Our purpose is to validate previously described massive transfusion (MT) scoring in our Transfusion Trauma Registry.
DesignA retrospective cohort of adult trauma patients.
SettingTrauma and Emergency Intensive Care Unit of a tertiary hospital.
PatientsPatients with severe trauma (injury severity score>15) admitted from October 2006 to July 2009.
InterventionsNone.
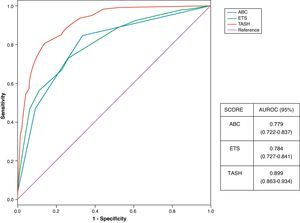
VariablesThe following MT scoring and cutoff points (CP) were evaluated: Trauma-Associated Severe Hemorrhage (TASH) CP: ≥16 and ≥18; Assessment Blood Consumption (ABC) CP: ≥2 and Emergency Transfusion Score (ETS) CP: ≥3, ≥4, ≥6. MT was defined as the transfusion of 10units or more of packed red blood cells in the first 24h. We studied the sensitivity (S), specificity (SP), and positive and negative predictive values (PPV, NPV), the positive and negative likelihood ratios (LHR+, LHR−) and area under the receiver operating characteristic curve (ROC).
ResultsA total of 568 patients were available for analysis; 77.6% were men, with a mean age of 41.16±18 years and an ISS of 30±13. 93.8% with blunt trauma. The overall MT rate was 18.8%. The best S was obtained with ETS≥3 and best SP was obtained with TASH≥18. ROC for different scores was: ABC: 0.779, ETS: 0. 784, TASH: 0.889.
ConclusionThese scales can be useful for characterizing the TM population, for excluding low-risk populations, and for attempting to be objective in hematological damage control and in supporting clinical decisions, based on fe1w and easily obtainable data.
Valorar la utilidad de diferentes escalas previamente descritas, en la predicción de transfusión masiva (TM) con un registro de transfusiones en trauma grave.
DiseñoEstudio retrospectivo de cohortes.
ÁmbitoUnidad de Cuidados Intensivos de Trauma de un hospital terciario.
PacientesSe incluyeron pacientes adultos con trauma grave (Injury Severity Score >15), admitidos desde octubre de 2006 hasta julio de 2009.
IntervenciónNinguna.
VariablesSe evaluaron las siguientes escalas y puntos de corte (PC): Trauma Associated Severe Hemorrhage (TASH) PC: ≥16 y ≥18; Assessment Blood Consumption (ABC) PC: ≥2 y Emergency Transfusion Score (ETS) PC: ≥3, ≥4 y ≥6. TM fue definida como la transfusión de 10 o más unidades de concentrados de hematíes (CH) en las primeras 24 horas del ingreso. Estudiamos la sensibilidad (S), especificidad (E), valor predictivo positivo y negativo (VPP y VPN), razones de verosimilitud positiva y negativa (RVP y RVN) y las curvas receiver-operating characteristics (ROC) y el área bajo las mismas (AUROC).
ResultadosSe estudiaron 568 pacientes, el 77,6% hombres, con una edad media de 41,16±18 años e ISS de 30±13. El 93,8% con trauma cerrado. La frecuencia global de TM fue del 18,8%. La mejor S se obtuvo para el ETS≥3 y la mejor especificidad con el TASH≥18. El AUROC para los diferentes escalas fue: ABC: 0,779, ETS: 0,784 y el TASH: 0,889.
ConclusionesEstas escalas pueden ser útiles para caracterizar la población con TM, la exclusión de población de bajo riesgo, intentar ser objetivos en la resucitación con control de daños y apoyar las decisiones clínicas, con pocos datos y fáciles de obtener.
Traumatisms are an important cause of death among the population between 1 and 44 years of age1 and account for up to 10% of global mortality.2 Bleeding in the context of severe trauma produced by a combination of surgical and coagulopathic hemorrhage is the most common cause of early mortality3 and the second most frequent overall cause of death in trauma.4 New knowledge of the physiopathology of coagulopathy associated to trauma, and military experiences in international scenarios5 have led to a strategic change in resuscitation practices in traumatized patients referred to as resuscitation with damage control, requiring the prompt and aggressive administration of blood products (red cell concentrates, frozen fresh plasma, platelets and fibrinogen).6
This global strategy includes the development of massive transfusion protocols (MTPs). In relation to the logistics and development of MTPs, one of the most difficult and controversial aspects refers to the protocol activation criteria used. Despite the proliferation of such protocols, very few involve a standardized activation policy.7 Delays in treatment and judgment errors in decision taking are causes of mortality during initial patient management,8 particularly referred to the identification of patients requiring massive transfusion (MT), and this has long been recognized in military medicine.9–13 In this context, different MT predictive scales or scores have been developed, combining a broad range of variables in different settings (civilian, military, etc.).14 The present study evaluates different MT activation scores in a Trauma and Emergencies Intensive Care Unit (ICU) of a tertiary hospital center.
