Extracorporeal membrane oxygenation (ECMO) support is indicated in patients who are refractory to treatment, those with cardiogenic shock or respiratory failure and those with exacerbations eligible for heart and lung transplantation. Physician experience and quantity of necessary resources are reasons why regionalization could benefit patients of this kind, establishing ECMO reference centers and integrating a transportation network specialized in ECMO.
This type of transportation is a challenge for healthcare systems and physicians, given its greater complexity, requiring a multidisciplinary and inter-territorial approach. ECMO transportation is safer than without mechanical support, though there are currently no criteria for starting such therapy in patients being transferred. Criteria of lesser severity might be necessary for these patients. The training and specialization of the team in extracorporeal support therapies, interfacility transport and the systemization of transfer can improve the outcomes. There are no studies on the conditions that must be met by the transportation media, although space and stability are important characteristics. Air transfer with ECMO is an increasingly frequent option. Although there are data on its safety, there are none on the physiology of patients undergoing ECMO at high altitudes. Such information could be of help in the indication and management of this type of transportation.
El soporte extracorpóreo con membrana de oxigenación extracorpórea (ECMO) está indicado en pacientes resistentes al tratamiento, con shock cardiogénico o insuficiencia respiratoria y en aquellos pacientes reagudizados subsidiarios de trasplante cardiaco y pulmonar. La experiencia profesional y la cantidad de recursos necesarios son causas por las que se cree que la regionalización podría beneficiar a este tipo de pacientes a través del establecimiento de centros de referencia en ECMO y de la integración de una red de transporte especializado en ECMO. Debido a su mayor complejidad, este tipo de transporte supone un reto para los sistemas sanitarios y para los propios médicos, y requiere un abordaje multidisciplinar e interterritorial. El transporte en ECMO es más seguro que sin soporte mecánico, sin existir por el momento criterios de iniciación de la terapia en pacientes a trasladar, pudiendo ser necesarios criterios de menor gravedad en ellos. La formación y la especialización del equipo tanto en terapias de soporte extracorpóreo como en transporte interhospitalario, así como la sistematización de los traslados, pueden favorecer los resultados. No existen estudios acerca de las condiciones que deben cumplir los medios de transporte, siendo el espacio y la estabilidad características importantes. El traslado aéreo en ECMO supone una posibilidad cada vez más frecuente, existiendo datos sobre su seguridad, pero no sobre la fisiología del paciente en ECMO en altura, lo cual podría ayudar a la indicación y gestión de este tipo de transporte.
Regionalizing or centralizing certain processes has proven to reduce morbimortality in certain diseases such as polytrauma or in neonatal intensive care units.1–3 Today the benefit of these programs for the management of other diseases like cardiorespiratory patients,4 transplant-eligible patients or extracorporeal life support (ECLS) therapies5–10 is still under discussion. Regionalization requires establishing centers of reference and safe and sanitary transfers.2,11,12 We could say that as long as it is safe, the transfer of critically ill patients will reduce morbimortality since it facilitates the arrival to the receiving center.3 The way the team is organized is dictated by the needs of the patient, so the more complex the patients to be transferred are, the more specialized and trained the teams need to be.5 For the time being, we do not have enough data to confirm an increased survival with the use of specialized teams of transportation, except in the case of pediatric transfers.3,13
The technological improvements made and the growing experience in advanced life support techniques and ECLS increase the possibilities of treating cardiogenic shocks and severe acute respiratory distress syndromes (SARDS).14–22 The low incidence rate, high management complexity and great amount of resources needed require regionalization.5–9
The end of the 1990s saw the beginning of transfers of pediatric patients with respiratory failure but the mortality rates associated to these transfers were up to 39.1%.23 Back in 2006, the CESAR study brought back the interest for the use of the extracorporeal membrane oxygenation (ECMO) in patients with SARDS by showing promising survival rates in these patients, yet once again, a relative mortality rate was associated with the transfers without extracorporeal support.14 Studies conducted during the H1N1 pandemic showed that the transfer of patients with SARDS was safer with ECMO than without it and obtained similar results to those patients treated right from the beginning in the tertiary referral center.10,24,25
Similarly, the transfer of patients with refractory cardiogenic shock has been evolving. In 2013, Paris saw the birth of the Cardiac-RESCUE program and since there has been a wide consensus among the experts to recommend hemodynamic stabilizations with veno-arterial ECMO and then transfer to the tertiary referral center being the VA-ECMO the bridge to cardiac function recovery, implantation of ventricular assist devices (VAD), and/or heart trasplant.11,18–22
The widespread use of the therapy and the universalization of ECMO transportation systems are a reality even in the absence of studies that establish the standardized criteria for conducting mechanical supports and the conditions required to perform ECMO transfers. The creation of a network of air and ground ECMO transportation includes the regional study of hospital resources, the hospital infrastructures available and the creation of highly qualified professional teams.
