To determine the life-sustaining treatment limitation (LSTL) predisposition upon patient admission to the Intensive Care Unit (ICU), the criteria upon which such predisposition is based, and whether these decisions are related to structural factors of the surveyed hospitals.
DesignA descriptive multicenter study was made in 2010, involving the conduction of a survey in 90 hospitals, with a view to documenting the usual practise referred to LSTL upon admission in these centers.
SettingSpanish ICUs.
InterventionOpinion survey.
Main variables of interestType of hospital, number of hospital beds, ICU and semicritical patient beds, usual bed availability in the ICU, use of restrictive admission criteria, use of LSTL criteria upon admission, and type of criterion used to decide LSTL.
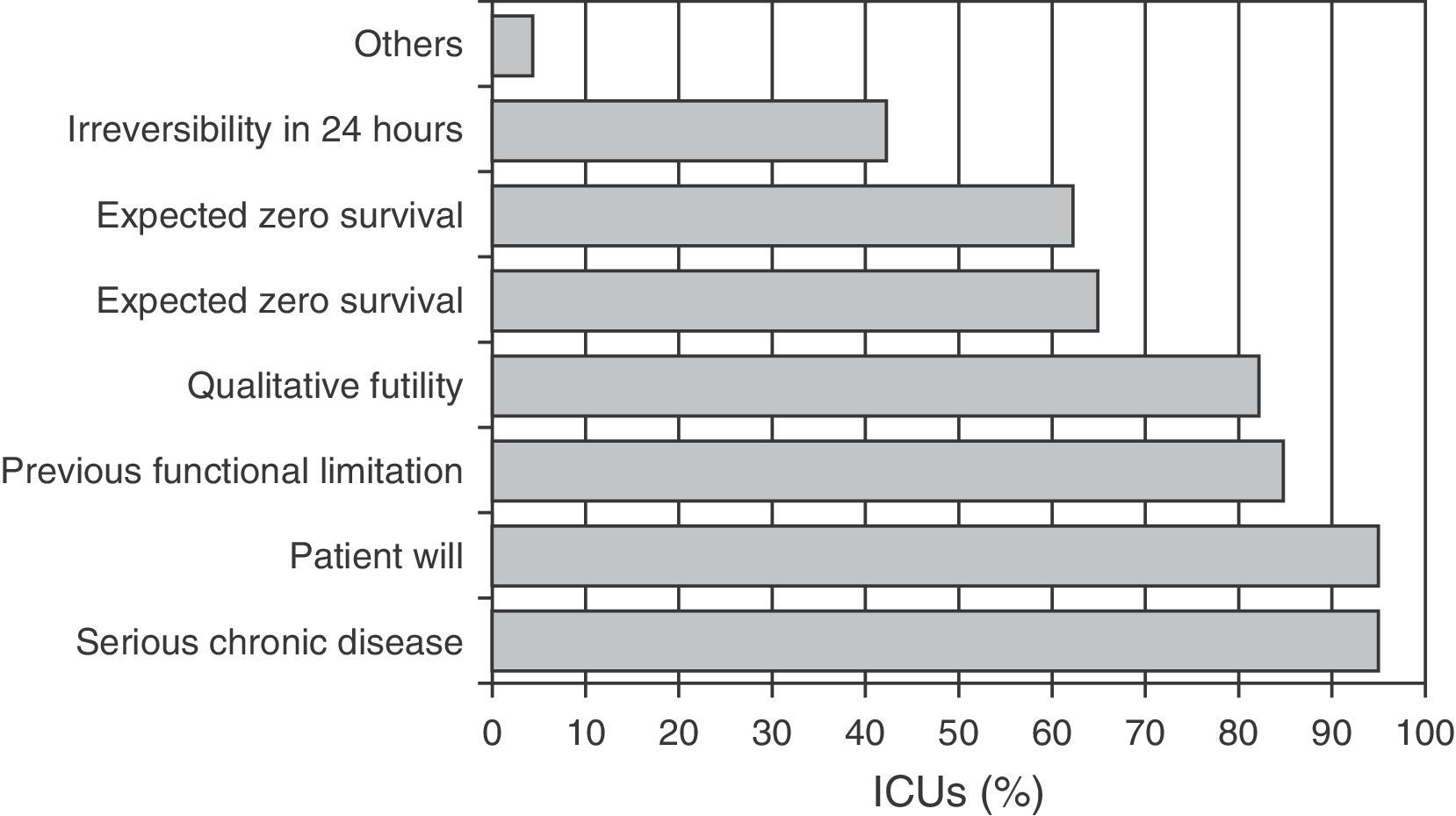
ResultsA total of 43 (48%) hospitals participated in the study, with LSTL being a common practise in these centers (93%). LSTL was fundamentally decided on the basis of the presence of prior severe chronic disease (95%), observation of previously declared patient will (95%), prior functional limitation (85%), and qualitative futility of care (82%). Frequent ICU bed availability (77% of the hospitals) and the use of restrictive criteria (79% of the hospitals) were also associated to patient admission with LSTL.
