To compare the complications and the difficulty of orotracheal intubation procedures performed in the Intensive Care Unit during the off-hours period and the on-hours period.
DesignA prospective, observational and non-interventional cohort study covering a period of 27 months was carried out. Working days between 8:00 a.m. and 7:59 p.m. were considered “on-hours”, while the remaining shifts were regarded as “off-hours”.
ScopeAn 18-bed surgical in a Intensive Care Unit of a third-level hospital.
PatientsAll orotracheal intubation patients admitted to the ICU from January 2015 to March 2017 were included. Patients were stratified into 2 groups according to whether intubation was performed on-hours or off-hours.
InterventionsNon-interventional study.
Variables of interestThe reason for intubation, time and day on which intubation was performed, degree of intubation difficulty (number of attempts, Cormack–Lehane laryngoscopic vision, need for accessory material) and complications during intubation.
ResultsA total of 252 patients were intubated; of these, 132 were included in the on-hours group and 120 patients in the off-hours group. In the off-hours group we observed a greater percentage of urgent and emergent intubations compared to the on-hours group. However, no differences were found between the 2 groups in relation to the other variables studied.
ConclusionsDuring the off-hours period, orotracheal intubation was not associated to a greater number of complications or to greater difficulty of the technique in our Unit.
Comparar las complicaciones y el grado de dificultad de la intubación orotraqueal realizada en una Unidad de Cuidados Críticos, durante el periodo off-hours (turno de noche y fines de semana) y el periodo on-hours (turno de día).
DiseñoEstudio de cohortes, prospectivo, observacional y no intervencionista, durante un periodo de 27 meses. Se consideró on-hours el periodo de entre las 8:00 a.m. y las 7:59 p.m. de los días laborales, y off-hours el resto de los turnos.
ÁmbitoUna Unidad de Cuidados Críticos de 18 camas de un hospital clínico universitario de tercer nivel.
PacientesSe incluyó a todos los pacientes con intubación orotraqueal en la unidad desde enero de 2015 hasta marzo de 2017. Los pacientes se estratificaron en 2 grupos en función de si la intubación se realizaba en periodo on-hours u off-hours.
IntervencionesEstudio no intervencionista.
Variables de interésMotivo de intubación, hora y día en el que se realiza la intubación, grado de dificultad de intubación (número de intentos, visión laringoscópica Cormack-Lehane, necesidad de material complementario) y complicaciones durante la intubación.
ResultadosSe intubó a 252 pacientes, de los que 132 fueron incluidos en el grupo on-hours y 120 en el grupo off-hours. En el grupo off-hours observamos un mayor porcentaje de intubaciones urgentes o emergentes en comparación con el grupo on-hours. No encontramos diferencias entre los 2 grupos en el resto de las variables estudiadas.
ConclusionesLa intubación que se realiza en nuestra unidad durante el periodo off-hours no se ha podido asociar a un mayor número de complicaciones ni a una mayor dificultad de la técnica.
Several studies have associated a greater number of complications and higher mortality rates in patients hospitalized in Intensive Care Units (ICU) during the night or during weekends compared to patients hospitalized during the day.1–5 This period of time that includes the night and the weekend is known as off-hours schedule.
Endotracheal intubation is one procedure that is usually conducted both in the operating room (OR) and in the ICU. This procedure is associated with a higher incidence rate of complications in the ICU compared to the OR, both because the technique is difficult and because of the poor hemodynamic or respiratory situation of the patient admitted to the ICU.6 Around 30–40% of serious complications during intubation have been reported in patients admitted to the ICU.6,7 A recent study conducted in Japan by Ono et al.8 confirmed more complications in patients intubated at night or during the weekend than in patients intubated during the day. They associated those results with fewer personnel during that time and with unexperienced personnel managing this difficult airway.
The goal of our study was to compare the complications and difficulty of the intubation procedures conducted at night or during the weekend with those conducted during the day at the Critical Care Unit (CCU) from the Hospital Clínico Universitario of Santiago de Compostela, Spain.
