To analyze the clinical indications for use, morbidity and mortality associated with a non-permanent transvenous pacemaker.
DesignProspective and observational study.
SettingCardiac intensive care unit.
MethodOne hundred and eighty-two patients with non-permanent pacemakers implanted consecutively over a period of four years.
Data collectedMain variables of interest were demographic data, clinical indications, access route, length of stay and complications.
ResultsA total of 63% were men, with a median age of 78±9.5 years and with symptomatic third-degree atrioventricular block in 76.9% of the cases. Femoral vein access was preferred in 92.3% of the cases. Complications appeared in 40.11% of the patients, the most frequent being hematoma at the site of vascular access (13.19%). Restlessness was associated to the need for repositioning the pacemaker due to a shift in the electrode (p=0.059) and to hematoma (p=0.07). Subclavian or jugular vein lead insertion (p=0.012; OR=0.16; 95%CI, 0.04–0.66), restlessness during admission to ICU (p=0.006; OR=3.2; 95%CI, 1.4–7.3), and the presence of cardiovascular risk factors (p=0.042; OR=5; 95%CI, 1.06–14.2) were identified by multivariate analysis as being predictors of complications. Length of stay in ICU was significantly longer when lead insertion was carried out by specialized staff (p=0.0001), and in the presence of complications (p=0.05).
ConclusionsPredictors of complications were restlessness, cardiovascular risk factors, and insertion through the jugular or subclavian vein. Complications prolonged ICU stay and were not related to the professionals involved.
Analizar las características clínicas, indicaciones y morbimortalidad asociada a la implantación de marcapasos transvenosos transitorios.
DiseñoEstudio observacional y prospectivo.
ÁmbitoUnidad de cuidados intensivos cardiológicos.
PacientesSe implantó marcapasos transvenoso transitorio a 182 pacientes, en un periodo de 4 años.
Variables recogidasSe registraron variables demográficas, clínicas, indicaciones, vía de acceso, días de estancia en la unidad y complicaciones.
ResultadosEl 63% eran hombres, con una media de edad de 78±9,5 años con bloqueo auriculoventricular sintomático en un 76,9% de los casos. La vía venosa de abordaje habitual fue la femoral (92,3%). El 40,11% sufrió complicaciones, siendo la más frecuente el hematoma en la zona de punción (13,19%). No hubo diferencias entre el profesional que implantó el marcapasos y la aparición de complicaciones. La agitación psicomotriz se asoció a la existencia de hematoma en la zona de punción (p=0,07) y a la necesidad de movilización del catéter (p=0,059). Se identificó la vía de inserción no femoral (p=0,012, OR=0,16; IC del 95%, 0,04-0,66), la agitación (p=0,006; OR=3,2; IC del 95%, 1,4-7,3) y la presencia de factores de riesgo cardiovascular (p=0,042; OR=5; IC del 95%, 1,06-14,2) como predictores de complicaciones. La realización del procedimiento por parte del personal especializado (p=0,0001) y la presencia de complicaciones (p=0,05) incrementaron la estancia en la unidad.
ConclusionesLa presencia de agitación, los factores de riesgo cardiovascular y la inserción a través de la vena subclavia o yugular fueron predictores de complicaciones. Estas no se relacionaron con el tipo de profesional implicado en la implantación, pero incrementaron la estancia en la unidad.
The implantation of a non-permanent transvenous pacemaker (NPTP) is common practice in Intensive Care Units (ICUs). This type of electrical pacing was first described in the 1950s.1 It allows the maintenance of an adequate and stable cardiac rhythm in patients with asystolia and/or extreme bradycardia,2 by means of an electrocatheter implanted through a central vein and opening up into the endocardium of the right ventricle–stimulating the latter and ensuring an adequate cardiac output under concrete circumstances.3
In most cases, NPTPs are placed in situations of extreme emergency, since the patients involved present unstable conditions, and are mostly elderly, and scantly cooperative. As a result, complications may develop.2,4–14 There is generally considerable variability in the infrastructure supervising NPTP implantation and posterior care. This is a crucial issue in relation to the prevention of morbidity–mortality associated to the procedure, since implantation in a sterile operating room specifically prepared to the effect is not the same as implantation in rooms with limited supporting systems. Another important conditioning element is the professional in charge of implanting the electrocatheter (specialist or physician in training).