ConclusionsAdmission to ICU with LSTL is a generalized practise in Spanish Hospitals. LSTL is decided not only based on physiological futility from an objective medical point of view, but also in observance of ethical and moral implications based on the qualitative futility of medical care.
Conocer la predisposición de la limitación de tratamientos de soporte vital (LTSV) al ingreso en las unidades de cuidados intensivos (UCI), y en base a qué criterios se decide la LTSV y si estas decisiones se relacionan con factores estructurales de los hospitales encuestados.
DiseñoEstudio descriptivo multicéntrico. En 2010 enviamos una encuesta a 90 hospitales dirigida a recoger la práctica habitual de la LTSV al ingreso.
ÁmbitoUCI nacionales.
IntervenciónEncuesta de opinión.
Variables de interés principalesTipo de titularidad del hospital, número de camas hospitalarias, de UCI y de semicríticos, disponibilidad habitual de camas de UCI, utilización de criterios restrictivos de ingreso, utilización de criterios de LTSV ya al ingreso, y tipo de criterio utilizado para decidir LTSV.
ResultadosHan participado 43 (48%) hospitales, en los que el ingreso de pacientes con LTSV es una práctica común (93%). La LTSV se decide mayoritariamente por: la presencia de una enfermedad crónica severa previa (95%), el respeto a las voluntades anticipadas del paciente (95%), la limitación funcional previa (85%), y la futilidad cualitativa (82%). Disponer frecuentemente de camas de UCI (77% de los hospitales) y el uso de criterios restrictivos (79% de los hospitales) también se asoció al ingreso de pacientes con LTSV.
ConclusionesEl ingreso en la UCI de pacientes con LTSV es una práctica que está generalizada en nuestros hospitales. La LTSV se basa en la futilidad fisiológica desde una posición médica objetiva, pero también atendiendo a implicaciones éticas y morales basadas en futilidad cualitativa.
Life-sustaining treatment limitation (LSTL) should be a clinical decision pondered jointly by the healthcare teams and in agreement with the patient or family, and consists of not starting, not increasing, or even suspending the started treatments on the grounds that such treatments are futile and do not afford significant benefit for the patients, in the context of responsibility with due observation of the necessary ethical principles.1
To date, most studies in this field have focused on LSTL applied during admission to the Intensive Care Unit (ICU), in patients in which the initial therapeutic actions have been shown to be futile.2
In this context, futility is understood to be the “quality of a medical act that is not advisable in a given patient because it is clinically ineffective, does not improve the prognosis, the symptoms or the intercurrent diseases, or because it will predictably cause personal, family, economic or social adverse effects that outweigh the expected benefits”.3
It has now been seen that LSTL decisions are also taken upon admission. In 2005, Fernández et al. described a small percentage of patients (1%) with LSTL already established at the time of admission, though with different incidences depending on the hospital involved. These differences are probably attributable to variability in the structural and demographic characteristics of each center.4 The mentioned study does not clarify the criteria used to decide LSTL upon admission, though they probably differ from one hospital to another.
Thus, the possibility of adopting limiting life-sustaining measures exists already upon admission to the ICU–such a limitation being understood as the acceptance of patient admission with the restriction of certain life-supporting measures or the prescription of treatments that are conditioned from the start. In any case, admission of the patient to Intensive Care is not denied even though the possibility of benefit is considered remote.
