Edited by: Federico Gordo. Intensive Care Service of Hospital of Henares, Madrid, Spain
Last update: April 2025
More infoThe severity of the critically ill patient, the practice of diagnostic procedures and invasive treatments, the high number of drugs administered, a high volume of data generated during the care of the critically ill patient along with a technical work environment, the stress and workload of work of professionals, are circumstances that favor the appearance of errors, turning Intensive Medicine Services into risk areas for adverse events to occur. Knowing their epidemiology is the first step to improve the safety of the care we provide to our patients, because it allows us to identify risk areas, analyze them and develop strategies to prevent the adverse events, or if this is not possible, be able to manage them.
This article analyzes the main studies published to date on incidents related to safety in the field of critically ill patients.
La gravedad del paciente crítico, la práctica de procedimientos diagnósticos y tratamientos invasivos, el alto número de fármacos que se administran, un elevado volumen de datos generados durante la atención al paciente crítico junto con un ambiente de trabajo tecnificado, el estrés y la carga de trabajo de los profesionales, son circunstancias que favorecen la aparición de errores convirtiendo a los Servicios de Medicina Intensiva en áreas riesgo para que se produzcan eventos adversos. Conocer la epidemiología de estos, es el primer paso para mejorar la seguridad de la asistencia que prestamos a nuestros pacientes, porque permite identificar las áreas de riesgo, analizarlas y desarrollar estrategias para prevenir los eventos adversos, o si no es posible, ser capaces de gestionarlos.
En este artículo se analizan los principales estudios publicados hasta la fecha sobre incidentes relacionados con la de seguridad en el ámbito de paciente crítico.
As has been shown by many national and international publications, the complexity of clinical practice implies that all healthcare is associated with some risk for the patient, which may give rise to an adverse event (AE). This risk is found at all levels of healthcare,1–3 though in the concrete case of Intensive Care Medicine it is even greater, due to several reasons. On one hand, mention must be made of the severity of the critically ill patient, the use of invasive diagnostic and therapeutic procedures, and the administration of a large number of drugs – many of which pose a high risk and are used via the intravenous route. On the other hand, this scenario also implies a great volume and complexity of data generated in the course of critical patient care,4 which requires close communication between professionals.5 Other influencing factors are a technified workplace, stress, professional workload6 and the safety culture found in the Department.7–9
These circumstances favor the appearance of errors and define the Department of Intensive Care Medicine (DICM) as a risk setting for the appearance of AEs.
Incidents related to patient safety in the critically illKnowledge of the epidemiology of AEs is the first step for improving the safety of patient care, since it allows us to identify areas of risk, analyze them, and develop strategies to prevent AEs or, if these cannot be avoided, to manage them appropriately (reduce their impact, reduce their frequency, or increase their detection).
An analysis is provided below of the main studies published to date on AEs in the critical care setting.
International studiesOne of the first multicenter studies was the Australian Incident Monitoring Study in Intensive Care Units (AIMS-ICU).10 This study aimed to detect the most frequent risks to define preventive strategies and design training programs. A voluntary and anonymous national reporting system was used, with the participation of 100 Intensive Care Units (ICUs). A total of 610 incidents were identified – the most frequent being related to medication (28%), procedures (23%) and the patient airway (20%). Of note is the observation that none caused serious harm to the patient. Since then there have been no further combined analyses, though there have been reports on concrete incidents, making it possible to assess the magnitude of the AEs related to the airway,11 arterial catheters,12 within-hospital transfer13 and to nursing staff inexperience and workload.14
In the United States, the Society of Critical Care Medicine, in collaboration with the Australian Patient Safety Foundation and the Agency for Research and Quality in Health Care, developed another reporting system methodologically inspired by the Australian system: the ICU Incident Safety Reporting System (ICUSRS).15 A total of 2075 incidents were reported, mostly related to medication (42%), care (20%), equipment (15%) and catheters, tubes and drains (13%). Forty-two of these incidents caused harm to the patient, particularly those referred to catheters, tubes and drains, and equipment. Patient death occurred in 0.8% of these incidents.