The use of non-permanent transvenous or endocardial pacing was gradually incorporated to most hospitals since the 1960s, and its main indication remains symptomatic bradycardia. These systems can also be used as a bridging measure in patients requiring implantation of a permanent pacemaker in advanced second- and third-degree block. Other indications based on lesser levels of evidence have also been well established by the American College of Cardiology/American Heart Association (ACC/AHA).15
A subgroup of patients requiring special vigilance are those individuals presenting atrioventricular block (AVB) in the context of acute myocardial infarction (AMI). There is a belief that such block implies increased mortality, though the latter is not related to the alteration in cardiac rhythm but rather to the size of the infarction.4 Accordingly, the use of NPTP is recommended in the case of symptomatic sinus bradycardia or with hemodynamic impairment and sinus node arrest or pause lasting over 3s, as explained in the most recent ACC/AHA guides.16
The incidence of complications in the implantation of NPTP varies from 10 to 60%, as reflected by the few recent publications available. Complications can develop particularly in patients requiring pacing for over 48h,17 and are also dependent upon other factors such as the need for a basic infrastructure for applying NPTP, prior training, and sufficient experience on the part of the professionals performing the technique.2,18 In our hospital, the implantation of these devices is carried out by intensivists in an adequately equipped room, since in many cases pacemaker placement is carried out under emergency conditions and in patients with AMI or in extremely serious condition.
Patients and methodsA prospective, systematic observational study was made of all non-permanent pacemakers consecutively implanted in our ICU in adult patients (over age 18 years) during the period between 2004 and 2008. The purpose of the study was to analyze the efficacy and safety of the technique, as related to mortality and the appearance of complications associated with implantation of the electrocatheter and the duration of patient stay in the unit.
Cases in which the signing of informed consent was not obtained (from the patient, relatives or legal representatives) were excluded from the study.
Epidemiological variables were recorded, together with clinical data and information on the indications, access routes, stay in the unit and days elapsed until implantation of the permanent pacemaker. We also registered the incidence of complications directly attributable to the NPTP implantation technique, from placement to withdrawal, as well as their possible relationship to the professional performing the procedure (specialist or physician in training). Pacemaker dysfunction was defined as capture failure, sensing failure, or both. Mortality due to any cause was also documented.
The study data were obtained by the supervising physician after execution of the technique and during patient stay in the corresponding unit, as defined by the established protocol.
All the procedures were carried out in an exploration room belonging to the Department, with the help of an image intensifier (Radiocol images®, Kodak Corporation, NJ, USA). The electrocatheters used were 125cm bipolar devices of caliber 6F (Bard Electrophysiology Division®). Catheterization was generally through the right femoral vein using the Seldinger technique, with insertion in the apex of the right ventricle under radioscopic control according to the usual technique. An adequate pacing threshold was considered for values of 0.5–2mV. Temporary pacing was initially established at voltage values double the threshold value, using Medtronic® generators in VVI mode.
The data were processed and analyzed using the SPSS version 15.0 statistical package. Quantitative variables were expressed as the mean and standard deviation (SD) or median, while qualitative variables were reported as frequencies and percentages, or median, depending on the type of data distribution involved. In the case of the quantitative variables, comparisons between groups were made using the Student's t-test and analysis of variance (ANOVA), while in the case of the qualitative variables the comparisons were made with the chi-squared test–establishing the strength of the associations from the corresponding odds ratios (ORs). Multivariate linear and logistic regression analysis in turn was used to identify possible predictors of the dependent study variable. In all cases an alpha error of under 5% was considered.
ResultsA total of 182 pacemakers were implanted (63.2% in males), the mean patient age being 78±9.5 years. The most frequent clinical antecedents of the patients are reported in Table 1.
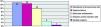
A total of 81.9% of the patients presented some cardiovascular risk factor, and 32.4% were receiving some negative chronotropic medication. The most frequent indications for NPTP implantation are shown in Fig. 1, and corresponded to complete AVB and symptomatic high-grade block (66.5% and 10.4% of the cases, respectively). Only four patients suffered complete AVB in the context of AMI.
In all cases chest X-rays were obtained to check correct positioning of the electrode, together with an electrocardiogram reflecting left bundle block after implantation. In most cases we administered low-molecular weight heparin via the subcutaneous route, at prophylactic doses.
The femoral vein was the most commonly used route (92.3%), followed by the internal jugular vein (5.5%) and subclavian vein (2.2%). A total of 62.1% of the NPTPs were implanted by ward physicians, and 37.9% by residents in training. The median time to implantation of a permanent pacemaker was two days.
