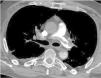
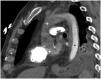
A 56-year-old man presented with profound shock and unresponsive hypoxemia. Pulmonary embolism was suspected given the extremely dilated right ventricle with septal flattening. It was decided then to start peripheral veno-arterial extracorporeal membrane oxygenation (VA-ECMO) through bedside cannulation. 72h later, the patient was on unfractionated heparin, had recovered from multiorgan failure without neurological impairment and vasopressors had been withdrawn. However, persistent hypoxemia and right ventricle dysfunction challenged ECMO weaning. A computed tomography confirmed the diagnosis (Fig. 1) and provided evidence of the harlequin syndrome (Fig. 2) as the two bloodstreams, the native cardiac output and oxygenated ECMO return, meet in the watershed area. Subsequently, the patient underwent a successful transcatheter pulmonary thromboaspiration (Fig. 3) and could be weaned from mechanical ventilation and ECMO the following days. He was discharged two weeks later without further complications.
Authors’ contributionConception, design and writing the article JMS and ISC. Analysis and image collection NAE.
Conflict of interestNone.
Funding sourceNone.