Various modifications of the Macintosh blade and direct laryngoscopy have been incorporated into practice to improve the intubation success rate and avoid complications while ensuring patient safety. This study evaluates the usefulness of two different direct laryngoscopy methods used by operators with various level of experience in the Intensive Care Unit.
Material and methodsIn a single centre prospective study, C-MAC and Macintosh laryngoscopes were compared in terms of laryngoscopy and intubation outcomes such as glottic visualization, number of intubation attempts, intubation success and satisfaction score.
ResultsDuring the one-year study period, 263 patients were evaluated and data of 218 patients were analyzed. The rate of successful first attempt intubation was higher in the video laryngoscope group (VL) (84% vs 57%; P<0.001). A significantly greater number of patients in the Macintosh laryngoscopy group had difficult visualization of the glottis in terms of the modified Cormack and Lehane classification and Percentage of Glottic Opening scale.
ConclusionThe use of video laryngoscope for intubation in ICU settings results in better visualization of the glottis and a higher incidence of successful intubation attempts.
En la práctica clínica se han incorporado diversas modificaciones a la hoja de Macintosh y del laringoscopio directo para mejorar la tasa de éxito de la intubación y evitar complicaciones, a la vez que se garantiza la seguridad del paciente. En este estudio evaluamos la utilidad de los 2 métodos de laringoscopia directa empleados por profesionales sanitarios con distintos grados de experiencia en la unidad de cuidados intensivos.
Materiales y métodosEn un estudio prospectivo y unicéntrico se compararon los laringoscopios de Macintosh y C-MAC en términos de deselances de la largingoscopia y la intubación, como la visualización de la glotis, el número de intentos de intubación, el éxito de la intubación y la puntuación de la satisfacción.
ResultadosDurante el periodo del estudio de un año se evaluaron 263 pacientes y se analizaron los datos de 218 pacientes. La tasa de intubación con éxito al primer intento fue más elevada en el grupo de videolaringoscopio (84% frente al 57%, p<0,001). Un número significativamente más alto de pacientes del grupo del laringoscopio de Macintosh presentó dificultades de visualización de la glotis de acuerdo con la clasificación modificada de Cormack y Lehane, y según la escala de porcentaje de apertura de la glotis.
ConclusiónEl uso del videolaringoscopio para la intubación en el entorno de la unidad de cuidados intensivos se asocia con una mejor visualización de la glotis y una tasa más alta de intentos de intubación exitosos.
Intubation and mechanical ventilation are essential and sometime urgent in various life threatening conditions in the Intensive Care Unit (ICU). Laryngoscopy and intubation are highly challenging and not free from complications such as hypoxia, bradycardia, hypotension, damage to upper airways, aspiration and cardiac arrest.1 Various attempts have been made to improve success rate and minimize complications, which include use of neuromuscular blockade, care bundles, training on simulators.2
In the last decade, many airway equipments including various types of video laryngoscope (VL) were being developed and compared with the conventional Macintosh laryngoscopy (ML). Better visualization of glottic opening may result in the easy and quick endotracheal intubation while reducing complication rates. Recent systematic review found evidence supporting decreased incidences of intubation failure in the context of difficult airway in operation theatre by using video laryngoscopy. There are positive and negative reports regarding the benefits of video laryngoscopy over direct laryngoscopy in critically ill patients in an ICU.1–3 From Indian subcontinent, no studies have been reported about the comparison between VL and ML in ICU settings. This study was conducted to test the hypothesis that C-MAC video laryngoscope increases the success rate of first pass orotracheal intubation in intensive care setting as compared to Macintosh laryngoscope.
Materials and methodsThis prospective, randomized, comparative study was conducted in a 32-bed multidisciplinary adult ICU of a tertiary-care teaching hospital. Following approval from Institute Ethics Committee, the study was conducted over a period of eighteen months (from 1st January 2017 till 30th June 2018). Informed consents were obtained from patients or their legal representatives and data relevant to intubation were collected in a prescribed format.