LSTL upon admission must result from medical consideration, preferably with agreement from the patient or family. Such a consensus is strongly advisable in order to define the objectives of patient care during the stay in the ICU. This is ethically justified, since it avoids situations of diagnostic or therapeutic obstinacy and abides with the principles of equality and fairness.
The present study aims to describe the approach toward LSTL prior to admission to the ICU in our hospitals; evaluate the criteria currently used to decide LSTL; and investigate possible structural factors inherent to each center and which affect these clinical decisions.
Materials and methodsIn the context of an upcoming multicenter study on the factors associated to LSTL at the time of admission to the ICU, we have conducted a prior evaluation of the current usual clinical practise in Spanish ICUs.
Clinical practise was assessed based on a survey designed to examine the demographic characteristics of the hospitals and the criteria for LSTL upon admission used in each ICU.
The survey was developed by an expert in bioethics with experience in Intensive Care. In addition to requesting demographic data, a series of pre-established LSTL criteria were offered, based on routine practise and described in previous clinical studies (with the possibility of choosing one or more criteria). In addition, an open option was allowed for the suggestion of other criteria.
LSTL upon admission was defined as limitation from the start, or increased limitation, of some life-sustaining measure such as mechanical ventilation, renal replacement therapy, hemodynamic support with vasoactive drugs, or artificial nutrition. Denial of admission to the ICU was not regarded as LSTL upon admission.
The survey was administered to 90 centers, with analysis of the following variables: type of center, number of beds in each center, number of beds in the ICU and semicritical patient unit (where applicable), usual availability of beds in the ICU, use of restrictive admission criteria (based on patient age, previous comorbidities and previous quality of life), decision of LSTL upon admission, and type of criteria used in making the decision. The availability of a guide or recommendations referred to LSTL in the hospital was also evaluated, together with the existence or not of a Care Ethics Committee (CEC). The possibility of attending patients with LSTL in other healthcare areas outside the ICU was also evaluated.
Regarding the decision of LSTL upon admission, we asked about the criteria influencing the decision, allowing for answers comprising more than one criterion: patient age; serious chronic disease; previous functional limitation; possible recovery from the acute condition but with unacceptably poor quality of life (qualitative futility); observation of prior patient will or instructions; predictable zero probability of in-hospital survival; predictable irreversibility of the current diseased process in the first 24h; and others.
The survey was answered by a specialist in Intensive Care Medicine (not particularly expert in bioethics or ethical issues) acting in representation of the team and describing usual practise in the hospital while avoiding personal opinion. In accordance with current legislation, the data obtained from the survey were kept confidential.
The data are reported as the mean and standard deviation (SD) for continuous variables, and as percentages in the case of categorical variables. The results of the patients with LSTL were compared to those without LSTL using the Student's t-test for continuous variables and the chi-squared test for categorical variables. Statistical significance was accepted for p<0.05. The SPSS version 15.0 Statistical package was used throughout.
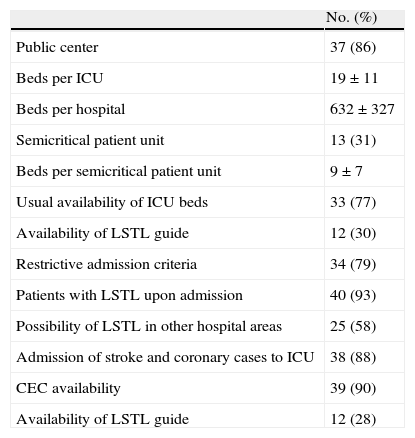
ResultsThe survey was completed by 45 hospitals (50%), though only 43 of the questionnaires were fully evaluable. The great majority of the hospitals were public centers (86%), while 14% were private centers. The mean number of hospital beds was 632, with broad variability (SD 327 beds) (Table 1).