ECMO programsThe low incidence of cases, the need for specialized training, the amount of material and equipment needed, the human resources required and the possible negative effect on morbimortality as a consequence of an insufficient volume and experience are some of the reasons that recommend centralizing and planning ECLS programs both for respiratory and cardiac patients.7–9,11
Tertiary referral centers promote continuous medical education (CME) and have a significant experience based on acceptable number of patients per year.9 The integration of different services is at the cornerstone of multidisciplinary approach, and the relation with non-tertiary referral centers and patients’ providers is at the very foundation of the program both for the educational task when it comes to the early detection of this type of patients and for the positive reinforcement that self-evaluation generates.7,9 ECMO teams are mobile specialized teams that assess the need for specialized transfers to the tertiary referral center with or without ECMO which allows the universalization of the program.7,10,25–27
We call it primary ECMO transport when the team from the tertiary referral center is transferred. Also, it is this team that evaluates and implements the support for the transfer. We call it secondary ECMO transport when therapy is initiated at the referring hospital and the patient is then transferred to the tertiary referral center by the team from one center or the other.27 This requires a greater availability of resources, training, and experience managing ECMO systems and it is an established and more advanced program.
The increased number of patients transferred on ECMO to tertiary referral centers has multiplied 5-fold since 2011 in some regions thanks to the existence of these programs.28 Future studies on the cost-effectiveness of these programs are necessary compared to those programs without an established coordination.12
The ECMO transportation teamECMO transportation teams should be coordinated by the tertiary referral center and the team members should be trained and be experienced in the management of patients on ECMO7,10,26,27 and also be used to transferring critically ill patients; when it comes to aerial transportation, the team in charge should be specifically trained in aerial transportation too.28 Training in ECMO aerial transportation can be essential since this training can end up saving the day and controlling the most severe adverse events induced by equipment malfunctioning in a hostile environment.29
There are different team configurations based on how experienced the center is and on the type of transfer performed.
All the different responsibilities of the process need to be well established and there needs to be one27,30:
- 1.
Intensivist:
- •
Coordinator of the transfer and coordinator of both centers involved in this process.
- •
The coordinator is the person responsible for the patient and performs the clinical evaluation of the patient and decides whether to prescribe the ECMO therapy. The coordinator also informs the family and signs the patient's informed consent.
- •
The coordinator makes all the decisions that pertain to the patient and the ECMO system until arrival at the tertiary referral center (by programming blood flows and ECMO flow rates, dose of anticoagulation drugs, fluid-management strategies, vasopressor drugs, etc.)
- 2.
Physician responsible for cannulation: in some centers the person in charge is the cardiovascular surgeon. In others, it is the intensivist trained in percutaneous cannulations.
- 3.
ECMO specialist: perfusionist, physician or nurse.
- •
ECMO circuit equipment.
- •
Material required in the referring hospital for the entire procedure.
- •
ECMO circuit priming.
- •
Management of the ECMO circuit during the transfer.
- 4.
Nurse specialized in intensive care:
- •
Nursing care.
- •
Administration of drugs, fluid therapy, blood, etc.
- 5.
Specialist in respiration techniques and transfers.
- •
Mechanical ventilation, connection, and gas exchange.
- •
This task should be the responsibility of the referring physician whenever there is not enough room for the entire team aboard the means of transportation.