MethodsObservational prospective cohort study conducted for 27 months (from January 2015 through March 2017) at the CCU from the Hospital Clínico Universitario of Santiago de Compostela, Spain. Our CCU has 18 beds for patients that are managed by physicians, and surgeons. On business days and during day time there are 5–6 assistant physicians available, and 1–3 resident physicians; the rest of the time, including nights and weekends, there are 2 assistant physicians available and 1 resident physician. The number of nurses available is always the same in every shift: there is always one nurse for every 2 patients. All physicians, assistant or resident, are experienced managing this difficult airway and at least 2 assistant physicians are on call 24 hours a day in the unit.
The study included all those patients above 18, admitted to the CCU for whatever reason who required intubation for whatever reason. Patients intubated outside the CCU were not included in the study. The study was approved by the Galicia Ethics Committee with registry code #2015/012. Given the special characteristics of the study, informed written consent was not required.
All intubations were conducted by medical personnel at the Unit of Anesthesiology and Resuscitation from the Hospital Clínico Universitario of Santiago de Compostela, Spain (assistant physician with over 4 year-experience conducting intubation, or resident physicians tutored by one assistant physician). After the intubation whoever it is that conducted the procedure had to fill out a form including: demographic data of patients, reason for admission at the CCU, reason why the patient was intubated, use of non-invasive mechanical ventilation prior to intubation, hour and time when the intubation was conducted, degree of urgency in the intubation procedure (scheduled, semi-scheduled [>30min], urgent [<30min], emergent) and prior physiological variables during intubation and 15min after intubation (arterial blood pressure, heart rate, oxygen saturation). The following data were collected regarding the intubation procedure: number of laryngoscopy procedures attempted, laryngoscopic view according to the modified Cormack–Lehane scale, degree of difficulty in the intubation procedure observed by the anesthesiologist (no difficulty, some, moderate, or serious difficulty), need for additional material for the intubation (Frova intubating introducer, glidescope, fiberscope, other), and complications during intubation or 15min after intubation (hypotension, hypoxia, esophageal intubation, bronchoaspiration, other).
The main goal of the study was to compare the incidence rate of complications when the intubations were conducted off-hours (night shift and weekends) and on-hours (day shift). During the off-hours schedule the patients included were those intubated between 8:00 p.m. and 7:59 a.m. and during weekends between Friday 8:00 p.m. and Monday 7:59 a.m. During the on-hours schedule the patients included were those intubated from Monday through Friday between 8:00 a.m. and 7:59 p.m. Each and every one of the complications was assessed separately. These were the complications included: hypotension (lower systolic blood pressure<80mmHg), severe hypotension (systolic blood pressure<65mmHg), hypoxia (arterial saturation of oxygen<90%), severe hypoxia (arterial saturation of oxygen<80%), esophageal intubation and bronchoaspiration.
The secondary goal of the study was to compare the difficulty of the intubation procedure between the two groups of patients measured by the number of laryngoscopy procedures conducted (1, 2, 3, >3), the best laryngoscopic view according to the modified Cormack–Lehane scale (grade I,IIa,IIb,III,IV), the need for additional material for the intubation procedure, or how difficult the intubation was according to the anesthesiologist.
Statistical analysisThe analyses were conducted using R v.3 (R Project for Statistical computing, Vienna, Austria). The qualitative variables were expressed as frequencies and percentages; the numerical variables were expressed as mean and interquartile range. After the distribution analysis of numerical variables was conducted, none of them met the conditions of normality (Kolmogorov–Smirnov test) and homoscedasticity (Levene test) which is why non-parametric tests for hypothesis testing were used.
Univariate analyses were conducted using the chi-square test (Pearson and Fisher, according to the condition of data) and Wilcoxon test.
Similarly, multivariate analyses with logistic regression were conducted being the most significant variables of all: the difficulty, or not, of intubation, and the presence, or not, of complications during the intubation procedure. The risk of associated independent factors was expressed using the odds ratio. Choosing the final model was based on the minimum Akaike information criterion (AIC) value. Finally, the predictive capability of the final model was assessed using the area under the ROC curve (AUC-ROC).
Multiple comparisons were penalized through the Benjamini–Hochberg correction method.
