To evaluate whether the size of acute myocardial infarction (AMI) shows circadian variability.
DesignAn observational, prospective study.
SettingA 12-bed coronary care unit.
PatientsConsecutive patients diagnosed with ST-elevation myocardial infarction (STEMI) undergoing primary percutaneous coronary intervention.
InterventionsThe patients were divided into two groups according to the time of onset of AMI symptoms (group A: 0–12h, group B: 12–24h).
Main variables of interestAge, sex, cardiovascular risk factors, coronary anatomy, left ventricular ejection fraction, infarct location, time from onset of symptoms to reperfusion, presence of heart failure upon admission, and peak troponin I value.
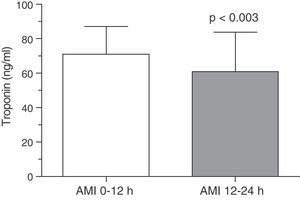
ResultsA total of 108 patients with a diagnosis of STEMI were included. Patients in group A showed a higher troponin I concentration compared to group B (troponin I: 70.85±16.38ng/ml vs 60.90±22.92ng/ml, p=0.003). In the multivariate analysis the onset of AMI between 0 and 12h was identified as an independent predictor of infarct size (OR: 1.133, 95%CI 1.012–1.267, p=0.01).
ConclusionsAn onset of AMI between 0 and 12h results in a significantly larger final size of necrosis compared with any other time of presentation.
Evaluar si el tamaño del infarto agudo de miocardio (IAM) presenta variabilidad circadiana.
DiseñoEstudio prospectivo observacional.
ÁmbitoUnidad coronaria de 12 camas.
PacientesEnfermos consecutivos con diagnóstico de IAM con elevación del segmento ST sometidos a intervención coronaria percutánea primaria.
IntervencionesSe dividió a los pacientes en 2 grupos, dependiendo del horario de inicio de los síntomas del IAM (grupo A: 0-12 h; grupo B: 12-24 h).
Variables de interés principalesEdad, sexo, factores de riesgo cardiovascular, anatomía coronaria, fracción de eyección del ventrículo izquierdo, localización del infarto, tiempo de inicio de los síntomas y reperfusión, presencia de insuficiencia cardiaca al ingreso, pico de troponina I.
ResultadosSe incluyeron un total de 108 pacientes con diagnóstico de IAM con elevación del segmento ST. Los pacientes del grupo A presentaron concentración de troponina I mayor con respecto al grupo B (70.85±16.38 frente a 60.90±22.92 ng/ml, p=0.003). En el análisis multivariado el inicio del IAM entre las 0-12 h se mostró como un predictor independiente del tamaño del infarto (OR: 1.133, IC del 95% 1.012-1.267; p=0.01).
ConclusionesEl inicio del IAM entre las 0-12 h resulta en un tamaño necrótico final significativamente mayor que cuando se inicia en cualquier otro momento del día.
The circadian rhythm is the biological clock that regulates most of the mechanisms in our body. In recent years, different clinical studies have shown acute myocardial infarction (AMI) to be more frequent in the first hours of the morning.1 No single underlying physiopathological mechanism is involved in this phenomenon; rather, a number of contributing factors have been identified: increased blood pressure and heart rate, increased vasomotor tone, increased platelet aggregability accompanied by diminished fibrinolytic activity, and variations in circulating hormone levels.2 The present study was designed to determine whether AMI size also shows circadian variability.
Patients and methodsA prospective study was made of the patients admitted to the Coronary Unit of a third-level hospital, diagnosed with AMI with ST-segment elevation and subjected to primary angioplasty. AMI was diagnosed based on the criteria published in the medical literature,3 and all patients were revascularized according to the established time periods. The patients were divided into two groups according to the time of onset of AMI (group A: 0:00–12:00h; group B: 12:00–24:00h). Clinical, angiographic and laboratory test variables were analyzed.
AMI size was quantified based on the peak troponin I concentration. The blood samples for this evaluation were collected every 8h on the first day, and every 24h over the next three days, in accordance with the hospital protocol. Troponin I was determined by means of immunoenzymatic techniques using an ELISA test. The within- and between-test coefficients of variability were 2.2% and 5.9%, respectively. The limit of detection was established as 0.12ng/ml.
The study was approved by the Clinical Research Ethics Committee of the hospital, and all patients gave informed consent to participation in the trial.
The results were analyzed using the SPSS version 15.0 statistical package (SPSS Inc., Chicago, IL, USA). Qualitative variables were expressed as percentages, while quantitative variables were presented as the mean ±standard deviation (SD). The Kolmogorov–Smirnov test was used to assess normal distribution of the study variables. The chi-squared test was used for the comparison of two qualitative variables. The differences in means between two quantitative variables exhibiting a normal distribution were analyzed with the Student t-test for non-paired samples. Multivariate analysis was carried out using a binary logistic regression model to demonstrate whether infarction onset is an independent predictor of infarct size. The model included variables such as cardiovascular risk factors, age, sex, anterior location of the infarct, multivessel coronary arterial disease, left ventricle ejection fraction, time of start of the symptoms and troponin I levels. Statistical significance was considered for p<0.05.
ResultsA total of 108 patients diagnosed with AMI with ST-segment elevation were included in the study. The subjects in group A presented a higher troponin I concentration than those in group B (70.85±16.38ng/ml vs 60.90±22.92ng/ml, p=0.003) (Fig. 1). The rest of the clinical variables, including ischemia time, infarct location, age, sex, cardiovascular risk factors and hemodynamic variables showed no statistically significant differences (Table 1). In the multivariate analysis, a time of onset of AMI between 0:00 and 12:00h was found to be an independent predictor of infarct size (OR: 1.133, 95%CI 1.012–1.267; p=0.01).