Just to mention a few examples, the team from the Karolinska Hospital in Stockholm, Sweden includes one surgeon, one intensivist experienced in ECMO systems, one perfusionist and, on some occasions, even one specialized nurse.30 The team of Columbia University in the City of New York, New York includes one cardiothoracic surgeon, one fellow surgeon, two perfusionists and two paramedics specialized in the management of critically ill patients.31 In the French Guiana, the team is made up of one cardiovascular surgeon plus one MICU (mobile intensive care unit) physician with or without an intensivist and/or perfusionist.32
ECMO criteria for the transfer of patients with acute respiratory failureRecent reviews on the management of severe SARDS recommend ECMO as the bailout therapy in patients with refractory hypoxemia to the optimal ventilatory therapy and different techniques like the prone decubitus position. For the time being, there are no consensus recommendations due to the lack of significant evidence as we wait for the findings of the ongoing EOLIA study (NCT01470703) that will outline the criteria for the use of ECMO in the management of SARDS.12,16,33 The Extracorporeal Life Support Organization (ELSO) guidelines recommend ECMO with PaO2/FiO2 ratios <150 and indicate the use of ECMO with l PaO2/FiO2 ratios <100 or respiratory acidosis with a plateau pressure (Pplat) >30cm HO2.34 These criteria are in direct contradiction to recent reviews that remain expectant and recommend the use of ECMO in the most severe cases of SARDS.16
Where we find more consensus is in how early therapy is implemented, since mortality rate decreases when ECMO is implemented during the first or second day of refractoriness to the optimal ventilatory therapy.25,34
The transfer of patients with moderate-to-sever respiratory failure to tertiary referral centers on mechanical ventilation and ECMO is extremely risky and even more risky in patients with severe hypoxemia and/or respiratory acidosis. The transfer on ECMO has proven such a safe transfer for these patients compared to without extracorporeal support10,24,25 to the point of wondering whether there should exist specific ECMO criteria in transfer-eligible patients.
The procedure used in the ECMOnet study implemented ECMO by using criteria of less severity in transfer-eligible patients. PaO2/FiO2<70 with PEEP>15cmHO2 if at the tertiary referral center and PaO2/FiO2<100 with PEEP>10cmHO2 if they were transfer-eligible patients.10,23 Growing experience has adjusted these inclusion criteria. In a later study, PaO2/FiO2<85 and/or respiratory acidosis with pH<7.2 were the criteria used to activate the protocol and make the necessary assessment by the ECMO team. After the optimal mechanical ventilatory therapy and rescue breathing maneuvers, 13% of the patients were safely transferred without ECMO meeting the following criteria: pO2>90mmHg with FiO2 1, PCO2<65mmHg and PEEP<20.25
One recent meta-analysis that included a total of 1481 patients transferred on ECMO from heterogeneous studies conducted from 1994 through 2016 contradicts the aforementioned being the degree of average hypoxemia pre-ECMO, the ratio of PaO2/FiO2=59 and survival rate around 60%.35 We can do nothing but wait for future studies and be cautious when transferring patients with severe SARDS while assessing how early the therapy should be implemented and the possible criteria of less severity to implement ECMO due to the high risk associated with the transfer.
ECMO criteria to be transferred in the presence of cardiogenic shockThe latest recommendations on the management of cardiogenic shocks include mechanical circulatory support techniques in cases of refractoriness to the standard therapy with a class IIb grade of recommendation.20
The Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) scale used for the stratification of the severity of heart failure and its mortality rate allows us to make the correct assessment of those patients who will benefit from this or that mechanical circulatory support device and eventually establishes the prognosis after an emergent heart transplant (Table 1).20,36,37
The Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) Scale.
| INTERMACS | Description | Time to circulatory support | Survival with support |
|---|---|---|---|
| 1 | Hemodynamic instability despite growing dose of catecholamines and/or mechanical circulatory support with critical hypoperfusion of target organs (critical cardiogenic shock) | Short-term circulatory support. Percutaneous support/ECMO | 52% |
| 2 | IV inotropic support with acceptable figures of blood pressure and rapid deterioration of the renal function, the nutritional status or signs of congestion | Short-term circulatory support. ECMO/VAD. In days. | 63% |
| 3 | Hemodynamic stability with low or intermediate doses of inotropic drugs and impossibility to withdraw such drugs due to hypotension, symptom deterioration or progressive renal failure | VAD. Elective in weeks. | 78% |
| 4 | The transient withdrawal of the inotropic therapy is possible, but the patient shows frequent symptom recurrence usually with fluid overload | VAD. Elective in weeks or months. | 78% |
| 5 | Absolute restriction of physical activity with stability at rest usually accompanied by moderate fluid retention and a certain degree of renal dysfunction | VAD, weeks or months. | 93% |
| 6 | Less restriction of physical activity and lack of congestion at rest. Fatigue with light physical activity | VAD pending assessment | – |
| 7 | Patient in NYHA functional class II–III without unstable fluid balance | N/A | – |
ECMO: extracorporeal membrane oxygenation; NYHA: New York Heart Association; VAD: ventricular assist device.