Estimating the sample sizeDifferent studies have confirmed that the percentage of complications after intubation procedures in Intensive Care Units is somehow around 40%.8 Assuming 20% more complications after intubation procedures during the off-hours schedule as clinically significant, we estimated that it would take 98 patients per group to detect that difference in a Chi-square test of independence with an α error of 0.05 and a power of 80%. When it comes to the sample size for logistic regressions the Peduzzi et al. method was used (https://www.ncbi.nlm.nih.gov/pubmed/8970487): approximately 10 patients were needed per adjusted covariable.
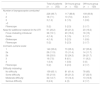
ResultsIn the study period, 252 patients were intubated at the CCU, out of which 132 were intubated in the on-hours schedule, and 120 in the off-hours schedule. No significant differences were found in the demographic characteristics of the patients in the 2 schedules (Table 1).
The reason for admission at the CCU and the reason for intubation are described in Table 2. In the off-hours schedule we observed a higher percentage of urgent intubations compared to the on-hours schedule. However, we found a higher percentage of urgent intubations compared to the on-hours schedule. However, we found more semi-scheduled intubations in the on-hours schedule. These differences were not statistically significant though.
Characteristics of intubation procedures on the 2 groups of patients.
| Total of patients (n=252) | On-hours group (n=132) | Off-hours group (n=120) | |
|---|---|---|---|
| Reason for CCU admission | |||
| Postoperative surgery | 117 (46.4) | 64 (48.5) | 53 (44.2) |
| Respiratory failure | 82 (32.5) | 39 (29.5) | 43 (35.8) |
| Hemodynamic abnormality | 32 (12.7) | 20 (15.2) | 12 (10) |
| Neurological abnormality | 34 (13.5) | 15 (11.4) | 19 (15.8) |
| Polytrauma | 2 (0.7) | 2 (1.5) | 0 (0) |
| Other | 2 (0.7) | 1 (0.7) | 1 (0.8) |
| Indication of intubation | |||
| Respiratory failure | 195 (77.4) | 97 (73.5) | 98 (81.7) |
| Hemodynamic abnormality | 33 (13.1) | 16 (12.1) | 17 (14.1) |
| Neurological abnormality | 54 (21.4) | 24 (18.2) | 30 (25) |
| Self-extubation | 10 (4) | 7 (5.3) | 3 (2.5) |
| Failure of extubation | 18 (7.1) | 9 (6.8) | 9 (7.5) |
| Scheduled | 13 (5.2) | 11 (8.2) | 2 (1.7) |
| Use of NIMV prior to intubation | 152 (60.3%) | 73 (55.3) | 79 (65.8) |
| Type of intubation | |||
| Scheduled | 13 (5.2) | 11 (8.3) | 2 (1.7) |
| Semi-scheduled | 84 (33.3) | 51 (38.6) | 33 (27.5) |
| Urgent | 141 (56) | 63 (47.7) | 78 (65.5) |
| Emergent | 14 (5.6) | 7 (5.3) | 7 (5.8) |
Data expressed as numbers and percentages (%). There are no significant differences between the two groups of patients.
CCU: Critical Care Unit; NIMV: non-invasive mechanical ventilation.
Table 3 shows the difficulty while intubating during the 2 schedules, assessed by the number of laryngoscopies, the modified Cormack–Lehane scale, the need for additional material for the intubation, and the difficulty of intubation assessed by the physician conducting the intubation. We found no differences in any of the variables associated with difficulty while conducting the intubation in the two groups of patients.
Difficulty during the intubation procedure in the 2 groups of patients.