In turn, the European Society of Intensive Care Medicine carried out the Sentinel Events Evaluation (SEE).16 This was a multicenter study with an incidental cut-off period of one day, carried out in 205 ICUs in 30 countries, including Spain. It aimed to determine the incidence of AEs related to medication (wrong dose, drug or administration route), airway (non-planned extubation, artificial airway obstruction, cuff leakage with reintubation), intravascular catheters, tubes and drains (accidental removal, inappropriate disconnection), equipment failure (infusion devices, respirator, renal replacement devices, oxygen supply) and alarms (inadequate suspension). A total of 584 incidents were recorded, representing 38.8 AEs per 100 patients-day (95% confidence interval [95%CI]: 34.7–42.9). Most of the incidents were related to tubes, drains and catheters (35.1%), followed by medication (23.2%) and equipment (22%).
Using the same methodology, the SEE was followed by a study focused on AEs exclusively related to the administration of parenteral medications.17 A total of 113 DICMs from 27 countries (including 8 Spanish centers) participated in the study. The sample consisted of 1328 patients, with the recording of 861 medication errors (MEs) in 441 patients. The incident rate was 74.5 per 100 patients-day (95%CI: 69.5–79.4), and 0.9% of the patients suffered permanent injury or died due to a ME. Antimicrobials, sedatives and analgesics were the drugs behind most of the incidents, and the most frequent causes were wrong administration frequency (44.8%), dose omission (30%), incorrect dose (13.7%) and wrong administration route (4.2%).
Likewise, to know the prevalence of MEs, another prospective cohort study was carried out, with the participation of 7 DICMs.18 The study sample consisted of 696 patients, with the identification of 52 MEs, of which 28 (53.8%) resulted in possible damage and 24 (46.2%) resulted in actual damage to the patient. There were 7.7 MEs per 1000 days-patient. Most of the errors were referred to prescription (71.1%), administration (21.2%), transcription (5.7%) and dispensation (2%). The MEs due to incorrect use were seen to predominate (23%), followed by incorrect dose (21.1%), inadequate duration (19.2%), incorrect administration rate (13.5%), drug omission (9.6%), incorrect administration technique (5.8%), incorrect pharmaceutical form (3.8%) and incorrect timing of administration (1.9%).
In 2010, the results of a French multicenter study, the Selected Medical Errors in the Intensive Care Unit (IATROREF) trial, were published,19 involving the participation of 70 DICMs. This was a prospective observational cohort study with a duration of one week, using the Delphi method, and established a list of 14 indicators associated with incidents related to medication (anticoagulants, vasoactive drugs, insulin), airway and mechanical ventilation (MV), central venous catheters, falls and delayed surgery. The incident rate was 2.1 per 1000 patients-day. The most frequent error corresponded to insulin administration (185.9 per 1000 days of insulin treatment). In turn, 183 errors (15.4%) were AEs, affecting 128 patients (9.3%). In addition to contributing to knowledge of the epidemiology of AEs in the critical care setting, this study established 14 indicators that can be used to monitor patient safety in our Units.
The Safety Climate Reduces Medication and Dislodgement Errors in Routine Intensive Care Practice trial was published in 2013,8 with the participation of 57 DICMs in Austria, Germany and Switzerland. This was a prospective observational study with a follow-up period of 48hours that used a voluntary reporting system to evaluate the incidence of MEs and the accidental removal of tubes, catheters and drains, as well as their relation to the safety climate and workload of the nursing staff. A total of 33.8% of the patients experienced one incident, with a rate of 49.8 errors per 100 days-patient. The occurrence of at least one medical error was greater with higher scores on the Nine Equivalents of Nursing Manpower Use Score (odds ratio [OR] 1.04, 95% CI: 1.02–1.05; p<0.01) and with the presence of a greater number of tubes, catheters and drains (OR 1.02, 95% CI: 1.01–1.03; p<0.01), In contrast, there were fewer errors when the safety culture of the Unit was greater (OR per standard deviation 0.67, 95% CI: 0.51–0.89; p<0.01).
Another retrospective cohort study analyzed 18 types of incidents based on the 10th Edition of the International Classification of Diseases (ICD-10) diagnostic codes associated with suboptimal quality of care.20 Thirty DICMs participated in the study, with 49,447 patients admitted from May 2014 to April 2017. The study aimed to estimate the frequency and types of AEs, identify the patient factors associated with such events, and establish their consequences. One or more AEs were detected in 12,549 admissions (25%) – the most common being respiratory complications (10%) and nosocomial infections (9%). The AEs in turn were associated with the presence of two or more comorbidities (OR=1.4, 95% CI=1.3–1.4), admission to the DICM from the operating room or other hospital ward (OR=1.8, 95% CI=1.7–2.0; OR=2.7, 95% CI=2.5–3.0), and readmission to the DICM during hospital stay (OR=4.8, 95% CI=4.7–5.6). The patients with AEs stayed 5.4 days longer in the DICM (95% CI=5.2–5.6 d, p<0.001) and 18.2 days longer in hospital (95% CI=17.7–18.8 d, p<0.001), and had a greater probability of in-hospital death (OR=1.5, 95% CI=1.4–1.6), compared with the patients without AEs.