In cases of refractory cardiogenic shock in stages 1 and 2 of the INTERMACS scale, it is advisable to use short-term circulatory support devices as a bridge to myocardial recovery or consider the implantation of long-term devices and/or heart transplant.12–22,37
The experience of the treating team is the key here, since they choose what the optimal time is to implant the device. On some occasions they can implant it very early or very late which is futile therapeutics.21 Scales such as the SAVE-score can help when it comes to assessing what the optimal time is for the implantation of these devices.38
It is highly controversial what the optimal device is in the acute phase,12,18,39 since the lack of a complete ventricular discharge can make the situation worse or keep a phase of multiple organ failure. These are some of the percutaneous devices we use today: the intra-aortic balloon pump (IABP) counterpulsation, the peripheral VA-ECMO cannulation and new devices such as the Impella® or the Tandem Heart® bypass. The latter two are placed through arteriography; the Impella® provides left ventricular support only and the Tandem Heart® provides biventricular suppport.12,18,39 For the time being, the experience curve with these devices is low, the cost compared to the ECMO is higher, they may not provide enough hemodynamic support in the most severe cases,12 and they are difficult to implement in programs of primary ECMO transport. Actually, the IABP is not recommended anymore on a routine basis in cases of cardiogenic shock,18 although some studies advocate for its concomitant use with the VA-ECMO to improve hemodynamics and reduce the risk of PAD.40,41
There are no prospective studies on the transfer of patients with cardiogenic shock. On this regard, we can mention the retrospective studies conducted in the French islands that analyze long-distance VA-ECMO transfers (136–10,000km) to centers specialized in heart trasplants.32,42,43 In the most recent study conducted on evacuation-eligible patients, 57.6% were transferred with the VA-ECMO system and 78.6% with the IABP. Patients transferred with circulatory support showed similar survival rates to those in whom the ECMO was implemented in the tertiary referral center (36.8% vs. 37%) and with similar post-heart transplant results to those who were transferred without circulatory support (85.7% vs. 83.3%) yet despite the fact that the former were in more critical condition.43
When it comes to VADs, they allow a medium-term full hemodynamic support as a bridge to the heart trasplant.20 Also, VADs can be used as a bridge to recovery, above all in young patients with potentially reversible conditions such as myocarditis or postpartum cardiomyopathy.20 The implantation of the VAD in the referring hospital followed by the patient transfer to the tertiary referral center specialized in heart transplants is well documented, it requires highly experienced centers on both ends, and a prior evaluation of the transplant-eligible patient.44,45
Other possible applications of the ECMO transferOut-of-hospital cardiopulmonary resuscitation with ECMOThe ECMO cardiopulmonary resuscitation (ECPR) may provide better neurological results compared to conventional cardiopulmonary resuscitation (CPR) and contribute to the donation of organs in patient who die.12,46–48 Nonetheless, the findings from controlled prospective studies so far are still in their infancy.12,49,50 The importance of receiving quality CPR immediately plus the right choice of patient accompanied by an early ECMO therapy48 has prompted studies on its convenience in out-of-hospital settings. Anticipating ourselves to future favorable findings on these techniques in the out-of-hospital setting, we should wonder whether we are ready to do this.
