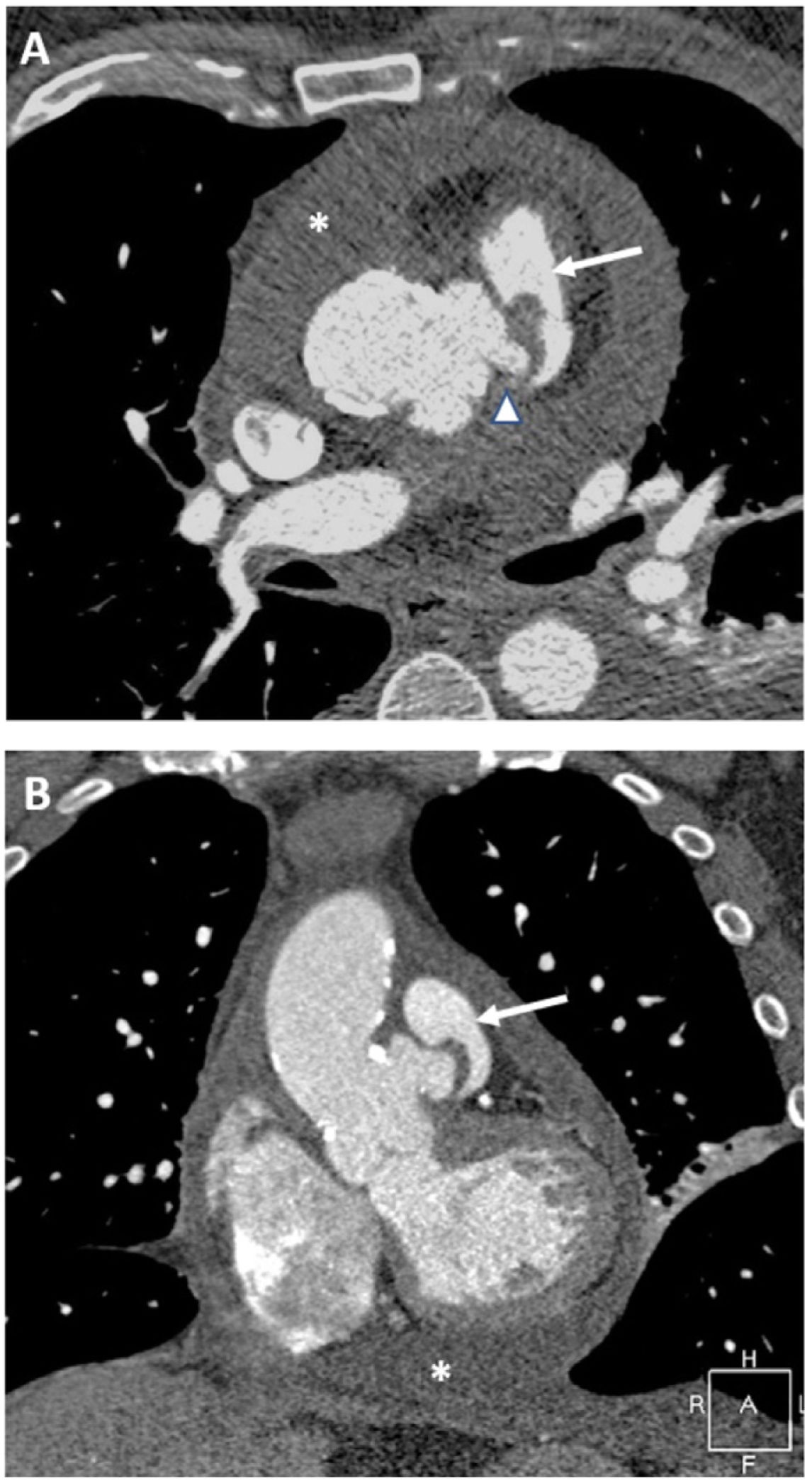
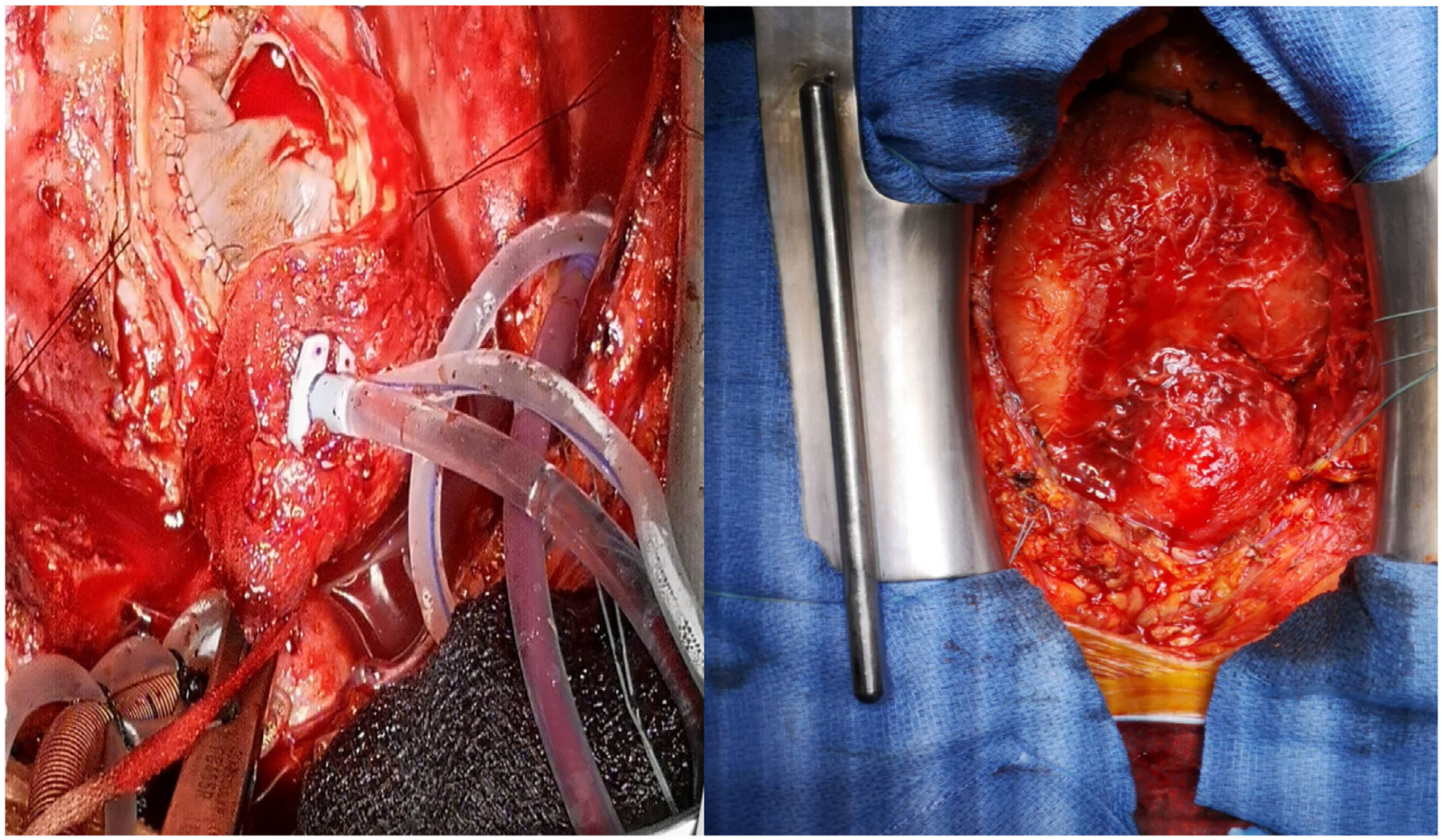
This is the case of a 62-year-old man with lower back pain, bacteremia, and isolation of Streptococcus agalactiae in hemocultures (group B). Nuclear magnetic resonance imaging is performed and a diagnosis of osteomyelitis at L5 level is achieved. The transthoracic echocardiography performed confirms the presence of severe pericardial effusion without clinical signs of tamponade or signs suggestive of infectious endocarditis. The coronary computed tomography angiography (CCTA) performed reveals the presence of an image of irregular morphology around the sinotubular junction suggestive of pseudoaneurysm (Fig. 1, axial view [A], and coronal view [B]) (Fig. 2 3D reconstruction) damaging almost its entire circumference, a 12mm×5mm aortopulmonary fistulous trajectory (arrow) including, in its inner portion, the left coronary ostium (arrowhead) with high-density pericardial effusion (asterisk) suggestive of infectious nature. Suspected infectious etiology due to microorganism isolated from the aortic pseudoaneurysm abscess being the fistula due to the latter. Emergency surgery for partial pseudoaneurysm repair is attempted (Fig. 3, direct surgical view) with heterologous pericardial patch, closure due to direct suture of the fistula, and bilateral ante-phrenic pericardiectomy (seropurulent exudate with a great amount of fibrin and epicardial adherences without microbiological isolates). The control CCTA confirms the closure of the pseudoaneurysm and the lack of interatrial shunt with practical resolution of pericardial effusion. The patient’s disease progression is favorable.
FundingNone whatsoever.
Conflicts of interestNone reported.