A retrospective study carried out in four Italian DICMs on the rates and types of critical incidents compiled all the incidents reported through a database from 2013 to 2017.21 A total of 160 critical incidents were identified, with a rate of 1.7 per 100 patient admissions and 2.86 per 1000 days of patients in the DICM. The most frequent critical incidents were related to medication (n=35, 21.9%) (particularly during administration), followed by resources and organization, and inadequate nursing training (94.2%).
The available literature contains specific studies on the impact of AEs on patient mortality and stay in the DICM. In this regard, a retrospective cohort study involving multivariate survival analysis found AEs to be associated with the time to patient death and to hospital discharge.22 A total of 207 critically ill patients were evaluated (81% required MV, the median Glasgow Coma score was 8, and the median predicted mortality rate was 31%). At the hospital level, the recorded mortality rate was 25% (95% CI: 19–31) and the duration of stay was 15 days (interquartile range [IQR] 8–34 days). The AEs occurring in the DICM and the avoidable events were not significantly associated with the time to in-hospital death (hazard ratio [HR]=0.93; 95% CI: 0.44–1.98 and HR=0.72; 95% CI: 0.25–2.04), but were associated to hospital stay HR=0.50; 95% CI: 0.31–0.81 and HR=0.46; 95% CI: 0.23–0.91), with a mean increase in duration of stay of 31 days.
In another study, a systematic review and meta-analysis were carried out to examine the impact of AEs on mortality and the duration of stay in hospital and in the DICM.23 The potentially eligible studies were identified from four main databases. Out of 902 selected studies, 12 met the inclusion criteria. The patients with one or more medical errors and AEs (versus no medical errors or AEs) presented a nonsignificant increase in mortality (OR=1.5; 95% CI=0.98–2.14), but had significantly longer stays in hospital and the DICM. The difference of means (95% CI) was 8.9 days (3.3–14.7) in the case of hospital stay and 6.8 days (0.2–13.4) in the case of DICM stay.
Cantor et al. carried out a logistic regression analysis to determine the association between AEs and patient mortality.24 The AEs were classified based on the ICD-10, and the study population consisted of 17,173 patients admitted to the DICM between 2011 and 2016. The patients who experienced an AE had longer hospital and DICM stays, required more invasive interventions, and suffered greater in-hospital mortality than the patients who experienced no AEs.
Aikawa et al. in turn carried out a retrospective observational study based on the review of clinical histories using the Global Trigger Tool.25 Of the 246 patients admitted, 126 (51%) experienced one or more AEs, with an incidence of 201 per 1000 patients-day and 115 per 100 admissions. The presence of AEs was associated with the duration of DICM stay (β=2.85, 95% CI: 1.09–4.61).
National studiesThe Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]), endorsed by the Quality Agency of the Ministry of Health, carried out the first study in Spain on Safety and Risk in the Critical Patient (Seguridad y Riesgo en el Enfermo Crítico, SYREC).26 This was a prospective, multicenter observational cohort study with a follow-up period of 24hours. The study aimed to establish the incidence of no-harm incidents (NHIs) and AEs through voluntary and anonymous reporting by the DICM staff members. A total of 79 DICMs participated, with the inclusion of 1017 patients, of which 591 (58.1%) presented one or more incidents. Sixty-six percent of the incidents were NHIs and 34% were AEs. The incident rate was 5.89 per 100 patients per hour of stay in the DICM, and that of the NHIs and AEs was 3.47 and 2.04, respectively. The individual risk of suffering at least one AE was 62%, one NHI 45% and one AE 29%. Ninety percent of the NHIs and 60% of the AEs were considered to be avoidable or possibly avoidable. The AE resulted in patient death in 9 cases, representing a rate of 4.38 per 10,000 patients-hour of follow-up. For the 1017 admitted patients, the risk was 8.8 per 1000 admitted patients. Of the 9 recorded deaths, two were considered to have been avoidable.