Organ donation in controlled asystole programsThe implantation of VA-ECMO in controlled asystole programs has had better results than the ultra-rapid organ extraction method.51,52 Sending a mobile unit of transplant coordinators with the necessary equipment and personnel to the referring hospital is well documented, so the option of controlled asystole donation could be offered here in hospitals where this resource does not exist.53
Patients with relapsing acute respiratory failure who remain on the transplant waiting listThe transfer of patients with relapsing acute respiratory failure who remain on the lung transplant waiting list to tertiary referral centers specialized in transplants is considered a high-risk transfer only to be conducted by specialists with the necessary means. Intubation and connection to mechanical ventilation is associated with poor results in the post-lung transplant period. Both the ECMO and extracorporeal CO2 removal (ECCO2R) systems implanted in awake patient as a bridge to the lung transplant have improved the survival rate in this type of patients.16,34,54 When it comes to the ECMO transfer of awake patients, for the time being, evidence is limited to case description but with good outcomes.55
ECMO transfer: choosing the right means of transportationThis is something that depends on the ECMO programs we are dealing with, so each country should study its own situation. Choosing this or that means of transportation depends on different variables: distance to cover; type of terrain; type of roads; hospital structures; meteorology in the region and availability of the right means of transportation with the adequate technology for the transfer.33,56,57
The recommendations on the means of transportation that should be used are highly variable. British guidelines on the transfer of critically ill patients recommend using a helicopter when the distance is more than 80km and a medicalized plane when it is more than 240km,57 while the ELSO guidelines recommend ground transportation when the distance is up to 300km, helicopter transportation when it is up to 600km and airplane transportation when the distance is more than 600km.27,58
It is important to analyze the evolution in those countries where numerous transfers of critically ill patients are done and in ECMO and see how these transfers have not evolved the same due to other determinants such as weather conditions and night time. For example, despite the fact that the Karolinska Hospital has the necessary hospital structures, its ECMO transfers are based on ground transportation for distance under 300km and aerial transportation for longer distances, which is used in 60% of the transfers.29 In other European regions with different conditions the inter-hospital helicopter transportation of critically ill patients has been growing thanks to the adaptation of infrastructures and the introduction of high-performance helicopters: German studies on ECMO transfers speak about helicopter transportations of somewhere between 60 and 178km.59
Ground transportationGround transportation on an ambulance is the most widely used means of transportation for healthcare purposes. One recent meta-analysis confirmed that 53% of ECMO transfers happen on an ambulance.35 The main advantages of this type of transportation are its availability, cost, and possibility to use in almost all situations.27 The availability of ambulances for the transfer of complex patients who require a great deal of material, equipment and personnel is relative, and it is questionable whether conventional ambulances are the optimal means of transportation for this type of transfers. The Karolinska Hospital uses one medicalized bus for ECMO transfers. The need for massive ground means of transportation delays the transfer in round trips, which is why some centers use a fast vehicle with personnel and equipment. Another aspect that should be taken into consideration here is the state of the roads to be used, since winding roads will delay transfer times even more making healthcare more difficult in these circumstances.
Helicopter transportationA study conducted by Mendes et al. says that 22% of the transfers happen on a helicopter.35 The helicopter provides speed, stability and bed-to-bed transfer without any other intermediate means of transportation; this would lead us to think that it is the optimal means of transportation for critically ill patients.
It is important to analyze the helicopter balance between the room at the cockpit and the maximum takeoff weight always according to the available infrastructures. The following aspects are important too: cruise speed; stability data; noises and vibrations. Autonomy times are importance even in the absence of long-distance trips, since this increases the range of possibilities and reduces transfer time.
The helicopters used for ECMO transfers should be spacious and admit a variable weight between 500kg (the smallest pieces of equipment) and 1000–1200kg (2 pilots, full ECMO equipment, patient and material). Helicopters such as the EC-145, Bell 429, Bell 412, or the new AW 169, have a high performance with a more limited maximum takeoff weight. Other helicopters used are the AW 139 or the Sykorsky S76, wide and stable, but more expensive, heavier and need less available infrastructures.
Some of the disadvantages of helicopter transportation are the need for a hospital infrastructure update and the need for implementing aeronautical technology to improve night flights and be able to fly with poor meteorological conditions.