Characteristics of the ICUs that answered the survey.
| No. (%) | |
| Public center | 37 (86) |
| Beds per ICU | 19±11 |
| Beds per hospital | 632±327 |
| Semicritical patient unit | 13 (31) |
| Beds per semicritical patient unit | 9±7 |
| Usual availability of ICU beds | 33 (77) |
| Availability of LSTL guide | 12 (30) |
| Restrictive admission criteria | 34 (79) |
| Patients with LSTL upon admission | 40 (93) |
| Possibility of LSTL in other hospital areas | 25 (58) |
| Admission of stroke and coronary cases to ICU | 38 (88) |
| CEC availability | 39 (90) |
| Availability of LSTL guide | 12 (28) |
CEC: Care Ethics Committee; LSTL: life-sustaining treatment limitation; ICU: Intensive Care Unit.
Forty hospitals (93% of the total) accepted the possibility of admitting patients to the ICU with prior LSTL, and only three centers did not admit patients to the ICU in the presence of LSTL instructions. Most of the centers (77%) claimed to often have free beds in the ICU, and most also applied restrictive ICU admission criteria (79%). In contrast, semicritical patient units were found to still be few in number (present in only 31% of the hospitals). The results showed that 25 hospitals (58%) contemplated the possibility of applying LSTL in other areas of the center outside the ICU.
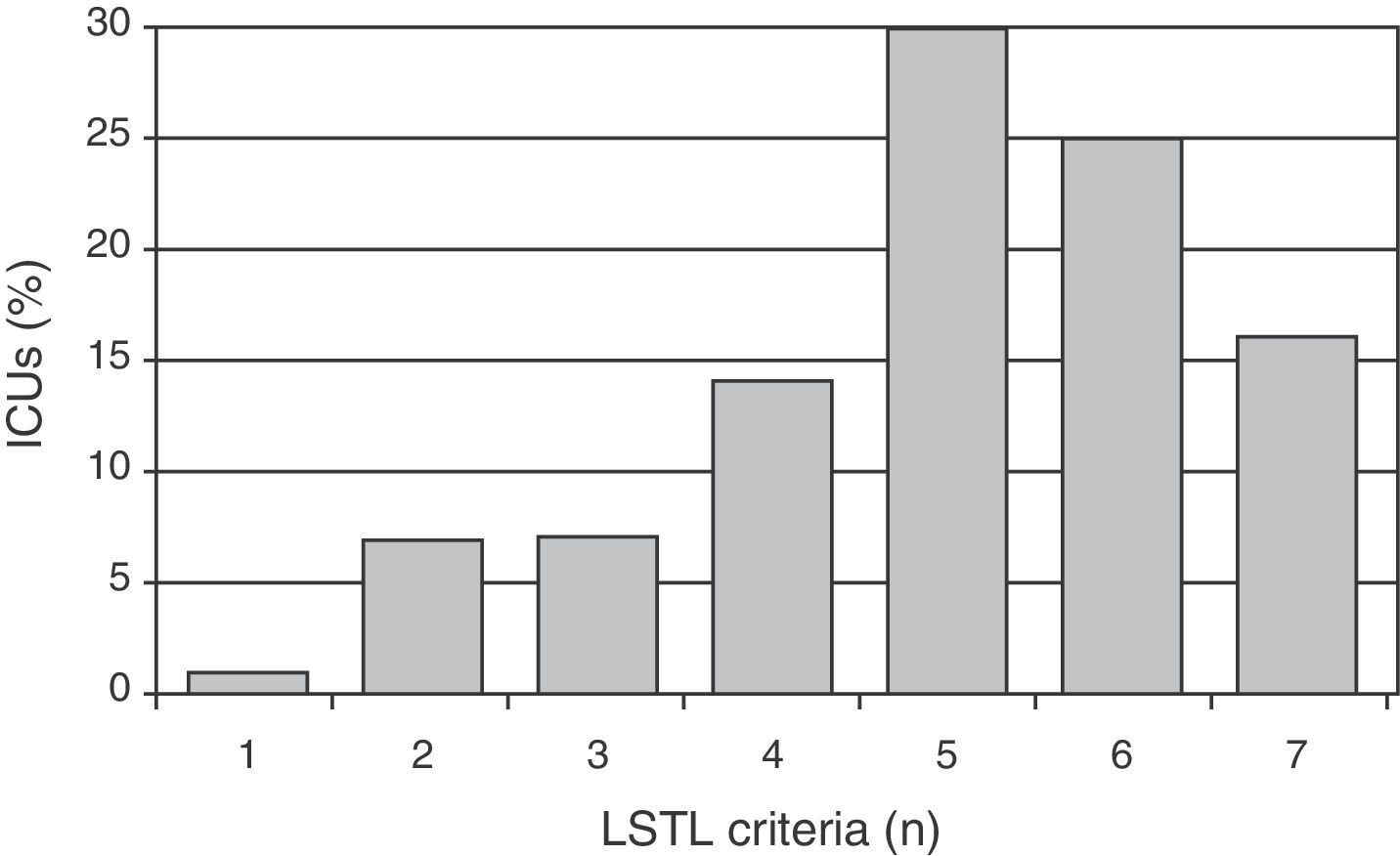
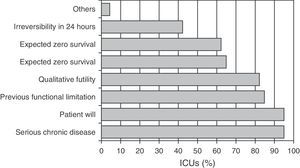
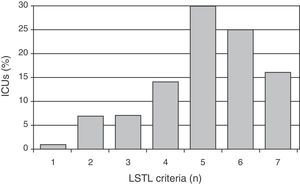
Regarding the criteria for indicating LSTL upon admission (several criteria could be cited by each center), the most frequent were: the existence of previous serious chronic illness (95%), observation of prior patient will or instructions (95%), previous functional limitation (85%), and qualitative futility (82%)(Fig. 1). Fig. 2 shows the number of criteria used by each center in deciding LSTL. Most of the hospitals (86%) cited more than four criteria simultaneously.
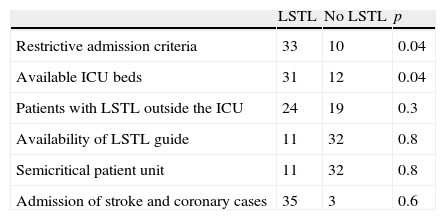
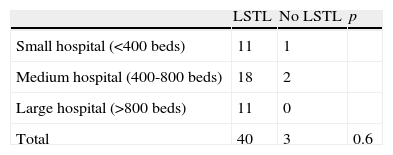
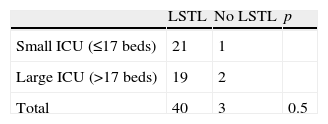