The most frequent incidents were related to medication (24%), equipment (15%), nursing care (14%), the accidental removal of tubes, vascular accesses and drains (10%), the airway and MV (10%). The incidents related to medication, the airway and MV, vascular accesses, tubes and drains, equipment and diagnostic tests were mainly NHI (p<0.05). In contrast, those related to diagnostic error, care, procedures and surgery were mainly AEs (p<0.05). By definition, nosocomial infections are AEs.
Another study was published, based on the results of the SYREC trial, seeking to determine the incidence of MEs, their severity and avoidability.27 Of the total incidents reported in the SYREC trial, 350 were MEs (25%), representing an ME rate of 1.13 per 100 patients-day of stay. Most of these errors occurred in the prescription (34%) and administration phase (28%); 16% caused harm to the patient, and 82% were considered to be clearly avoidable.
Likewise, from the SEMICYUC, a study on Incidents in Mechanical Ventilation and the Airway (IVeMVA) has been carried out.28 It aimed to evaluate the incidence and characteristics of the safety incidents related to the management of the patient airway and MV in Spanish DICMs. This was a prospective, cross-sectional observational study with a duration of 7 days in which the incidents were reported on a voluntary and anonymous basis using a structured questionnaire. It analyzed the type of incidents, their characteristics, severity, avoidability and contributing factors. A total of 104 DICMs participated in the study, with the inclusion of 1267 patients, of which 745 (59%) suffered one or more incidents. Of the 2492 reported incidents, 59% were NHIs and 41% AEs. The individual risk of suffering at least one incident was 66.6%, and the incidence ratio of the incidents was 2 per 100 hours-patient. A total of 73.7% were related to MV, 9.5% to tracheotomy, 6.2% to noninvasive MV (NIMV), 5.4% to weaning/extubation, 4.4% to intubation, and 0.8% to prone decubitus. There was temporary patient damage in 12% of the incidents, while 0.8% were associated with a permanent injury, a threat to life or contributed to patient death; a full 73.5% were considered to be avoidable.
In the aforementioned studies, AEs were among the most common incidents in the critically ill. Concern about preventing them led to the signing of the collaboration agreement between the SEMICYUC and the Spanish Society of Hospital Pharmacy (Sociedad Española de Farmacia Hospitalaria [SEFH]), which contemplated different initiatives29 such as adapting the Self-Evaluation Questionnaire of the Hospital Drug Use Safety System to the DICM, know the degree of implementation of safe practices with drugs in the DICM, and identify possible opportunities for improvement.30
At the Spanish national level, two registries allow us to detect safety problems in the care of critically ill patients, improve the quality of such care, and generate knowledge in two areas: nosocomial infections, as assessed by the ENVIN study,31 and the management of acute coronary syndrome (ACS), as evaluated in the ARIAM registry.32
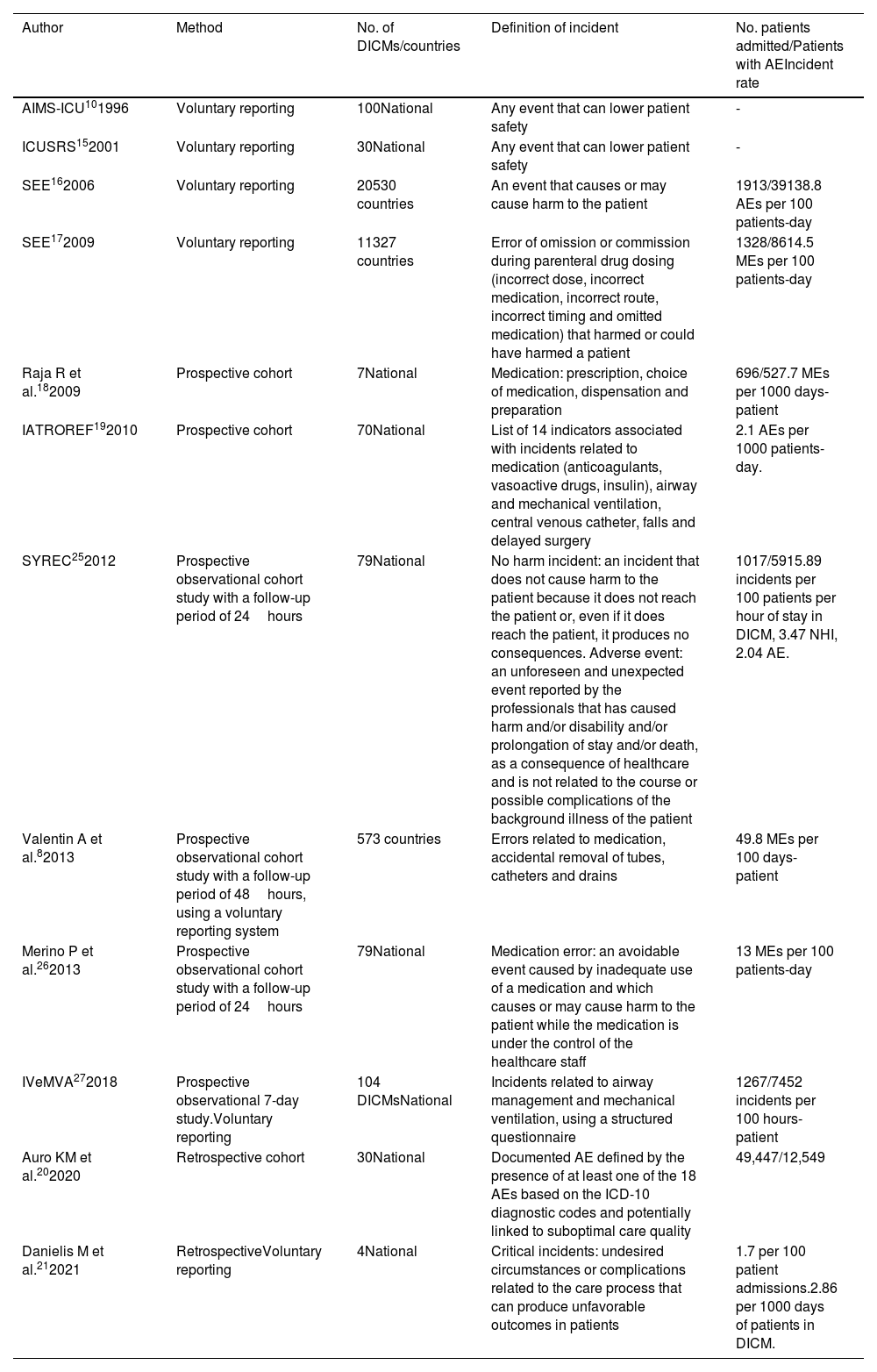
Different reasons may be postulated to explain the differences found in the published results. In this respect, the lack of a common terminology and taxonomy means that the definition of an AE varies from one study to another.33 The methods used for data collection and the type of events analyzed also condition the evaluation of safety incidents.34 Lastly, the different diseases and severities of the patients studied, as well as the number of participating DICMs, their different forms of organization, the availability of resources and safety culture further complicate the comparison of the published studies. Furthermore, in the case of MEs, addition is made of the pharmacotherapeutic groups analyzed, the process being evaluated, and the inclusion or exclusion of the different administration routes. Table 1 compares the different characteristics of the mentioned studies. Despite the differences found, most authors agree that safety incidents in the critically ill are frequent and are largely avoidable.