To date, no study has analyzed specifically cost-effectiveness when it comes to ECMO transfers and the very few that have are not easy to compare due to the different models of funding. The higher cost-effectiveness of medicalized aerial transportation depends on several criteria: moderate distances (80–350km); direct transfers without the need for ground transportation; highly qualified medical personnel; the right management and type of patient to be transferred.6,56,57
Airplane transportationThe advantages of the airplane are: stability; room; constant pressurization; autonomy and lack of weight limitations regardless of weather conditions and night flights. Its disadvantages are that it depends on airports and the associated logistics and the fact that there is this need for pre- and post-transfers in an ambulance.27,56,57 Historically, twenty-seven per cent (27%) of the transfers have been conducted through this means of transportation which in turn has made long-distance ECMO transfers possible – 7% of the overall international transfers.35
Equipment and preparations for the transferPlanning ECMO transfers includes reviewing the entire necessary equipment and material and checking the compatibility with the means of transportation chosen (electric connections; voltages; fastenings). It is mandatory to get a hold of all the equipment, the battery-run time, and whether it is possible, or not, to change the batteries. Also, it is advisable to have some sort of power source to feed all the equipment. In the case of aerial transportation, it is mandatory that the specific model of airplane or helicopter used has been certified by Civil Aviation and also that all electromagnetic devices have been adjusted to avoid interferences during the flight.1,26–28,56,57
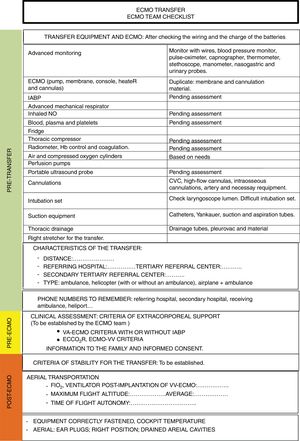
Each ECMO program designs its own equipment and material based on the missions required and experience of the teams in charge. Backpacks and checklists to reduce the possibility of forgetting this or that piece of equipment are recommended (Figs. 1 and 2: editable checklist templates).27,29,30,60,61
Proposal of checklist for the referring hospital: ECMO team activation criteria; clinical data; analytical data and relevant imaging modalities; equipment required and room needed to arrange the extracorporeal support. IABP: intra-aortic balloon pump counterpulsation; ECMO: extracorporeal membrane oxygenation; MOF: multiple organ failure; HR: heart rate; iNO: inhaled nitric oxide; DBP: diastolic blood pressure; ABP: average blood pressure; SBP: systolic blood pressure; PEEP: positive end-expiratory pressure; CT: computed tomography; CRRT: continuous renal replacement therapy.
For advance monitoring purposes the following pieces of equipment are a necessity: LAP; pulse oximeter; BIS; capnography; PWP and brain oximetry, if necessary; blood; platelets and plasma; fridge; 2 surgical teams; cannulation devices and double ECMO membrane. Especially in primary ECMO transports the following may be needed: thoracic compressor; portable ultrasound probe; portable radiometer; coagulation monitoring and hemoglobin. It is necessary to have a stretcher or sled for the transfer fit for this type of patients and with capacity to fasten the entire equipment.26,27,56 There are stretchers available specifically designed for ECMO transfers with the possibility of fastening the equipment without having to place it inside the means of transportation.
The mechanical ventilator and the transport monitor should provide us with the most advance technical capabilities and at the same time should be portable; there are portal mechanical ventilators available adjusted to barometric pressure. This capability together with portability and vibration attenuation is also offered for transport IABP. There are various types of ECMO devices used for transportation purposes; it is important to know the weight and volume these devices occupy as well as the technical specifications, since all devices provide the same capabilities. It is advisable that the weight of the entire equipment necessary for cannulation and ECMO itself does not exceed 35kg in cases of aerial transportation.32
Need for air and oxygenIt is important to know the amount of oxygen and compressed air needed always bearing in mind the possible setbacks that may occur and that will make waste time. The problem of logistics and running out of oxygen are relatively common incidents here.29
One patient on ECMO or VAD with an additional oxygenation membrane will be using mechanical ventilator and membrane outputs so we need to know both volumes per minute. The ECMO device during the transport and during most of the veno-venous therapy is configured with FiO2 1, being sweep air (from 0 to 10lpm) the ECMO volume/minute which will be configured based on the patient's ventilatory needs (usually a 1:1 ratio with the blood flow).34
Portable mechanical ventilators allow us to mix oxygen and ambient air and run independent from compressed air allowing us to get rid of this type of cylinders. There is an extra gas output that the ventilator uses for internal control – usually between 100 and 500ml/min.62,63 It is advisable that the ventilator FiO2 is the lowest possible one while still making sure we are providing the right oxygenation. Also, that the mechanical ventilation is protective or ultra-protective.64
Once we know what the exact demand for air and oxygen is and the estimate transfer time, then we will know how many cylinders we need65 (additional material [Tables 1E and 2E]). During the transfer it is important to monitor the output and the liters available, so we can anticipate any problems on this regard. There are medical oxygen cylinders available with digital screens with the time available without having to do calculations at nanometric scale.