All ICU patients who needed elective endotracheal intubation were included in the study except patients of age less than 18 years, pregnant and lactating women, patients with facial trauma including burn injury, suspected or confirmed cervical spine injury, lack of time for randomization and inclusion due to ongoing resuscitative efforts, unable to obtain informed consent. Following inclusion into the study, sequential sealed opaque envelope technique was used for allocation of laryngoscopy method, either Macintosh Laryngoscope (ML group), blade size 3 or 4 or Karl Storz C-MAC video laryngoscope (VL group), Macintosh shaped blades size 3 or 4 (Karl Storz GmbH & Co, KG, Tuttlingen, Germany). C-MAC VL blade is a Macintosh type with a small camera and light source at the distal one third of the blade. The removable electronic module, interface between front-end of VL and the portable monitor unit, fits into the receptacle of laryngoscope and after intubation they can be separated for the preparation of the laryngoscope for the next intubation.
All anaesthesiologists working in this ICU were being oriented to video laryngoscopy (using C-MAC VL) on manikin at the time of joining in the department. Intubating anaesthesiologists (laryngoscopist) had experience of minimum fifty videolaryngoscopies using C-MAC VL. Laryngoscopists were categorized (based on exposure) into junior (up to three years), senior (more than 3–8 years) and consultant (more than 8 years) based on their years of anaesthesia experience. All intubations were performed in the presence of two laryngoscopists, one of them being either senior or consultant anaesthesiologist.
Preoxygenation was done for at least 3min by using either bag valve mask with oxygen flow of 15l per minute or noninvasive ventilation using 100% fraction of inspired oxygen. The medications for induction were intravenous (IV) fentanyl (1–2μg/kg) in every patient, with either propofol (1.5–2.0mg/kg) IV or thiopentone (3–5mg/kg) IV. Neuromuscular blockade was obtained by using succinylcholine (1–1.5mg/kg) IV (except patients with hyperkalemia, burn injury older than 24h) or Rocuronium (0.9mg/kg) IV. Laryngoscopies were performed using the method as per random allocation, after three failed attempts of intubations alternative techniques were used and subsequently they were not included in the analysis. Stylet was used as when required and external laryngeal manipulations were performed as per laryngoscopist's instruction. Alternative techniques such as gum elastic bougie, laryngeal mask airway (LMA), intubating LMA, intubation endoscope, cricothyrotomy set were used based on the in-house difficult airway algorithm. An intubation attempt was defined as introduction of laryngoscope and its subsequent removal with or without endotracheal tube (ETT) placement. Correct placement of ETT in first attempt by an individual laryngoscopist was defined as first-pass successful intubation. Successful placement of ETT was confirmed by both auscultation and mainstream capnography (normal appearing waveform over four or more breathing cycles).
The laryngoscopist documented the laryngoscopic view by using the modified Cormack & Lehane (C&L) classification and Percentage of Glottic Opening scale (POGO) and other intubation characteristics such as the indication for the intubation, number of intubation attempts, intubation success, and ease of intubation in relation to the video laryngoscopic view and satisfaction scores.4,5
Macintosh laryngoscopy (ML) has up to 69% success rate during first-pass orotracheal intubation, where as the success rate is 79% patients if video laryngoscope (VL) is used.1,3,6,7 Assuming 80% success rate of first-pass orotracheal intubation during VL, with type I error set at 5% and type II error set at 20%, 104 patients were needed in each group (i.e. 208 patients in total), to detect a difference of 18.5% in success rate.
Baseline and demographic data were expressed as the mean±standard deviation for Gaussian variables. The comparison of the two proportions was performed with the use of the chi-square test or Fischer's exact test when appropriate. The comparisons of means and medians were performed using Student's t test and Mann–Whitney test, respectively. The differences were considered statistically significant if P<0.05. Data were analyzed using MedCalc software (version 16.0, Ostend, Belgium).