Patients and methodsA retrospective cohort study was designed to validate three MT predictive scores, based on our trauma registry and on the transfusion registry of the Unit. These registries that meet the confidentiality criteria applied in our hospital, are anonymous, and have been encoded. The transfusion registry keeps a prospective record of all blood product transfusions, laboratory test results before and after each transfusion indication, cost estimates, complications, and the use of drugs related to hemostasis.
The study included those patients over 15 years of age with severe trauma as defined by an Injury Severity Score (ISS) of >15,15 admitted to our 9-bed Trauma and Emergencies ICU belonging to a third-level hospital attending severe trauma cases in the urban and rural setting, during the period between October 2006 and July 2009. We excluded those patients deceased upon admission and those who rejected blood product transfusions. Initial trauma management is carried out by a specialized team composed of two intensivists (staff physician and resident in training), two patient care nurses and a third registry nurse, and auxiliary personnel – with integration of the different consulting specialties related to the care of patients of this kind, and following internationally recognized management protocols such as Advanced Trauma Life Support (ATLS®).
The hospital has an MTP that has been approved by the Transfusions Commission and hospital management board, and which can be consulted on the hospital website (www.h12o.es).
The following MT predictive scores were chosen in view of the possibility of applying them in our setting:
- (1)
The Assessment of Blood Consumption (ABC) score16,17 assigns a value of 0 or 1 to the presence of penetrating trauma, positive focused abdominal sonography in trauma (FAST), systolic blood pressure (SBP)<90mmHg, and heart rate (HR)>120bpm (the latter 2 parameters upon arrival).
- (2)
The Emergency Transfusion Score (ETS)18,19 contemplates SBP<90mmHg, positive FAST, clinical pelvic instability, age, admission from the scene of trauma, and mechanism of injury (traffic accident or fall from a height of over 3m).
- (3)
The Trauma Associated Severe Hemorrhage (TASH) score assesses 7 independent variables correlated to an increased probability of MT and with different relative impacts: SBP, hemoglobin (Hb), presence of intraabdominal fluid, long bone fractures or complicated pelvic fractures, HR, base excess<10, and male gender.20–23
Different cutoff points (CPs) were assessed for each concrete score:
MT was defined as the administration of ≥10 red cell concentrate units (RCs) in the first 24h after trauma, in accordance with usual practice as reflected in the literature comparing these scores.16–23
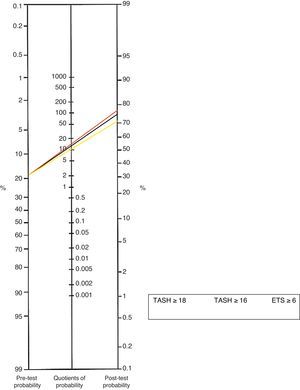
For each score and different CP, we calculated the sensitivity (S), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), positive likelihood ratio (PLR) and negative likelihood ratio (NLR). Based on the combination of pre-test probability and PLR, the use of tools such as the Fagan nomogram allows us to calculate the post-test probability of requiring MT, for a given cutoff point.
Use was made of the pre-test probability (incidence in the series) and PLR for calculating the post-test probability in the Fagan nomogram for the scores and CPs that could prove most useful, with the aim of potentially applying them to a concrete patient – examining the possible combinations in search of the lowest cutoff point capable of predicting the need for MT.24
We likewise plotted the receiver operating characteristic (ROC) curves as graphic representations of the discriminative capacity of a given score based on all its CPs, and calculated the areas under the ROC curves (AUROC) for the scores and CPs that could prove most useful, with 95% confidence intervals.25,26
Comparative inferential statistical analysis was carried out of these areas using the Chi-squared test, with a level of significance of p<0.05. The SPSS version 15.0 statistical package was used throughout.
ResultsWe studied 568 patients with a mean age of 41±18 years. There was a clear predominance of males (77.6%) and of closed trauma (93.8%). The mean ISS was high: 30±13. Some type of blood product was required by 52.9% of the patients, while 18.8% required MT. The mean transfused RC volume was 2.692±2.793ml in the global series and 4.925±3.055ml in the patients with MT.
The values corresponding to S, Sp, PPV, NPV, PLR and NLR for each scale and cutoff point are summarized in Table 1. The ROC curves and AUROC in turn are summarized in Fig. 1. Comparison based on the Chi-squared test was made between the ABC and ETS scores – no significant differences being found. In contrast, very significant differences were found between the TASH and the other two scores (ABC and ETS) (p<0.00001).