Planning the transferLogistics issues lead to waste time in the transfer and associated risks and a greater number of nosocomial infections and adverse events during long-distance transfers have been reported.29,43 That is why systematizing the transfer can improve the results.
It is advisable to think that wasted time is something that can happen and draw a back-up action plan knowing the characteristics and location of alternative hospitals. It is important that both the transfer and the medical teams are on the same page and in the case of aerial transportation, it is important to design a flight plan together with the pilots. Also, it is advisable to have information on possible target heliports, urgent refueling areas during the itinerary and, ultimately, establish what will be the average and maximum flight altitude depending on the clinical situation of each patient.
Characteristics of aerial transportationDuring the flight we should take certain measures into considerations to prevent hypothermia, sound, vibrations, and the energies released during acceleration and deceleration maneuvers. The advances made in the fields of technology and healthcare have minimized these issues and no secondary complications have been reported so far.29,32 Another factor that may affect respiratory and pediatric patients is low humidity rate (close to 10%),66 which is why active humidification measures in high-risk patients should be taken into consideration here.
The influence exerted by aerial transportation on our patient is due to a reduced partial pressure of oxygen in the alveoli (PAO2) and an increased volume of gases as pressure goes down with the increasing altitude.66–69 The literature of complications of hypoxemia due to a reduced PAO2 is scarce (3–4%).32
To this day no specific study has approached the physiology of patients on ECMO when facing altitude changes, which is actually important for a safe transfer and to individualize the flight plan. Higher flight altitudes reduce the helicopter gas output, which in turn increases its flight autonomy and with it, the possibilities of transportation without making any additional stops while improving cost-effectiveness.
In altitude the volumes per minute go up both for the ECMO and the ventilators, and we may run the risk of hyperventilating our patient.66–69 Today the equipment is more and more adapted to aerial transportation and it has been modified to meet the barometric pressure requirements as it is the case with some mechanical ventilators and IABPs, yet, for the time being, ECMOs do not have this capability. It is possible to create estimates based on the Boyle–Mariotte law to know what effects altitude will have on the ventilation (additional material [Tables 1E and 3E]). This is one of the reasons why a portable radiometer may be a good idea.
Similarly, to estimate the FiO2 we will need to increase the duration of the ventilation at a given altitude, individualize the flight plan or even contraindicate aerial transportation (additional material [Tables 3E and 4E]).
Complications during the transferMortality during the ECMO transfer is close to zero compared to transfers without extracorporeal support.23–25,29,35 We should mention here one recent study that specifically evaluates the adverse events occurred in 514 ECMO transfers. We should also mention here that most of these transfers were primary and 59% were airplane transportations, which may be indicative of the complexity of the cases analyzed. In this study, the probability of suffering an adverse event was 40% – higher in transfers that took more than 3h. Tables 2 and 3 show the classification of adverse events and the frequencies with which they were registered.29
Adverse events recorded during ECMO transfers and categorized into causes and absolute frequency per group.
| Causes for adverse events | Frequency | Adverse events |
|---|---|---|
| Due to the patient | 65% | • Accidental extubation |
| • Low level of sedation | ||
| • Bleeding | ||
| • Cardiac dysfunction | ||
| • Hypovolemia | ||
| • Recirculation | ||
| • Arterial ischemia | ||
| • Other | ||
| Due to the medical equipment | 14.6% | • Damaged materials |
| • Worn out oxygen | ||
| • Circuit thrombosis | ||
| • Electrical failure | ||
| • Worn out batteries | ||
| • Other | ||
| Due to the medical personnel | 5.8% | • Communications failure |
| • Overlooked material | ||
| • Lack of personnel | ||
| • Other | ||
| Due to the means of transportation | 12.6% | • Logistics failure |
| • Erroneous ambulance | ||
| • Traffic | ||
| • Electric supply failure | ||
| • Other | ||
| Due to the environment | 1.9% | • Freezing of venous accesses |
| • Other |
Source: Ericsson et al.29
Adverse events recorded during ECMO transfers and categorized into levels of severity and absolute frequencies per group based on causality.