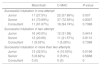
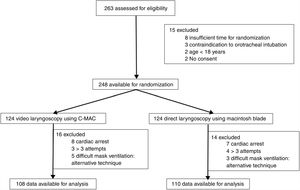
ResultsA total of 263 patients were evaluated, 248 patients were randomized into two groups (VL – videolaryngoscopy and ML – Macintosh laryngoscopy) and data of 218 patients were available for the final analysis (Fig. 1). Both the groups were comparable in terms of their demographic variables (Table 1). Sequential Organ Failure Assessment II score and the indications for intubation were similar between the two groups (Table 1).
Baseline characteristics of study population.
| Macintosh laryngoscopy(n=110) | C-MAC video laryngoscopy(n=108) | P-value | |
|---|---|---|---|
| Age in years, mean (SD) | 45.8 (16.2) | 48.3 (16.8) | 0.26 |
| Gender (male/female) | 67/43 | 63/45 | 0.92 |
| Body mass index, mean (SD) | 24.8 (7.6) | 23.9 (6.8) | 0.36 |
| Sequential organ failure assessment score, mean (SD) | 9.1 (3.9) | 8.8 (4.2) | 0.58 |
| Stylet use | 41/110 (37.3) | 71/108 (65.7) | <0.0001 |
| Stylet use in first attempt | 12/63 (19.0) | 55/91 (60.4) | <0.0001 |
| Stylet use in second attempt | 21/27 (77.8) | 13/14 (92.8) | 0.23 |
| Stylet use after second attempt | 20/20 (100%) | 3/3 (100%) | – |
| Indication for intubation | |||
| Neurological failure | 56 (50.9%) | 58 (53.7%) | 0.68 |
| Respiratory failure | 38 (34.54%) | 34 (31.5%) | 0.63 |
| Circulatory failure | 4 (3.6%) | 5 (4.63%) | 0.70 |
| Others | 12 (10.9%) | 11 (10.18%) | 0.86 |
Successful first-pass intubation was significantly higher in VL group (84% vs 57%, P<0.001) (Table 2). Reciprocally, higher number of patients in ML group needed two or more than two attempts for successful intubation (P<0.05). The incidence of difficult intubation, at least two failed intubation attempts, was 18% and 3% in the ML and VL groups, respectively (Table 2). Stylet use (Table 1) was higher in VL group as compared to ML group during first (VL vs ML, 65.7% vs 37.3%, P<0.0001) and second attempt intubation (VL vs ML, 92.8% vs 77.8%, P=0.23).
Intubation characteristics (number, percentage).
| Macintosh | CMAC | P-value | |
|---|---|---|---|
| Cormack and Lehane grade | |||
| Grade 1 | 49 (44.54%) | 91 (84.25%) | <0.0001 |
| Grade 2 | 28 (25.45%) | 7 (6.48%) | 0.0003 |
| Grade 3 | 21 (19.09%) | 6 (5.55%) | 0.0047 |
| Grade 4 | 12 (10.90%) | 4 (3.70%) | 0.0752 |
| Percentage of glottic opening | 54±23 | 81±11 | <0.0001 |
| Successful first-pass intubation | |||
| Intention-to-treat analysis | 63/124 (50.8) | 91/124 (73.37) | 0.0003 |
| Per-protocol anaysis | 63/110 (57.27) | 91/108 (84.26) | <0.0001 |
| No. of intubation attempts | |||
| 1 | 63 (57.27%) | 91 (84.26%) | <0.0001 |
| 2 | 27 (24.54%) | 14 (12.96%) | 0.044 |
| >2 | 20 (18.18%) | 3 (2.78%) | 0.0005 |
| Laryngoscopist's satisfaction score | |||
| 0 | 3 (2.73%) | 1 (0.93%) | 0.63 |
| 1 | 3 (2.73%) | 3 (2.78%) | 0.69 |
| 2 | 5 (4.55%) | 6 (5.56%) | 0.97 |
| 3 | 21 (19.09%) | 14 (12.96%) | 0.29 |
| 4 | 68 (61.81%) | 84 (77.78%) | 0.015 |
Based on modified C&L classification, higher number of patient in ML group had difficult visualization of the glottis in comparison to VL group. The glottis could not be visualized in 33 (30%) and 10 (9%) patients (C&L grade 3 or 4), was only partially visualized in 28 (25%) and 7 (6%) patients (C&L grade 2) and was fully visualized in 49 (44%) and 91 (84%) patients (C&L grade 1) in ML and VL groups, respectively. POGO scale showed significant improvement in glottis view in VL group compared to ML group (81 vs 54, P<0.0001) (Table 1). Junior laryngoscopists could successfully intubate higher number of patients in VL group in first attempt (57.9% vs 27.5%, VL vs ML, P=0.007). Intubation success rates were similar in both the groups when experience of the anaesthesiologist was concerned, except in the subgroup as mentioned above (Table 3).