Demographic, laboratory test and hemodynamic data of the study population.
| Group A (AMI 0:00–12:00h) (n=21) | Group B (AMI 12:00–24:00h) (n=87) | p-value | |
| Age (years) | 60±12 | 65±11 | 0.09 |
| Sex (males), n (%) | 18 (86) | 67 (77) | 0.38 |
| Arterial hypertension, n (%) | 12 (57) | 45 (52) | 0.40 |
| Diabetes mellitus, n (%) | 10 (48) | 25 (29) | 0.09 |
| Hypercholesterolemia, n (%) | 7 (33) | 46 (53) | 0.10 |
| Smoker, n (%) | 9 (43) | 35 (40) | 0.82 |
| CD, n (%) | 11 (52) | 38 (44) | 0.92 |
| LVEF | 56±10 | 56±12 | 0.86 |
| Anterior AMI, n (%) | 10 (48) | 39 (45) | 0.81 |
| Killip class > I, n (%) | 3 (14) | 8 (9) | 0.65 |
| Pain-reperfusion time (min) | 244±67 | 240±70 | 0.80 |
| Final post-PTCA TIMI flow | 0.72 | ||
| 0–1 | 1 (5) | 4 (5) | |
| 2 | 3 (14) | 15 (17) | |
| 3 | 17 (81) | 68 (78) | |
| Creatinine, mg/dl | 0.95±0.21 | 1.10±0.34 | 0.67 |
| Total cholesterol, mg/dl | 182±40 | 185±51 | 0.81 |
Values expressed as n (%) or mean±standard deviation.
PCTA: percutaneous transluminal coronary angioplasty; CD: coronary arterial disease; LVEF: left ventricle ejection fraction; AMI: acute myocardial infarction; TIMI: thrombolysis in myocardial infarction.
Circadian rhythms are known to influence many cardiovascular physiopathological processes. Studies in rodents have shown that infarct size can be influenced by the time of day.4 In humans, the fact that AMI is more frequent in the first hours of the morning was demonstrated by Muller et al.5 over two decades ago. Changes in the physiological cycles of the body take place during this time period, including increased blood pressure and platelet aggregability, and variations in hormone secretion. The first morning hour accentuation of these processes, when acting upon a vulnerable target organ, can help explain the increased incidence of AMI in the first hours of the morning.
The present study recorded a significant association between the time of day of AMI and the size of myocardial necrosis. Specifically, the onset of infarction between 0:00 and 12:00h results in a significantly larger infarct size than when AMI occurs at any other time of the day. It is important to note that these findings are independent of other variables that might act as confounding factors, particularly those independent of the time of onset of AMI. Likewise, circadian variations have been shown to influence the success of primary angioplasty.6–8 In our study, the results were not influenced by the primary angioplasty procedure used, since there were no differences in the final post-angioplasty TIMI flow between the two groups. The results obtained are of considerable clinical relevance, since the long-term prognosis of AMI patients is conditioned by the size of the infarct, the final ejection fraction, and left ventricular remodeling, which often leads to heart failure.9 Therefore, the onset of AMI symptoms between 0:00 and 12:00h should be regarded as a potential additional risk factor and an indicator of a poorer patient prognosis.
These observations are similar to those recently published by Suárez-Barrientos et al.,10 who retrospectively analyzed infarct size in 811 patients in relation to the time of AMI. The authors concluded that the time of day exerts an important influence upon the presentation of AMI and its size-the latter being greater when infarction occurs in the hours of transition from night to day. The study of these mechanisms has generated considerable interest in recent years due to their clinical relevance. In effect, they may prove crucial for understanding certain studies on myocardial protection, and a number of mechanisms mediated by certain hormones-some of which exhibit a circadian secretory pattern-could constitute a spontaneous form of cardiac protection. In this sense, melatonin is a hormone that plays a key role in the human body. This methoxyindolamine is mainly produced by the pineal gland, with a circadian secretion profile, and has a range of functions—though its circadian secretion mainly regulates physiological and neuroendocrine processes.11 Clinical studies in humans and experimental research in animals have demonstrated a relationship between serum melatonin levels and coronary arterial disease.12
Several years ago, we showed that AMI patients have lower nocturnal melatonin concentrations than the controls.13 We therefore postulate that AMI occurring between 0:00 and 12:00h involves a larger infarct size due at least in part to the presence of lower serum melatonin levels, and therefore to lesser antioxidant and ischemia–reperfusion damage protective action.14 In this context, we consider that further studies of these cardioprotective mechanisms are needed, as they may have future diagnostic, protective and therapeutic implications for patients with AMI.
Our study has a number of limitations, such as the small sample size and the indirect calculation of infarct size based on the elevation of myocardial necrosis markers. Although this measurement approach has been extensively validated, the current technique of choice is cardiac MRI.15 The high cost and limited availability of this technique has not allowed us to include it in our study protocol, however.
In conclusion, this prospective study shows the time of day to exert an important influence upon the presentation of AMI and on infarct size – the latter being larger when infarction occurs between 0:00 and 12:00h in the morning.
Conflict of interestThe authors declare no conflicts of interest.
Please cite this article as: Arroyo Úcar E, et al. Influencia de la variabilidad diurna en el tamaño del infarto agudo de miocardio. Med Intensiva. 2012;36:11–4.