On analyzing the collected variables, the availability of beds in the ICU and the use of restrictive admission criteria were found to be significantly associated to the admission or non-admission of patients with LSTL, though not so the rest of the factors (Table 2). The size of the hospital or the availability of a larger number of beds in the ICU was not found to be associated to a greater disposition to admit patients with LSTL (Tables 3 and 4, respectively).
Factors associated to the admission of patients with life-sustaining treatment limitation (LSTL).
| LSTL | No LSTL | p | |
| Restrictive admission criteria | 33 | 10 | 0.04 |
| Available ICU beds | 31 | 12 | 0.04 |
| Patients with LSTL outside the ICU | 24 | 19 | 0.3 |
| Availability of LSTL guide | 11 | 32 | 0.8 |
| Semicritical patient unit | 11 | 32 | 0.8 |
| Admission of stroke and coronary cases | 35 | 3 | 0.6 |
The results obtained suggest that the decision of LSTL upon admission, as reported by critical care professionals, is a generalized practise among the hospitals that answered the survey.
Ideally, such decisions should be pondered by the healthcare team with the consent of the patient and/or legal representatives, as defined by our scientific society in its LSTL recommendations for critical patients in 2008.5 However, these recommendations are not always followed, and in 12-19% of the cases the decision is made by the medical team on duty before admission.6,7
A previous study described an incidence of LSTL at the time of admission equivalent to 1% of all admissions to the ICU, with an in-hospital survival of 12%.1 This indicates that despite LSTL, some in-hospital survival is observed among such patients. It is in this small percentage of cases where we must reflect upon what can be expected from each admission, from the first moment onwards. The decision is often made individually by the physician on duty, with the agreement of the patient or family, and based not only on the physiological futility of treatment but also on its qualitative futility, centered around responsibility ethics.