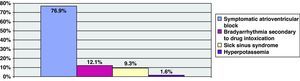
Complications were recorded in 40.11% of the cases (73 patients). Fig. 2 shows the absolute and relative frequencies of the observed complications – the most frequent problem being bruising at the venous puncture site and pacemaker dysfunction in the form of capture failures. There were no cases of deep venous thrombosis, arrhythmias or pneumothorax. Restlessness was recorded in 45.6% of the admitted patients, with a mean age of 89.46±9.8 years (range 42–99), which was significantly older than in the case of the patients without restlessness (76.43±9 years) (p=0.004).
The univariate analysis showed insertion of the pacemaker using a non-femoral route, the existence of cardiovascular risk factors – specifically arterial hypertension – and the presence of restlessness to be significantly correlated to the appearance of complications. On the other hand, the femoral venous access entailed a lesser risk of bruising at the puncture site (p=0.0001; OR=0.036; 95%CI, 0.010–0.13), probably because such access is easy and is employed for catheterization in cases of extreme emergency.
The multivariate logistic regression analysis identified the following factors as predictors of complications: restlessness, the use of a non-femoral catheter insertion route, and the presence of cardiovascular risk factors (Table 2).
Univariate and multivariate analysis of the factors predicting complications.
| Variables | Univariate, p/OR (95%CI) | Logistic regression, p/OR (95%CI) | |
| Age | 78±9 | NS | NS |
| Males/females | 115 (63.2%)/67 (36.8%) | NS | NS |
| Specialist/resident | 113 (62.1%)/69 (37.9%) | NS | NS |
| Femoral/non-femoral venous access | 168 (92.3%)/14 (7.7) | 0.006/0.18 (0.05–0.6) | 0.012/0.16 (0.04–0.66) |
| Indication of implantation | Fig. 1 | NS | NS |
| Risk factors | Table 1 | 0.08 | 0.042/5 (1.06–14.2) |
| Arterial hypertension | 0.034/2.09 (1.05–4.1) | NS | |
| Restlessness | 83 (45.6%) | 0.0001/1.8 (1.3–2.4) | 0.006/3.2 (1.4–7.3) |
NS: nonsignificant.
As has been mentioned, the presence of restlessness was a determinant factor in the appearance of complications. On categorizing according to the type of complication, no statistically significant association was observed between the presence of restlessness and the existence of bruising at the venous puncture site (p=0.07), or the need for catheter mobilization (p=0.059).
The overall mortality rate was 1.6% (3 patients). One patient died as a result of massive cardiac tamponade secondary to cardiac rupture after removing the pacemaker electrocatheter. The other two patients died of septic shock and multiorgan failure after pneumonia, following cardiac arrest and massive bronchial aspiration, respectively.
The median duration of stay in the unit was 3 days. Table 3 shows the variables associated to a longer average stay in the univariate analysis: performance of the procedure by a specialist versus a resident, the presence of restlessness, and certain complications (infection or bruising at the puncture site) imply the need to administer treatment, and therefore to delay implantation of the permanent pacemaker. The multivariate analysis yielded similar results referred to the professional performing the technique, and showed that the presence of complications (e.g., infection at the insertion site) requiring the start of treatment and the performance of tests to discard complications, or pacemaker dysfunction due to defective placement, restlessness, or the need to perform continuous cardiac pacing, both made it necessary to prolong patient monitorization and thus prolong admission to the unit.
Analysis of the factors conditioning patient stay in the unit.
| Variables | Univariate, p | Multivariate, p | |
| Age | 78±9 | NS | NS |
| Males/females | 115 (63.2%)/67 (36.8%) | NS | NS |
| Specialist/resident | 113 (62.1%)/69 (37.9%) | 0.0001 | 0.0001 |
| Indication of implantation | Fig. 1 | NS | NS |
| Risk factors | Table 1 | NS | NS |
| Restlessness | 83 (45.6%) | 0.041 | NS |
| Chronic renal failure | 12 (6.6%) | 0.054 | NS |
| Complications | 0.015 | 0.05 | |
| Hematoma | 24 (13.2%) | NS | NS |
| Capture failure | 23 (12.6%) | NS | 0.028 |
| Electrode displacement | 18 (9.9%) | NS | NS |
| Infection | 5 (2.7%) | 0.013 | 0.0001 |
| Deaths | 5 (2.7%) | NS | NS |
NS: nonsignificant.