Values for the different selected scores and cutoff points.
| ABC≥2 | TASH≥16 | TASH≥18 | ETS≥6 | ETS≥4 | ETS≥3 | |
| S | 43% | 43% | 28% | 66% | 81% | 89% |
| Sp | 90% | 96% | 98% | 94% | 71% | 36% |
| PPV | 56% | 78% | 85% | 66% | 30% | 26% |
| NPV | 84% | 86% | 84% | 86% | 91% | 92% |
| PLR | 4.3 | 13.43 | 14 | 11 | 2.7 | 1.3 |
| NLR | 0.63 | 0.58 | 0.73 | 0.36 | 0.26 | 0.30 |
ABC: Assessment Blood Consumption; ETS: Emergency Transfusion Score; CP: cutoff point; NLR: negative likelihood ratio; PLR: positive likelihood ratio; S: sensitivity; Sp: specificity; TASH: Trauma Associated Severe Hemorrhage; NPV: negative predictive value; PPV: positive predictive value.
For calculation of the post-test probabilities and obtaining a graphic representation of the latter, use was made of the Fagan nomogram27 for the most useful scales and CPs (TASH≥18, TASH≥16 and ETS≥6)—post-test probabilities of about 70–78% being recorded after application of these scores (Fig. 2).
DiscussionMassive transfusion is applied in a very small percentage of patients, though high mortality is involved (40–60%), and the technique consumes up to 70% of all blood products in this type of patient population.28
Early prediction of the need for MT is very difficult to establish, but probably could contribute to improve the development of MT protocols (MTPs) – particularly in relation to early preparation of the corresponding logistics and the availability of frozen fresh plasma, and the definition of adequate blood product ratios.11 The percentage of patients requiring MT in our series was much higher than in other published series (18% versus 3–5% in the civilian population and 8–10% in the military setting).29,30 These differences are explained by the fact that ours was a selected patient sample with high ISS scores, in which many patients meeting the requirements for MT but with traumatisms affecting fewer anatomical regions (e.g., severe orthopedic trauma requiring surgery) were excluded.
On the other hand, there are a number of MT predictive scores that have not been considered in the present study.31,32 Some of these instruments are specific to certain types of trauma such as penetrating chest injuries.11 Some scores have assessed blood loss based on visual estimates,33,34 ionic calcium values upon admission,35 and derived secondary hemodynamic parameters.36
The decision to apply the predictive scores considered in our study was based on their calculating options, on the recommendations of different internationals scientific societies,14 and on their suitability to the type of population involved (civilian in our case).
TASH with high CPs (values of 16–18) has been found to be a better predictor of the need for MT, probably due to the similarity between the studied population and our series – though when applied to routine clinical practice, TASH poses the difficulty of having to deal with a large number of variables in comparison with ABC. The scores are particularly useful for discarding subjects at low risk of requiring MT, as reflected by the high NPV of the different scores and for the different CPs.
Our study has some limitations, some of which are inherent to its design, such as the definition of MT using an a posterior rather than an a priori time concept (with the capacity to determine massive bleeding),37 and the institutional policy with respect to the management of severe trauma and transfusion therapy.
On the other hand, this is a study in which predictive scores are applied retrospectively—though to the best of our knowledge, no prospective studies are found in the literature. Furthermore, some techniques (FAST) imply inter-operator variability, and there is some ambiguity in the definition of certain score variables—these factors being able to affect reproducibility when applying the scores.
Lastly, it should be mentioned that the findings have been useful in upgrading our institutional MT protocol.
ConclusionsMassive transfusion predictive scores can be useful for characterizing patients requiring MT and for excluding low risk populations, and help us to be objective in applying resuscitation measures with damage control, and to design and audit MT protocols—though at present these instruments are probably not able to replace clinical judgment and continuous re-evaluation within the dynamic process of initial trauma management. The choice of a given score must be based not only on its predictive capacity but also on its simplicity and rapidity, and even on the possibility of application the score in the pre-hospital setting. The clinical validation of these instruments requires prospective and multicenter studies38 adapted to the settings in which they are to be used, with the application of appropriate statistical tools and even assessments of the contributions made by each individual component.39
Conflicts of interestThe authors have no conflicts of interest to declare.
Thanks are due to all the personnel members of the Trauma and Emergencies ICU of Doce de Octubre University Hospital (Madrid, Spain), to the Transfusions Commission, and to the Massive Transfusion group of the mentioned hospital.
Please cite this article as: Chico-Fernández M, et al. Escalas predictivas de transfusión masiva en trauma. Experiencia de un registro de transfusiones. Med Intensiva. 2011;35:546–51.