All these imply reflection upon whether we should accept as valid the same criteria used for LSTL during admission to the ICU. The answer from most of our hospitals is that the decision is based on the anticipation of physiological futility, sustained by technical considerations, in accordance with medicine based on evidence. However, it is seen that the decisions are also made respecting the will of the patient, and particularly taking into account the previous and expected posterior functional condition of the patient – these criteria being directly related to qualitative futility.
Although our sample of hospitals is heterogeneous in terms of the number of available beds, most of the ICUs normally have vacant beds; this probably facilitates decision making referred to LSTL at the time of admission, with a possibly lesser likeliness of admission if no such beds were available. A very recent study has shown that in patients who suffer sudden worsening, there is a clear relationship between the number of available ICU beds and admission to the ICU and the objectives of patient care, but not with respect to in-hospital mortality.8 In this regard, Colmenero has described that because of the ritual referred to a lack of beds, the admission of one patient to the ICU potentially may affect the admission of another patient.9 A limitation of our study therefore might be this availability of beds at the time of the survey, and the observations probably would differ in situations characterized by a lack of ICU beds.
Despite this availability of beds for admission, the results of our survey show that restrictive admission criteria are used. This suggests that despite the admission of older patients, with more comorbidities, and with LSTL upon admission, we continue to use criteria relating to social justice and the efficient use of resources in deciding admission.
Our survey did not include questions on early or premature discharge, which has been associated with a poorer patient outcome in the hospital ward,10 and possibly might be regarded as a form of LSTL.
We do not know whether there are presently large differences in the admission criteria between hospitals, or whether these differences give rise to a larger or smaller proportion of patients with LSTL at the time of admission–though such differences probably do condition the decisions referred to treatment limitation.
Our survey explored the use of restrictive admission criteria based on patient age, comorbidities and previous quality of life. Most of the hospitals (79%) claimed to use restrictive admission criteria; as a result, the sample of centers is quite homogeneous as regards admission criteria (globally defined as restrictive or non-restrictive). If more data were available on the admission criteria used by all ICUs in Spain, we probably could guarantee greater homogeneity as refers to LSTL upon admission and its relation to the admission criteria. A limitation of the study may be the fact that the survey did not sufficiently characterize the profile of those patients admitted with LSTL and the criteria for admission to the ICU; such data would be interesting with a view to defining which patients and ICU admission criteria are most closely associated to LSTL upon admission.
On the other hand, the results of the survey suggest that LSTL decisions upon admission to the ICU are not conditioned by the availability of semicritical patient beds or the possibility of referring palliative-phase patients with life support measures to other areas of the hospital.
Our results confirm that most of the hospitals abide with the ethical principle of autonomy and respect the will of the patients. This reflects an evolutive change from paternalistic attitudes towards the observation of patient autonomy as based on expressed will. The incidence of written instructions from the patient is not known, but in any case is still very infrequent.6
The survey shows that futility is not only evaluated from a strictly technical perspective but is also related to ethical issues. Medical ethics related futility to aspects such as respect for patient autonomy, beneficence and non-maleficence.11
To our knowledge, this is the first opinion survey on this topic, and casts light upon the criteria used in deciding LSTL upon admission. Without having yet reached prior consensus among the professionals of the different medical societies, it seems that the medical knowledge of physicians and common sense work to establish a minimum body of generalizable criteria that can be based on the presence of previous serious chronic disease, previous functional limitation, and qualitative futility (reversible current disease process, but unacceptably poor quality of life)–despite the limitations that may be associated to such criteria. This would be consistent with the observations of another opinion survey on the limitation of therapeutic effort by intensivists, which suggested that the latter find it harder to stop than to start treatments12; anticipating the futility of life support measures is therefore in line with this approach.
