8 There were no differences in pain assessment scores between survivors and non-survivors; however, the doses and duration of opioid use were high, likely due to the high prevalence of deep sedation and extended MV. Notably, the doses of all analgosedative drugs were similar between survivors and non-survivors (Table 3). In the largest multicenter cohort study carried out during the pandemic evaluating the implementation of the ABCDEF bundle, which included 69 adult ICUs across 14 countries, the epidemiology of coma and delirium in critically ill patients with COVID-19 was assessed. The study reported lower use and shorter duration of continuous benzodiazepine and opioid infusions compared to our findings. However, propofol use and duration were higher, and the use of dexmedetomidine was similar, although we administered it for more days. Delirium incidence and ventilator-free days were comparable, but 28-day mortality was lower.23
In another point prevalence study, the implementation rates of the ABCDEF bundle—both for each individual element and for an ICU diary—were found to be extremely low for patients with and without COVID-19 infections during the pandemic.24
A survey on practices conducted before and during the pandemic outlined the use of analgosedative drugs, but not the specific details regarding its usage. In this survey, which had significant representation from South America and Europe, it was reported that prior to the pandemic, the drugs used for patients with ARDS were midazolam, propofol, and fentanyl. Only 26% of respondents from South America and 12% from Europe reported using dexmedetomidine. During the pandemic, the main use was for midazolam (76%) and propofol (74%) for sedation, and fentanyl and morphine for analgesia.7 In another survey conducted by FEPIMCTI in the Pan-American and Iberian settings, which evaluated analgosedation and delirium practices as well as factors associated with oversedation after the COVID-19 pandemic, respondents from South America were the most likely to recognize oversedation, and habit acquired during the pandemic was identified as the main factor contributing to oversedation.25
Moreover, the continuous infusion of benzodiazepines is still widely used despite the associated complications, such as delayed awakening and extubation, prolonged ICU and hospital stay, increased delirium, cognitive impairment, and post-ICU syndrome.26 However, midazolam remains a valuable option in deep sedation strategies as long as the maximum recommended doses are not exceeded, particularly when periods of neuromuscular blockade are required or when the patient's clinical condition—such as shock, hemodynamic instability, or lactic acidosis—makes the use of propofol or volatile anaesthetics inadvisable.27
In our study we evaluated the daily doses of each analgosedation drug, and in accordance with current guidelines, the maximum dose of any drug was never exceeded, even when deep sedation was required for patients with ARDS in the prone position. Additionally, the use, duration, and doses of NMBAs were consistent between survivors and non-survivors, reflecting the high percentage of patients requiring these agents for early severe ARDS, as recommended by the guidelines.28–30
Delirium was screened in patients with a RASS > −2 and was assumed in those requiring antipsychotics. Although we observed a higher incidence of delirium among survivors, the prevalence in non-survivors—considering the high proportion of patients managed at very deep levels of sedation—can be assumed to be nearly 100% in absence of assessment results, as noted by Devlin et al.8,31
Although recommendations for analgesia-sedation strategies in COVID-19 patients existed, there was limited literature providing detailed information on measured doses and duration.7–9,32 Our study demonstrates that the use of established protocols, including nomograms with fixed dilutions, pure dose options, and maximum dose ranges, ensured uniform optimization for this patient group, despite the overuse of benzodiazepine and opioid infusions. Originally designed to prioritize an analgesia-before-sedation approach and promote light sedation with non-benzodiazepine sedatives like propofol or dexmedetomidine, these nomograms were adapted during the pandemic to streamline and limit dosing prescriptions, even for deep sedation cases. They also facilitated accurate analgosedation administration during personnel shortages and enabled seamless transitions to alternative NMBAs during stock outages, such as with atracurium.
