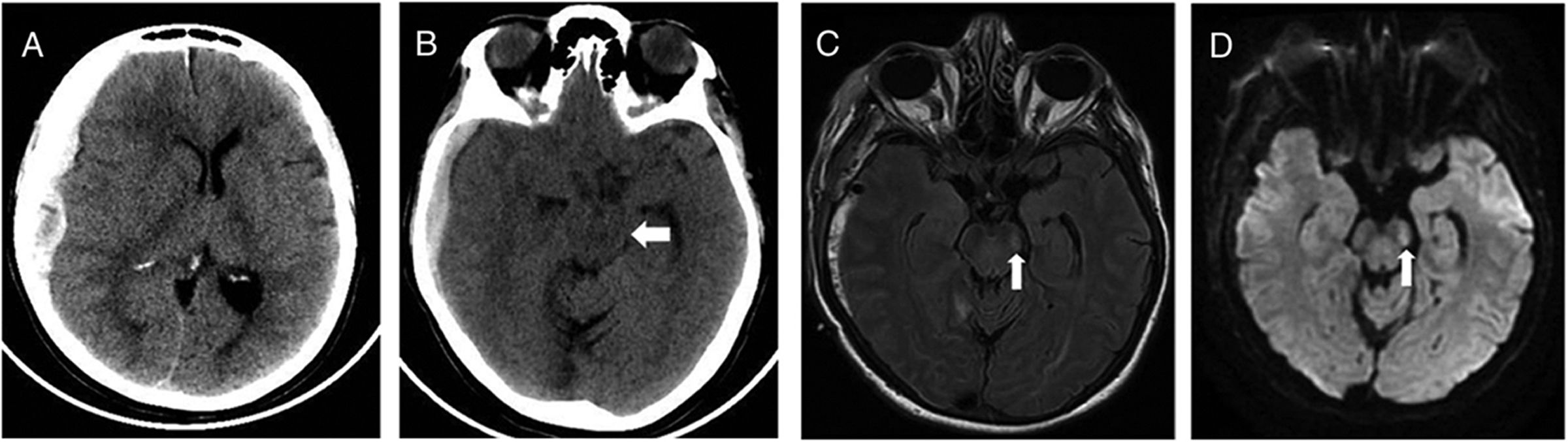
A 60-year-old woman, with past medical history of stroke (under treatment with aspirin and clopidogrel) presented with headache and incomplete palsy of III right cranial nerve. The patient referred a minor head trauma some days ago. Brain computed tomography (CT) showed an extended right-sided subdural haematoma (14mm), with mass effect, and midline shifted to the left (10mm) (Fig. 1). A craniotomy and evacuation of the subdural collection was done. The patient awaked confused, with right-sided hemiparesis. Cervical spine pathology and stroke were excluded. Magnetic Resonance Image (MRI) of the brain showed changes in the contralateral cerebral peduncle, compatible with Kernohan–Woltman notch phenomenon. She was transferred to the general ward with moderate right-sided hemiparesis.
Brain CT showed extended right-sided subdural haematoma (A), with compression of left cerebral peduncle against free tentorial (B, white arrow). Brain MRI reveals a rounded hyperintense T2 FLAIR (C) and DW1 (D) images in left cerebral peduncle (white arrow), at 2 days after initial injury.
Neurointensivists should recognize Kernohan–Woltman notch phenomenon as a paradoxical neurological manifestation of an ipsilateral motor deficit to the primary brain injury. The compression of the contralateral cerebral peduncle against the free tentorial, and the disruption of the corticospinal tract fibers above the medullary decussation, is the causes of this false localising neurological sign.