Comparison of intubation attempts (number, percentage).
| Macintosh | C-MAC | P-value | |
|---|---|---|---|
| Successful intubation in one attempt | |||
| Junior | 11 (27.5%) | 22 (57.89%) | 0.007 |
| Senior | 41 (70.69%) | 37 (72.55%) | 0.8307 |
| Consultant | 11 (91.67%) | 18 (94.74%) | 0.7388 |
| Successful intubation in two attempt | |||
| Junior | 16 (40.0%) | 12 (31.58) | 0.4414 |
| Senior | 12 (20.69) | 11 (21.57%) | 0.9110 |
| Consultant | 1 (8.33%) | 1 (5.26%) | 0.7388 |
| Successful intubation in more than two attempts | |||
| Junior | 13 (32.5%) | 4 (10.53%) | 0.0196 |
| Senior | 5 (8.62%) | 3 (5.9%) | 0.5888 |
| Consultant | 0 (0) | 0 (0) | 0 |
Endotracheal intubation in critically ill patients differs from intubation in the well controlled operation theatre environment in many ways such as: illness and instability of patients, limitations in terms of time spent preparation, patient positioning, equipments, medications, preoxygenation, operator experience, optimum glottic visualization. In the present study, use of the C-MAC® videolaryngoscope significantly improved percentage of glottis opening during airway management in the ICU. During video laryngoscopy, looking around the corner improves the optical access, but there can be difficulty in negotiating the tip of the tube into larynx with increased risk of contact with the anterior larynx wall. Increased usage of stylet in VL group during all attempts were the result of this phenomenon, which has been described earlier with the use of several video laryngoscopes.8
In patients with history of difficult laryngoscopy, C-MAC laryngoscopy had better glottis view in 94% of patients.9 Patients with predicted difficult airway had better optical access and more successful first attempt intubation during C-MAC laryngoscopy as compared to Macintosh laryngoscopy.10 There has been mixed result from various studies when VL was compared with ML in ICU setting. A recent multi-centre randomized controlled trial (RCT) (MACMAN trial) conducted seven ICUs in France found no improvement in the frequency of successful first-pass intubation by using VL compared to ML.2 The outcome difference between present study and MACMAN trial can be attributed to single centre vs multicenter, type of video laryngoscope, observer bias, laryngoscopist's background and skill level and experience with the VL. Various studies11–14 including two meta-analyses8,15 had reported increased first pass intubation success rate of VL over ML in non-ICU settings, but there were methodological flaws and heterogeneity. At the same time, evidences from other studies including two RCTs in ICU had shown no improvement in the success rate of video laryngoscope over direct one during first-pass intubation.9,10
A recent systematic review, which included intubations done in operation theatre, had reported reduced intubation failure, easier intubation in patients with known or predicted difficult airway and likely improvement of glottic view and reduction in number of laryngoscopy attempts. There was lack of evidence to support the ability of VL to reduce the time required for intubation and decrease incidences of hypoxia or respiratory complications.16 In this study, though VL group had significantly higher successful first-pass intubation, but in terms of overall successful intubation, both the groups were similar.