Main published studies on safety incidents in critically ill patients. Authors, methodology used, number of participating Departments of Intensive Care Medicine (DICMs) and countries, definition of incident, number of patients admitted, patients with an adverse event (AE) and AE incidence rate.
| Author | Method | No. of DICMs/countries | Definition of incident | No. patients admitted/Patients with AEIncident rate |
|---|---|---|---|---|
| AIMS-ICU101996 | Voluntary reporting | 100National | Any event that can lower patient safety | - |
| ICUSRS152001 | Voluntary reporting | 30National | Any event that can lower patient safety | - |
| SEE162006 | Voluntary reporting | 20530 countries | An event that causes or may cause harm to the patient | 1913/39138.8 AEs per 100 patients-day |
| SEE172009 | Voluntary reporting | 11327 countries | Error of omission or commission during parenteral drug dosing (incorrect dose, incorrect medication, incorrect route, incorrect timing and omitted medication) that harmed or could have harmed a patient | 1328/8614.5 MEs per 100 patients-day |
| Raja R et al.182009 | Prospective cohort | 7National | Medication: prescription, choice of medication, dispensation and preparation | 696/527.7 MEs per 1000 days-patient |
| IATROREF192010 | Prospective cohort | 70National | List of 14 indicators associated with incidents related to medication (anticoagulants, vasoactive drugs, insulin), airway and mechanical ventilation, central venous catheter, falls and delayed surgery | 2.1 AEs per 1000 patients-day. |
| SYREC252012 | Prospective observational cohort study with a follow-up period of 24hours | 79National | No harm incident: an incident that does not cause harm to the patient because it does not reach the patient or, even if it does reach the patient, it produces no consequences. Adverse event: an unforeseen and unexpected event reported by the professionals that has caused harm and/or disability and/or prolongation of stay and/or death, as a consequence of healthcare and is not related to the course or possible complications of the background illness of the patient | 1017/5915.89 incidents per 100 patients per hour of stay in DICM, 3.47 NHI, 2.04 AE. |
| Valentin A et al.82013 | Prospective observational cohort study with a follow-up period of 48hours, using a voluntary reporting system | 573 countries | Errors related to medication, accidental removal of tubes, catheters and drains | 49.8 MEs per 100 days-patient |
| Merino P et al.262013 | Prospective observational cohort study with a follow-up period of 24hours | 79National | Medication error: an avoidable event caused by inadequate use of a medication and which causes or may cause harm to the patient while the medication is under the control of the healthcare staff | 13 MEs per 100 patients-day |
| IVeMVA272018 | Prospective observational 7-day study.Voluntary reporting | 104 DICMsNational | Incidents related to airway management and mechanical ventilation, using a structured questionnaire | 1267/7452 incidents per 100 hours-patient |
| Auro KM et al.202020 | Retrospective cohort | 30National | Documented AE defined by the presence of at least one of the 18 AEs based on the ICD-10 diagnostic codes and potentially linked to suboptimal care quality | 49,447/12,549 |