| Total of patients (n=252) | On-hours group (n=132) | Off-hours group (n=120) | |
|---|---|---|---|
| Number of laryngoscopies conducted | |||
| 1 | 226 (89.7) | 117 (88.6) | 109 (90.8) |
| 2 | 18 (7.1) | 10 (7.6) | 8 (6.7) |
| 3 | 3 (1.2) | 2 (1.5) | 1 (0.8) |
| >3 | |||
| Fiberscope | 5 (2) | 3 (2.3) | 2 (1.7) |
| Need for additional material for the OTI | 51 (20.2) | 28 (21.2) | 23 (19.2) |
| Frova intubating introducer | 38 (15.1) | 20 (15.2) | 18 (15) |
| Guide | 4 (1.6) | 2 (1.5) | 2 (1.7) |
| Glidescope | 4 (1.6) | 3 (2.3) | 1 (0.8) |
| Fiberscope | 5 (2) | 3 (2.3) | 2 (1.7) |
| Cormack–Lehane scale | |||
| 1 | 140 (55.6) | 73 (55.3) | 67 (55.8) |
| 2a | 29 (11.5) | 15 (11.4) | 14 (11.7) |
| 2b | 58 (23.0) | 32 (24.2) | 26 (21.7) |
| 3 | 19 (7.5) | 8 (6.1) | 11 (9.2) |
| 4 | 1 (0.4) | 1 (0.8) | 0 (0) |
| Fiberscope | 5 (2) | 3 (2.3) | 2 (1.7) |
| Difficulty intubating | |||
| No difficulty | 159 (63.1) | 81 (61.4) | 78 (65) |
| Some difficulty | 55 (21.8) | 28 (21.2) | 27 (22.5) |
| Moderate difficulty | 32 (12.7) | 19 (14.4) | 13 (10.8) |
| Serious difficulty | 6 (2.4) | 4 (3) | 2 (1.7) |
Data expressed as numbers and percentages (%). There are no significant differences between the two groups of patients.
OTI: orotracheal intubation.
The most common complications of the patients intubated in our CCU was hypotension (27.8%), followed by hypoxia (19.8%). We found no differences between the two groups when it comes to complications associated with intubation (Table 4).
Frequency of complications during the intubation procedure in the two groups of patients.
| Total number of patients (n=252) | On-hours group (n=132) | Off-hours group (n=120) | |
|---|---|---|---|
| Complications during intubation | 105 (41.7) | 50 (37.9) | 55 (45.8) |
| Hypotension <80mmHg | 70 (27.8) | 37 (28) | 33 (27.5) |
| Hypotension <65mmHg | 40 (15.9) | 23 (17.4) | 17 (14.2) |
| Hypoxia <90% | 50 (19.8) | 23 (17.4) | 27 (22.5) |
| Hypoxia <80% | 29 (11.5) | 15 (11.4) | 14 (11.7) |
| Esophageal intubation | 6 (2.4) | 5 (3.8) | 1 (0.8) |
| Bronchoaspiration | 3 (1.2) | 1 (0.8) | 2 (1.7) |
Data expressed as numbers (%). There are no significant differences between the two groups of patients.
After the multivariate analysis adjusted by factors prior to intubation, no factors significantly associated to the occurrence of complications were found, except for the presence of Cormack ≥3 (p=0.01; p=0.054 after penalization; AUC-ROC=0.58).
No factors independently associated with the difficulty of intubation were found either, except for the BMI (p=0.02; p=0.054 after penalization; AUC-ROC=0.59).
DiscussionThe period of time including nights and weekends is known as off-hours schedule. During the last few years, numerous studies have been published associating the moment of hospital admission in this off-hours schedule with higher mortality rates.1–4 In the present study, we were unable to associate a higher incidence rate of complications or technical difficulties in the orotracheal intubation procedures conducted in our CCU to this off-hours schedule compared to the on-hours schedule.
Unlike our study, a recent study conducted in Japan by Ono et al.8 that analyzed 123 intubations observed a higher incidence rate of complications associated with intubations conducted in the off-hours schedule (42.7%) compared to the on-hours schedule (22.9%). The authors give three (3) possible explanations for the results obtained. In the first place, in Japan, at night time or during the weekend, medical personnel shortage is something customary, which in turn worsens the healthcare provided to critically ill patients who require intubation, above all, with patients with difficult airways. Secondly, the rank and experience of the physicians who take care of the night shift or work during the weekend is usually lower than that of those who work during the day. And thirdly, the fatigue accumulated by these physicians after many hours of work may be influencing the incidence rate of complications associated with intubations found in their study. In an observational retrospective study conducted by Carrol et al.9 in a pediatric ICU, they also saw a higher incidence rate of complications during emergent intubations conducted during the off-hours schedule. In their study, the intensivist pediatrician was not available at the hospital 24 hours a day. The authors say that having one intensivist available at the hospital 24 hours a day might reduce the incidence rate of complications while recognizing those who may require intubation.