Our series showed an important complications rate (40.11%), despite the fact that NPTP is a common and protocolized technique in our unit, performed by experienced personnel in adequately equipped rooms. The different series published in the literature (Table 4) report similar and sometimes even much higher complications rates, though the underlying causes and insertion routes differ.
Summary of the published series on non-permanent transvenous pacemaker (NPTP) implantation.
| Author, year | Cases, n (%) | Age, mean | Subclavian vein | Internal jugular vein | Femoral vein | Antecubital vein | Complications, n (%) |
| Lumia9, 1973 | 142 (3.8%) | 81 (57%) | 61 (43%) | 85 (59.9%) | |||
| Austin10, 1983 | 100 (2.6%) | 0 | 0 | 81 (81%) | 19 (19%) | 57 (57%) | |
| Hynes19, 1983 | 1022 (27.2%) | 68.2 | 177 (17.3%) | 111 (10.9%) | 48 (4.7%) | 606 (59.3%) | 323-140 (31.6%-13.7%) |
| Krueger27, 1983 | 126 | 23 (18%) | |||||
| Donovan11, 1985 | 148 (3.9%) | 108 (73%) | 27 (18%) | ||||
| Abinater12, 1987 | 339 (9%) | 81 (24%) | 14 (4%) | 3 (1%) | 241 (71%) | ||
| Winner13, 1989 | 145 (3.8%) | 74.4 | 135 (93.1%) | 6 (3.4%) | 0 | 4 (2.1%) | 74 (51%) |
| Volkman, 1989 | 591 (15.7%) | 219 (37.1%) | |||||
| Jowett26, 1989 | 162 (4.3%) | 60.5 | 162 (100%) | 0 | 0 | 0 | 32 (19.8%) |
| Andrews28, 1992 | 40 (1.1%) | 21 (52.5%) | |||||
| Rashid29, 1993 | 50 (1.3%) | 65 | 5 (10%) | ||||
| Murphy5, 1996 | 194 (5.2%) | 71 | 132 (68%) | 36 (18.5%) | 26 (13.5%) | 0 | 44 (22.6%) |
| Betts7, 2003 | 111 (3%) | 75 | 52 (46.8%) | 37 (33.3%) | 22 (19.8%) | 0 | 31 (27.9%) |
| Ayerbe2, 2004 | 530 (14.1%) | 74.8 | < 1% | < 1% | 99% | < 1% | 101 (19.1%) |
| Birkhahn30, 2004 | 117 (3.1%) | 77.8 | 4 (3.4%) | 113 (96.6%) | 0 | 0 | 29 (25%) |
| Lancs, 2005 | 56 (1.5%) | 78 | 10 (18%) | 43 (76%) | 3 (6%) | 0 | 18 (32%) |
| Total | 3.747 | 70.8 | 26.5% |
Reproduced from McCann.20
The femoral route was used in our study, because of its easy access and compressibility in the event of bleeding. López Ayerbe et al.2 also mainly used this route. In contrast, Murphy5 and the group of Hynes et al.19 showed a preference for the jugular route, followed by the subclavian vein. The review published by McCann20 in 2007 concluded that the internal jugular route involves the fewest complications, and moreover causes the fewest infections. The highest infection rate has been associated to use of the antecubital vein (Table 4). Other authors have postulated the internal jugular route adopting the infraclavicular access as the venous route with the fewest complications and affording the greatest efficacy and safety.21 This access was not used in our series, however.
Patient restlessness was found to be a relevant risk factor for complications in our study. Bruising in the venous access zone was the most common complication, particularly when coinciding with restlessness, together with the need for implanted catheter displacement in order to optimize operability. Over 92% of our patients were treated with fractionated heparin, generally on a prophylactic basis and via the subcutaneous route before carrying out the procedure. However, in the series of López Ayerbe2 and Betts,7 hematomas were considerably less frequent, despite the fact that over 95% of the patients received fractionated heparin at prophylactic doses – pacemaker migration being the most common complication in these series. It should be mentioned that in the series of Bett, the venous access was predominantly of a non-femoral nature, in contrast to our series.
