Undergraduate and postgraduate medical education has traditionally been based on theoretical learning, acquiring clinical skills through the direct treatment with patients. Over the last few decades, patient's safety and ethical imperatives have been focusing on the patient's protection and, as a matter of fact, learning via trial and error is ill-advised on current patients.1 In this context, clinical simulation has been developed as a teaching tool to provide comprehensive training that is risk-free for the patients.2 Its use has been growing in clinical areas such as anesthesiology, intensive medicine, and emergencies, but above all it has focused on postgraduate training.3 Medical students receive for the most part vertical training where the use of clinical simulation is just a formality. In this context, clinical simulation with medical students has focused on cases of shock, approach to sepsis or advanced life support, but for severe traumatic injury it is more limited.4–6
A simulation activity was conducted at our service focused on severe traumas for 6th-year medical students during their intensive medicine practices. The objectives were to assess the effectiveness of simulation in the management of severe trauma among the students and determine their perceptions on the suitability of simulation for technical skills.
A cross-sectional prospective study was conducted with 6th-year medical students during their rotation at the intensive medicine unit of Hospital Universitario Marqués de Valdecilla, Spain in the 2017–2018 school year. High-fidelity simulation scenarios on Severe traumatic disease were used with groups of 8 students each. Each clinical case was developed by 2 students. They received a briefing session prior to developing each scenario. Each and every one of the cases was developed in a 15-min. period. The simulation was followed in real time by the rest of the workshop students. At the end of each case, a second 15-min. debate session was conducted to analyze how the case was developed and how the decisions were made. They were asked to make a voluntary assessment of the activity through questionnaires using the 5-point Likert scale (1=complete disagreement, 5=complete disagreement) and open questions. Some of the variables were evaluated before and after the teaching activity. All answers were anonymous.
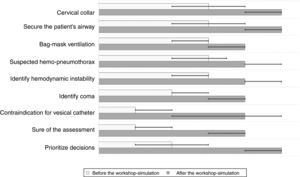
There were 84 students, 64.5% of them women. Their mean age was 24 years (SD 1.2). The resources available, as well as the design of the activity were assessed positively. Also, the closeness and accessibility of the teaching staff were highlighted (Table 1). Fig. 1 shows the self-evaluation of the capacities analyzed before and after the training activity. The degree of confidence acquired by the students after conducting the activity was significantly higher compared to the previous one, which underlines the greater capacity for leadership and make decisions before a case of Severe traumatic disease (Fig. 1).
Assessment of the simulation workshop “Severe traumatic disease”.
| Objectives and content | |
| The duration of the course was suitable | 4 (IQR 4–5) |
| The in-depth level of the topics was suitable | 4 (IQR 4–5) |
| The content of the course fulfilled my training needs | 5 (IQR 4–5) |
| The objectives of the course were achieved | 5 (IQR 4–5) |
| Methodology | |
| The methodology used was the most suitable one for the objectives and contents | 4.5 (IQR 4–5) |
| The methodology used enabled active participation | 5 (IQR 4–5) |
| The practices were useful and enough | 5 (IQR 4–5) |
| Utility | |
| The expectations I had regarding the utility of the workshop have been met | 4 (IQR 4–5) |
| The contents of the course have proven useful and met my expectations | 5 (IQR 4–5) |
| I am going to be able to apply the knowledge acquired to my professional clinical practice | 5 (IQR 4–5) |
| Means | |
| The technical means have worked correctly during the workshop | 4 (IQR 3.5–5) |
| The facilities have made learning easier | 4 (IQR 4–5) |
| Teaching staff | |
| The teaching staff exhibited good competence level | 5 (IQR 5–5) |
| The teaching staff managed to maintain a good level of awareness | 5 (IQR 5–5) |
| The teaching staff prompted debate and discussion and was close to the students | 5 (IQR 5–5) |
Categorical variables were expressed as median and interquartile range (IQR).
Evaluation of skills in clinical care to polytraumatized patients. The bar represents the median and the error bar the interquartile range (P25 and P75).
The Wilcoxon signed-rank test was used to analyze change in the skills evaluated. Significance level (p) was <.001 in all of them.
Hm., hemodynamic.
Similarly, the students underlined teamwork and the acquisition of leadership skills in the first person. They suggested increasing the frequency of these activities and expanding their use in the different academic courses. As positive points, they assessed the possibility of facing clinical cases (11 students), the practical character (32 students), and the possibility of participation in the first person (7 cases). Ninety-one-point-four per cent rated the course as excellent.
High-fidelity simulation allowed students to perform in a clinical scenario using the same resources they will have available in their routine clinical practice. On the other hand, it allowed the detection of possible improvements for future editions and adapt it to the vision contributed by the students. Finally, it made student self-evaluation easy, confirming its role as an effective tool for educational practices.
The students’ knowledge prior to post-simulation increased significantly and their confidence in being able to handle severe trauma improved as well. These aspects are consistent with previous experiences above all regarding nursing students,7,8 where this teaching tool is more established. A vertical, more individualistic learning focused on the academic performance of medical studies could explain this difference.
It has been reported that throughout their university training students do not have defined objectives to attain in terms of technical skills, unlike knowledge goals that are clearly established.9 Simulation may be useful as a teaching tool to complete that technical profile of the students. However, generalizing clinical simulations in the Medical Science syllabus has not been achieved. It has been postulated that technical and economic requirements and the need for a large staff properly trained are obstacles for this consolidation. Nevertheless, data that question the “actual” cost of medical education are scarce and controversial.2 The experience gained in other disciplines like nursing, along with its generalization in postgraduate training, suggest that there may be a place for it in the undergraduate studies of Medical Schools.
The development of experiences like ours has brought Intensive Medicine closer to Medical students. Also, these conclusions are consistent with simulation projects from other disciplines like neurosurgery.10 This is another strong point of simulation, that it allows filling the existing gap between academic training and actual medical practice. This reflects the need to modify syllabi to engage students in their medical specialty and complement clinical knowledge with suitable practical skills. We believe that student motivation can be enhanced through the use of simulations. Producing highly competitive medical professionals in the coming years would result in a future generation of well-trained intensivists.
The work has limitations. There was one group of students only. Subjective opinions have been assessed and the effectiveness of skill acquisition in the clinical practice was not measured. It was conducted in one center only with a relatively small sample size, which is why it cannot be generalized to other simulation scenarios.
Clinical simulation can facilitate clinical reasoning and the acquisition of technical skills. Severe traumatic disease is a good model because it requires a systematic approach, the cross-sectional integration of knowledge, developing leadership, and a correct decision-making process. Our pilot study suggests the possibility of including clinical simulation in the undergraduate training of Medical students. On top of facilitating the acquisition of practical skills, it brings students closer to the Intensive Medicine specialty.
Conflicts of interestNone reported.
Please cite this article as: Ballesteros MA, Feo González M, Suberviola B, Miñambres E. Simulación clínica en el paciente politraumatizado. Aplicación en estudiantes de Medicina. Med Intensiva. 2020;44:389–391.