| Danielis M et al.212021 | RetrospectiveVoluntary reporting | 4National | Critical incidents: undesired circumstances or complications related to the care process that can produce unfavorable outcomes in patients | 1.7 per 100 patient admissions.2.86 per 1000 days of patients in DICM. |
In addition to the mentioned harm to the patient, AEs have other undesirable consequences. Few authors have investigated the associated economic costs. Kaushal et al.,35 in a case-control study, evaluated the cost increments associated with AEs in two DICMs. During one year, in 13 established periods of two and three weeks, a comparison was made of 108 cases with AEs and 375 controls. A total of 159 AEs were identified, of which 44% were avoidable, with un total cost of 1,480,000 $.
Another prospective observational study estimated a cost attributable to a medical error of 800,000 € annually, equivalent to 800 € per treated patient.36
Leape et al.37 found that reducing MEs through the incorporation of a pharmacist to the team in a 17-bed Unit resulted in a cost saving of 270,000 $ a year.
Cantor et al.24 found that the mean total hospital costs and the specific costs of the DICM were greater among those patients who experienced an AE (72,718 $; 46,715 $) than in those with no AE (20,543 $; 16,217 $). After controlling for patient age, sex, comorbidities and the severity of disease, AEs were seen to be associated with an increase in mean total costs (cost ratio=1.04, 95% CI: 1.06–1.08). The types of events with the greatest cost impact were nosocomial infections and those related to heart disease.
In addition to the mentioned negative consequences, it must be remembered that AEs also have serious repercussions for patient families and healthcare professionals, erode patient confidence in the healthcare system, and are an important cause of lawsuits.38–40
ConclusionsIt can be concluded that AEs are frequent in critically ill patients, and are avoidable in a large percentage of cases. Medication errors, mainly those occurring in the prescription and administration phases, are among the most frequent problems.
All AEs imply an economical cost, in the same way as their prevention or elimination – though to a lesser degree. We have to work with budget limitations, but when dealing with actions that are clearly effective in preventing AEs, if the decision is made in terms of efficiency and the opportunity costs of the different options, the associated cost increment should be seen as an investment.
It is mandatory to adopt policies that offer global support and cover the needs of the different collectivities involved in an AE.
We must control the great impact of AEs on health and economic outcomes in the critical care setting, adopting healthcare risk management policies based on systematic and structured methods. An example is the UNE 179003 standard as Patient Safety Risk Management System - a Spanish-specific healthcare standard developed by the Spanish Association for Standardization and Certification (Asociación Española de Normalización y Certificación [AENOR]).41 The certification of a healthcare organization by this system, which is warranted by independent entities, indicates that it complies with a series of rules and standard operating procedures intended to reduce the incidence of AEs.42 In addition, it makes continuous improvement necessary, since audits are carried out on an annual basis and must be passed.
Financial supportNone.
Conflicts of interestThe author declares that she has no conflicts of interest.
Please cite this article as: Merino P. Epidemiología de los eventos adversos en los servicios de medicina intensive. Med Intensiva. 2024. https://doi.org/10.1016/j.medin.2024.03.015.