Maintaining critically ill patients under light or no sedation has a greater impact on patient-centered outcomes than the specific drug choice. However, achieving light sedation in real-world settings remains challenging, especially in low- and middle-income countries. During the pandemic, this goal was further complicated by factors such as high staff turnover and inadequate nurse-to-patient ratios.32,33 A 3:1 nurse-to-patient ratio was significantly associated with the non-implementation of elements A and C of the ABCDEF bundle.24 In Argentina, a large quasi-experimental study evaluating a multifaceted approach to improve care delivery during the pandemic reported a staff turnover rate of 35%.34
In our ICU, nurse staff turnover exceeded 60%, aligning with rates reported in Argentine ICUs during the pandemic.35 These issues, including inadequate nurse-to-patient ratios, were longstanding challenges in Latin American ICUs even before the pandemic.36
Anecdotal evidence and expert opinions do have their place during difficult times, and the COVID-19 pandemic has undoubtedly created desperation in certain hospitals and scenarios.37 In response, strategies such as the "Oversedation Zero" tool—which promotes clear goal setting, protocol implementation, clinical pharmacy support, pain and sedation monitoring, dynamic titration, and avoidance of unnecessary deep sedation—may prove highly effective.38 Other guidelines support these principles, emphasizing multimodal pain management, minimizing sedation levels, and reserving deep sedation for selected cases, with growing evidence favoring agents such as dexmedetomidine, remifentanil, and ketamine.39
LimitationsThe retrospective study design relied on clinical records, which may be less sensitive than prospective research assessments for evaluating sedation levels and detecting delirium. Moreover, the lack of objective devices for measuring pain and sedation levels while patients were under NMBAs was also a limitation. However, the use, duration, and doses of AS drugs and NMBAs were prospectively recorded in an automatic dispensing system, ensuring the validity of prescriptions.
We did not collect data on the rationale behind sedation choices; however, based on reports, we can speculate that the use of deep sedation and neuromuscular blockade, in the context of moderate-to-severe ARDS and a previously adopted protocol, coupled with resource constraints, influenced some of these decisions. Additionally, we did not evaluate all the components of the ABCDEF bundle.
Another limitation is the single-center study, which could limit the generalizability of the findings. As with any observational study, we cannot establish causality when examining factors associated with mortality, sedation levels, or sedation choices in patients with COVID-19. However, using an adjustment model, we were able to identify independent associations, although we could not determine whether the observed benefits of sedation level on mortality were related to light sedation or to less profound deep sedation, as the variable was introduced as a continuous one. Additionally, we did not record whether coma was intentionally drug-induced or a result of the patient’s disease process. However, our findings align with numerous previous studies on delirium and coma in acute respiratory patients without COVID-19. These results are essential for healthcare teams to make informed quality improvement decisions for COVID-19 care, drawing on evidence from before the pandemic to identify potential modifiable risk factors.
ConclusionsThe use of standardized protocols prioritizing the evaluation of the ACD components of the ABCDEF bundle may have contributed to the appropriate use of analgosedation and NMBAs, even with limited healthcare personnel. This approach was effective even when deep sedation was necessary, with no significant differences observed in doses of analgosedative drugs and NMBAs between survivors and non-survivors, aiding in the management of patients in middle-income countries and beyond. The level of sedation and the use of nonbenzodiazepine sedatives were independently associated with better outcomes, emphasizing the importance of implementing and prioritizing light sedation whenever possible, along with the other components of the ABCDEF bundle.
CRediT authorship contribution statementConception and design of the study: Cecilia Inés Loudet, Marisol García Sarubbio, María Julia Meschini and Rosa Reina.
Acquisition of data: Jacqueline Vilca Becerra, María Agustina Mazzoleni, Vanesa Aramendi, Agustina Barbieri, Carolina Colavita, Gustavo Cerri and Sofía Pacho
Analysis and interpretation of data: Cecilia Inés Loudet, Marisol García Sarubbio, María Julia Meschini, Rosa Reina and Eliseo Ferrari
Drafting the article: Cecilia Inés Loudet, Marisol García Sarubbio and María Julia Meschini Revising the article critically for important intellectual content: Rosa Reina and Eliseo Ferrari
Final approval of the version to be submitted: All authors
Declaration of Generative AI and AI-assisted technologies in the writing processDuring the preparation of this work the authors used ChatGPT 4.0 in order to improve grammar. After using this tool, the authors reviewed and edited the content as needed and takes full responsibility for the content of the publication.
FundingThis research study was not financed
The authors do not have any conflict of interest to declare
Pharmacy Service: Viviana Pazos and Claudia Edith Páez.
ICU: Maria Cecilia Marchena and Maria Gabriela Sáenz.