Regarding infection at the puncture site, our percentage incidence (2.7%) was slightly higher than in other studies such as those of Murphy5 (1.7%) or Morgan et al.22 (1%). None of our cases developed septic problems. These results justify strict observation of asepsis, despite the emergency nature of NPTP placement. The most effective way of preventing pacemaker-associated infection is to use a meticulous surgical technique during placement, including careful preparation of the skin, precise localization of the cutaneous incision site, the adoption of strict aseptic measures, effective hemostasis, and the avoidance of drains.23 It is not common to use antibiotic prophylaxis, and in fact such medication was not used in our patients. Some authors recommend systematic antibiotic use, while others reserve such treatment for more prolonged procedures.23
Another complication, pacemaker dysfunction due to capture failure, was recorded in 12.6% of our cases. Similar figures have been reported by López Ayerbe (9%), with clearly higher rates in the series of Murphy8 (19%) and Ochoa et al.24 (42%). In our case, patient restlessness was found to be a risk factor for the presence of complications in general, and of catheter migration in particular, independently of the emergency with which the technique was performed. Given the high incidence of such migration, Lumia et al.9 considered continuous electrocardiographic monitoring to be indicated in these patients until the time of permanent pacemaker implantation, in order to ensure the early detection of possible dysfunction. In our center, all patients admitted for this reason remain under continuous monitorization for as long as they carry the NPTP, though the practice varies in different hospitals.
On the other hand, we found no association between morbidity derived from the NPTP implantation procedure and the physician in charge of performing the technique. Although the procedure was carried out by residents in training in over one-third of the cases, there are no reasons for linking the incidence of complications to this fact – among other reasons because resident intervention centered on the most clinically stable patients, with close specialist supervision. In contrast, Betts7 considered resident status to be a risk factor for complications, compared with the specialized intensivist. Likewise, Murphy5 initially attributed the high rate of complications to the limited training of the younger physicians, and to scant supervision by the more experienced specialists, among other factors. Brown and Thwaites6 raised the question of whether the technique should be reserved only for specialists–whether cardiologists, anesthetists or intensivists–in order to lessen the number of complications. Years later, Murphy continued the controversy regarding the professionals best suited for performing the technique–insisting on the need for adequate and exhaustive training of the largest number of physicians possible, in view of the risks involved.8 In this sense, McCann considered that pacemaker implantation by experienced physicians could reduce the number of complications.20 In our series there was only one case of cardiac wall perforation by the electrocatheter, that was diagnosed by transthoracic echocardiography. This frequency may seem a little low compared with other publications, since it is not common in our center to perform echocardiography on a protocolized basis after pacemaker implantation, except when perforation is clinically suspected; as a result, this complication may have been underdiagnosed.
The indications of insertion likewise did not prove decisive in relation to the incidence of complications. Our indications for NPTP were similar to those of other authors such as Murphy et al., who found the main indications to be complete AVB and, to a lesser degree, AVB secondary to AMI.5 Similar data have been published by Ochoa et al.24 and Canabal Berlanga et al.25 In our series complete AVB predominated (66.5%), together with symptomatic high-grade block (10.4%), while AMI was implicated in the evolution of the former in only 3.3% of the cases.
On examining the earlier studies, the impression might be that the indications have changed over time. In effect, before the 1990s, the series published by Jowet et al.26 described AVB in patients with AMI to be the most frequent indication. Posteriorly, this indication tended to decrease, as clearly confirmed in our own study. The introduction of thrombolytic therapy in the last few decades may have played a relevant role in this phenomenon, since the early restoration of coronary blood flow in many cases allows the restoration of normal cardiac rhythm, by reducing ischemia of the cardiac excitation–conduction system.
Thus, the results of our study offer new lines of investigation, after identification of possible areas for improvement, such as infection control or the protocolized management of patient restlessness, with a view to increasing the efficacy and safety of this procedure.
Since this is not a multicenter study but rather a series limited to a single third-level hospital, its external validity is limited to centers in our setting with similar degrees of healthcare complexity–though the most recent publications on this technical procedure offer results and conclusions that are similar in many aspects to our own. We believe that there is presently sufficient knowledge and experience for conducting a multicenter prospective study capable of defining good clinical practice and safety guidelines related to the use of this technique.
In conclusion, NPTP is both useful and effective when applied in relation to the specified indications, though the procedure is not without associated morbidity. Serious complications are the least common problems, and the predictors of morbidity comprise patient restlessness, the presence of cardiovascular risk factors, and catheter insertion through the subclavian or jugular vein. Those patients with complications required a longer stay in the unit. Mortality directly related to the procedure was found to be low.
Financial supportNone.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Muñoz Bono J, et al. Eficacia y seguridad de la implantación de marcapasos transvenosos transitorios en una unidad de cuidados intensivos. Med Intensiva. 2011;35:410-6.