| Risk grading | Definition | Frequency | Subgroup analysis per cause |
|---|---|---|---|
| Category 1 | Repercussion on mortality or high morbidity if not solved in a matter of seconds | 7.8% | 19% patient 50% medical equipment 19% medical personnel 12% environmental causes |
| Category 2 | Repercussion on mortality or high morbidity if not solved in a matter of minutes | 58.7% | 93% patient 2.5% medical equipment 2.5% medical personnel 1.7% environmental causes |
| Category 3 | Intermediate risk that does not lead to an imminent risk of morbimortality but requires a solution | 22.8% | 34% patient 19% medical equipment 13% medical personnel 34% means of transportation |
| Category 4 | Low risk if dealing with this or that event during the transfer | 10.7% | 9% patient 45% medical equipment 45% means of transportation |
Source: Ericsson et al.29
Based on these findings we can say that most adverse events that happen during ECMO transfers are due to the patient29 and most of the time they are common incidents occurring during the first few hours of an ECMO program. A team experienced in techniques of extracorporeal support is usually aware and trained in all these issues and its response margin is usually higher. On the contrary, most adverse events-induced risks of imminent consequences are due to issues with the medical equipment29 and the transfer per se. The team here is not very familiar with all these issues. Also, it is surprising to see that 19% of imminent risks are due to mistakes made by the medical team – mainly due to miscommunication.29 All this makes us think that specific training on how to transfer critically ill patients and do ECMO transfers is a necessity with specific training on medical and technical issues and team work.70
ConclusionsExtracorporeal support with ECMO is indicated in cases of refractoriness to therapy, in cases of cardiogenic shock and respiratory failure and in aggravated patients who have received a heart and lung transplant. The experience and volume necessary to obtain good results together with the great number of resources needed are the reasons why extracorporeal support programs are required. These programs should be coordinated by the tertiary referral center specialized in ECMO programs and by the heart-lung transplant centers through a comprehensive network specialized in ECMO programs.
Evidence on the exact criteria that should alert the transfer team and the criteria required for mechanical ventilation under transfer conditions is scarce. The patient's safety and the cost-effectiveness of the entire system should be taken into consideration. Also, new studies on the utility of these programs should be conducted in the future.
A team specialized in ECMO programs is key for the clinical evaluation of the patient and for safety purposes during the transfer. Technological knowledge under transfer conditions and the specific training of the critical transfer team are essential to be able to handle any equipment problems that may pose imminent danger.
The impossibility to apply the studies of cost-effectiveness on means of transportation because every region and system are different leading to specific individual analysis of each case. Thanks to its speed; possibility to cover long distances without the need for any other means of transportation and stability, the helicopter would be the ideal means of transportation for medium distances as long as hospital infrastructures and the necessary aeronautical resources are available and weather permitting. Although the safety of this means of transportation has already been described, the physiology of ECMO under altitude conditions still needs to be studied to increase safety during the transfer and individualize the flight plan of every patient. Ground transportation is still the most widely used means of transportation due to its availability and cost. Nonetheless, the ambulance should be adapted to meet the specific needs of the transfer of critically ill patients and ECMO. Long-distance transfers and airplane transportations associate more logistics and medical incidents but bring ECMO to remote areas and with a positive benefit–risk analysis.
ECMO transfers are a challenge for the healthcare system, due not only to their technical or medical complexity, but because they entail the creation of a structure that can lay the foundations of multidisciplinary relations in out-of-hospital settings and increase inter-hospital relations for the good of the patient.
Conflict of interestsThe authors declare no conflict of interests whatsoever.
Please cite this article as: Burgueño P, González C, Sarralde A, Gordo F. Transporte interhospitalario con membrana de oxigenación extracorpórea: cuestiones a resolver. Med Intensiva. 2019;43:90–102.