The results of our survey do not differ greatly with respect to the findings of previous studies in which the key elements in deciding LSTL after admission to the ICU correspond to indicators which directly or indirectly quantify the seriousness of the process, such as the NEMS and APACHE II scores, or previous quality of life, admission due to clinical disease, and an age of no more than 80 years.6 Saralegui et al., in a study on LSTL after admission to the ICU, also found futility, the prognosis and poor quality of life to be the different reasons for limiting treatment.13
A recent French multicenter study evaluating mortality under LSTL in Emergency Care Departments, found patients over 80 years of age with metastatic cancer or previous functional limitation to be the individuals most often associated with LSTL.7 In this study the qualitative futility criterion was not cited as a main criterion, in contrast to our own observations. The SUPPORT study underscored the need to talk with the patient and family about the anticipated procedures with a view to improving end of life decisions and the making of decisions–though the study found this practise to be very infrequent.14
In our survey, patient age, foreseeable irreversibility in the first 24h, and expected zero survival received less consideration and priority. Of the options offered by the survey referred to the decision of LSTL, the least used by most of the hospitals was anticipated or foreseeable irreversibility in the first 24h. This points to the need to have a longer time interval before considering LSTL, which reflects greater caution among the physicians in making decisions of this kind. To our knowledge, the only study to have evidenced physiological futility has been published by Cabré et al., reporting a 100% mortality rate among patients with the following conditions: maximum SOFA score >15, minimum SOFA score >10, age >60 years, and deterioration in the first 5 days.15
Although our survey reflects a strong disposition to admit patients with LSTL to the ICU, it must be noted that only a minority of centers (12%) have LSTL recommendation guides. The number of Spanish hospitals with explicit LSTL protocols at this time is not known, though a number of ICUs are showing interest in incorporating LSTL protocols not merely as a guide but as registered parameters in the clinical history.16 However, the availability of an LSTL guide and/or the possibility of consulting the Care Ethics Committee (CEC) was not related to any greater disposition to admit patients with LSTL in our survey.
In conclusion, our study shows that the admission of patients with LSTL to the ICU is a generalized practise, and is decided based on the principle of futility from a medical perspective, but also taking ethical and moral issues into account. In addition, ethical considerations have been shown to be present in patient care, and such bioethical principles are deeply rooted in the daily work of our specialists in Intensive Care Medicine.
Conflicts of interestThe authors declare that they have no conflicts of interest.
The authors thank all the participating centers for their collaboration and willingness in completing the surveys.
Andalusia: Complejo Hospitalario de Jaén, Hospital Universitario Virgen de las Nieves, Hospital Regional Universitario Carlos Haya, Hospital Internacional Xanit, Hospital Parque de Sant Antonio, Asturias: Hospital Universitario Central de Asturias, Balearic Islands: Hospital Son Llàtzer, Canary Islands: Hospital Universitario Nuestra Señora de Candelaria, Cantabria: Hospital Universitario Marqués de Valdecillas, Castilla y León: Hospital Clínico y Hospital Virgen de la Vega (Complejo Hospitalario de Salamanca), Hospital Virgen de la Concha, Hospital Virgen de la Luz, Hospital Rio Hortega, Complejo Asistencial de Burgos, Catalonia: Hospital de Igualada, Hospital de Sabadell, Hospital Universitario Mútua de Terrassa, Hospital General de Vic, Hospital General de Granollers, Hospital Clínico de Barcelona (Unidad quirúrgica y Unidad general), Hospital General de Catalunya, Hospital Universitario Doctor Josep Trueta, Hospital de Mataró, Fundació Althaia, Hospital de Terrassa, Hospital Santa Creu i Sant Pau, Valencian Community: Hospital Clínico de Valencia, Hospital General de Castellón, Hospital de La Fe, Galicia: Complejo Hospitalario Xeral-Cíes de Vigo, Complejo Universitario de Santiago, Complejo Hospitalario de Orense, Hospital Montecelo, Navarre: Hospital de Navarra, Madrid: Hospital Universitario 12 de Octubre, Fundación Jiménez Díaz, Hospital Moncloa, Hospital Gregorio Marañón, Hospital del Henares, Murcia: Hospital Universitario Virgen de la Arrixaca, Hospital Morales Meseguer.
Please cite this article as: Rubio O, et al. Criterios para limitar los tratamientos de soporte vital al ingreso en unidad de cuidados intensivos: resultados de una encuesta multicéntrica nacional. Med Intensiva. 2013;37:333–338.