In our study, we did not find a higher incidence rate of complications in the so-called off-hours schedule. Having an adequate number of nurses10 and two (2) assistant physicians experienced in airway intubations available at our CCU 24 hours a day could be the reason why we did not find any differences in the incidence rate of complications associated with orotracheal intubation procedures during the 2 periods in our study. Several studies11–13 have already demonstrated that having one intensivist physician available at the CCU 24 hours a day associates lower mortality rates, and that the presence of a second staff member at the CCU associates lower incidence rates of complications during orotracheal intubation procedures. Also, the supervision of physicians experienced in intubating airways has been associated with a lower incidence rate of complications during emergent intubations.14 Therefore, we can see here that human resources play a significant role in the management of airways of patients admitted to CCUs.
In two former studies,15,16 and although the study main goal was not the same as ours, they obtained similar results. Jaber et al.15 conducted a study in 9 French ICUs and did not find differences in the number of complications occurred during the intubation procedures conducted during day time or during the off-hours schedule. Martin et al.16 found similar results after analyzing 3423 emergent intubations conducted outside the OR: they did not find a higher incidence rate of complications in the intubations conducted during the off-hours schedule.
After seeing these results, we believe it is important to try to maintain an organizational structure at the CCU that remains homogeneous throughout the day, at night time, and during the weekends. These efforts should be aimed at keeping the same number of nurses, assistants, and physicians, while guaranteeing the level or capacity of all the healthcare providers who take care of these units during the night, national holidays, or during the weekends. In one meta-analysis published in Chest back in 2010, Cavallazzi et al.2 reported that patients who were admitted to the ICU during the weekend had an 8% higher risk of death compared to those admitted during the week. They concluded that the organizational difference of these units during the weekend or during the week may explain the higher mortality rate described. Some of the causes included a lower number of intensivists, less experienced doctors on call and of a lower rank and fatigue itself. Human resources play an important role in the prognosis of patients at the CCU setting.
Several authors claim that conducting different hospital interventions during the night shift or during the weekend was accompanied by a higher incidence rate of complications and worse results.17–21 For example, it was reported that the off hours schedule was associated with adverse events in patients with pulmonary embolism,17 cerebral infarction,21 cardiac arrest,19 myocardial infarction20 or ruptured aortic aneurysm.1
Our study secondary goal was to compare how difficult it was to conduct intubation procedures during the night shift or during the weekend compared to the intubation procedures conducted during the day. In order to measure the difficulty of the intubation procedure, we used several parameters such as the Cormack–Lehane scale, the number of laryngoscopies required for the intubation procedure, the need for additional material for the intubation, or the difficulty of the intubation procedure according to the physician. In our study we found greater difficulty intubating during the off-hours schedule than in the on-hours schedule. We did not find any studies that compared how difficult intubation was in the aforementioned two schedules.
Our study has some limitations though. The most important one is that it was conducted in one single center only. We should bear in mind that the very organizational system of every hospital, and even every unit within the same hospital, can influence the results. Another limitation would be the definition of on-hours schedule and off-hours schedule. We observed that in different studies the definitions of these two schedules are different, which may difficult the comparison. Also, the definition of complications varies from one study to the next which is why in the present study we distinguished between hypoxia <90% and <80%, and hypotension <80 and <65% mmHg.
In sum, the intubation procedures conducted in our CCU during the off-hours schedule could not be associated with higher incidence rates of complications or with a more difficult technique of intubation. We believe that human resources play a significant role in the prognosis of patients admitted to the CCU in the sense that there are no differences in the complications associated with the intubation procedure of critically ill patients regardless of the moment of the day when the patient is intubated.
Conflicts of interestsThe authors declare no conflicts of interests associated with this article whatsoever.
Please cite this article as: Taboada M, Calvo A, Doldán P, Ramas M, Torres D, González M, et al. ¿Tiene más complicaciones la intubación orotraqueal en las Unidades de Cuidados Críticos durante el periodo llamado off-hours? Estudio prospectivo y observacional. Med Intensiva. 2018;42:527–533.