Intubation at locations other than operating room is commonly met with many difficulties. The incidence of difficult laryngoscopies reported for the operating room (5%) is significantly less frequent than in other settings.17 Various studies have stated that the occurrence of difficult intubations in critically ill patients ranges from 10 to 22%.18–20 In our study, the rate of difficult laryngoscopy (C&L grade 3 and 4) using ML was 30%. We attribute the involvement of anesthesiologists with different years of experience to the higher incidence of difficult airway in the current study. In earlier studies, VL had a better glottic visualization but not higher first-pass successful intubation and higher usage of stylet or gum elastic bougie.1–3 In the present study, we reported better glottic visualization, laryngoscopist's satisfaction, higher successful first-pass intubation and increased stylet usage in VL group as compared to ML group. Similar to the result of MACMAN trial,3 we had a significantly higher usage of stylet in the VL group as compared to ML group. Gum elastic bougie as compared to stylet improved the success rate during Macintosh laryngoscopy in cases with poor glottic visualization.21 At the same time, gum elastic bougie has been found to be as efficient as stylet during video laryngoscopy.22 Routine use of stylet during video laryngoscopy had not improved the rate of successful first-pass intubation and French guidelines recommends avoidance of stylet and use of gum elastic bougie in case of difficult orotracheal intubation.23
In terms of experience, juniors had a significantly higher successful first-pass intubation by using VL, but the difference was not significant in the hands of senior and consultant anaesthesiologists. In an earlier prospective study conducted in ICU, there were no significant differences in successful intubation attempt when experience was taken into account by using video and direct laryngoscopy.1 The finding from current study indicates that in the hand of less experienced laryngoscopists, video laryngoscope may increase the success rate of laryngoscopy and intubation in intensive care setup. But further studies are required to compare the time needed for intubation and rates of complication between the different laryngoscopies. Various factors that can confound include the study population, place of use, use and type of neuromuscular blockade, laryngoscopist characteristics, type of VL, difficult mask ventilation and intubation, involvement of independent trained data collector.
Limitations of our study were: (a) only Macintosh blade of C-MAC not the more curved D-blade was compared with direct laryngoscopy was used, (b) predictors of difficult laryngoscopy were not taken into account, (c) neuromuscular monitoring was not used to assess the adequacy of muscle relaxation, (d) time required for successful intubation and complications of intubation such as changes in oxygenation and haemodynamic parameters were not taken into account, (e) number of intubations performed by various laryngoscopists were not the same, juniors performed significantly higher number of laryngoscopies, and (f) use of subjective methods of assessment such as Cormack and Lehane grade, POGO score and laryngoscopist's satisfaction always introduce observer's bias. Future studies may plan alternative objective ways of assessment to minimize such bias.
ConclusionUse of VL not only improved glottis visualization, but also increased the rate of successful first-pass intubation and especially in less experienced hands in ICU. Despite equivocal support for video and direct laryngoscopy, further studies involving laryngoscopists of different expertise are required to evaluate usefulness various available video laryngoscopes as compared to Macintosh laryngoscope.
FundingNone to disclose.
Authors’ contributionSamarjit Dey, conception and design of the study, data acquisition.
Debasis Pradhan, conception and design, analysis and interpretation of data.
Priyam Saikia, analysis and interpretation of data, draft of the article, final approval.
Prithwis Bhattacharyya, conception and design, critical review of the intellectual content and final approval.
Hariom Khandelwal, data acquisition, draft of the article.
Adarsha KN, data acquisition, draft of the article.
Conflicts of interestNone.
This work would not have been possible without the help and commitments of all the nursing and medical staffs of Department of Anaesthesiology and Critical Care, NEIGRIHMS, Shillong, India.