As highlighted by the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias [SEMICYUC]), efficient coordination with other professionals is needed both inside and outside the hospital, to provide effective circuits for critical and potentially critical patients.1 In this context, Departments of Intensive Care Medicine point to the need for a broader and more dynamic approach to critical patients, classifying them according to their needs for care rather than their location.2,3 This approach has implied a change in the way critical care professionals work outside their units, mainly through early detection in hospital wards.3 However, these teams do not usually work in emergency care areas, where workloads are high4 and delays in the management of potentially critical patients have prognostic consequences.4,5 In our center, the Intensive Care Unit provides early management for patients in the emergency department, which is an important part of the care activity. Within the diversity of patients, those presenting with trauma may have serious injuries that initially go unnoticed. These are referred to as potentially critical trauma patients,6,7 and our center has a specific program to deal with such cases (Appendix 1). In order to evaluate these programs, which are carried out in highly complex scenarios, the resources allocated must be correctly determined. In this regard, the article “Estimation of the needs of medical professionals in the Department of Intensive Care Medicine”, published in 2017, emphasizes the importance of calculating the number of activities and the time dedicated by the professionals. Given the difficulty of collecting data in practice, the authors propose a table based on the theoretical times per procedure as a management tool.8 The present study describes the resources in terms of the time dedicated to the care of potentially critical trauma patients compared to the theoretical times found in the literature. As commented in the aforementioned article, knowing the time and activities performed is essential in order to evaluate the efficiency of these programs and to determine human resources.8 We therefore conducted a retrospective observational study of a database of potentially critical trauma patients. The study included patients over 16 years of age, in the period between September 2012 and December 2022, who were treated after activation of the trauma team. Physiological variables (age, gender, heart rate, etc.) were analyzed, along with trauma-specific parameters (mechanism, reason for team activation, Injury Severity Score [ISS]), and variables related to patient care (examinations, tests and procedures). A descriptive analysis was performed, followed by the calculation of the theoretical care time8 dedicated to each patient. The Wilcoxon test was used to compare the theoretical time with the actual time recorded. Finally, a care time model was developed to identify those characteristics that influenced care times above the median.
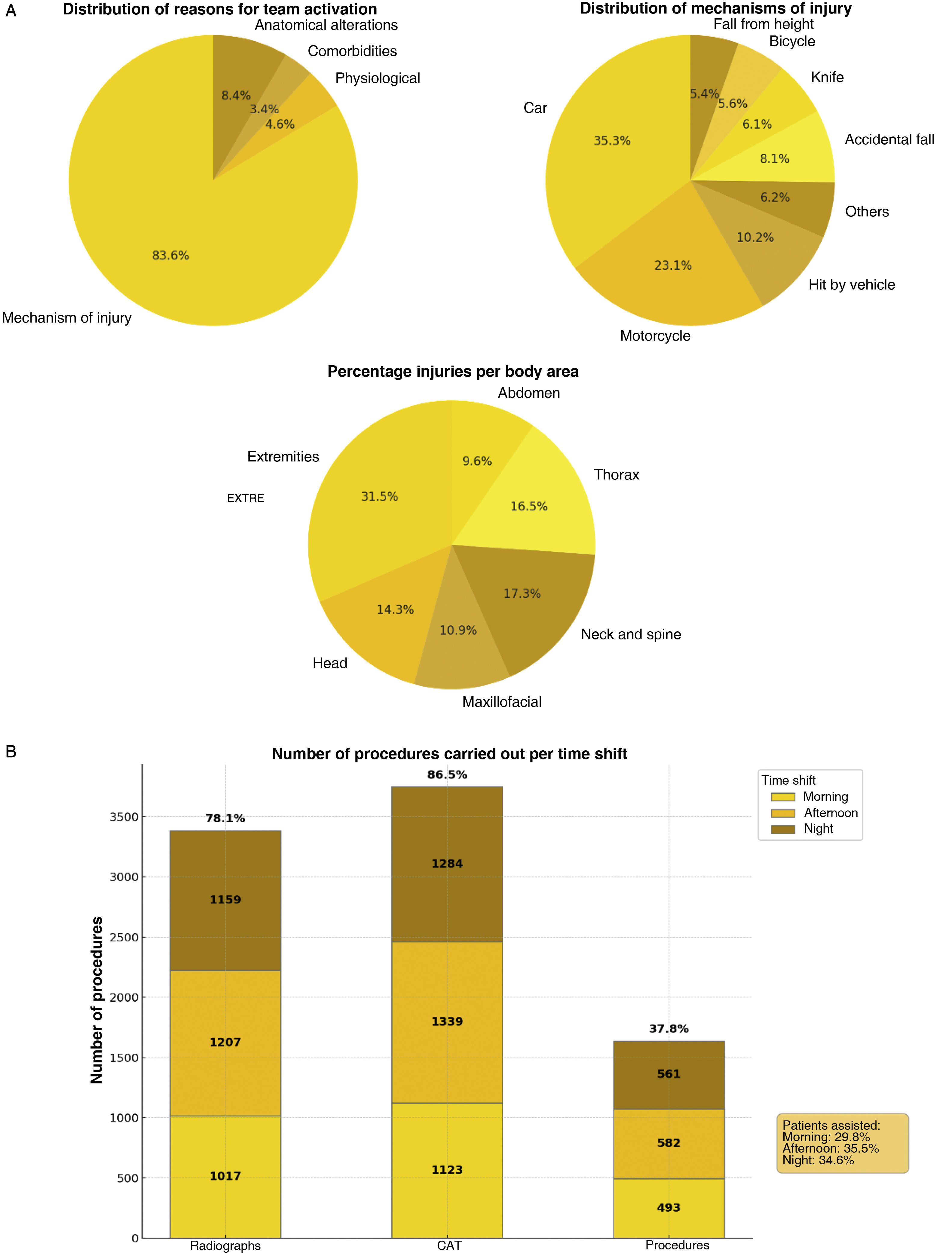
A total of 4332 patients were included, while 25 subjects had incomplete records and were thus excluded from the study. The median age was 36 years (interquartile range [IQR] 21), and 73% were male. The most common reasons for team activation and the mechanisms of injury are shown in Fig. 1, along with the body areas affected. Upon arrival, 93% of the patients had a Revised Trauma Score (RTS) of 12, with a median heart rate of 80 bpm (138), a median respiratory rate of 16 (3.5), and a score on the Glasgow Coma Scale (GCS) of 15 points in 92% of the cases. The care time window or shift and the imaging tests and procedures performed are shown in Table 1 in the Supplementary material. Of all the patients, 88% had an ISS < 8 and 3.61% had an ISS > 15. A total of 357 patients (8.6%) were admitted to the Intensive Care Unit (ICU), while the rest remained in the emergency department. The median actual length of stay was 53 minutes (33) compared to a calculated theoretical length of stay of 135 minutes (22). This difference was statistically significant (p < 0.001). Table 1 in the Supplementary material shows the variables and their relationship to above-median care times.
The theoretical care time was found to be significantly longer than the actual care time. In turn, care times greater than one hour were independently and significantly associated with the use of computed tomography, the indication for the procedure, and the number of body regions affected by the trauma. No association was observed with respect to variables such as patient age, gender, mechanism of injury, reason for team activation or care time shift. In contrast, the indication of radiographs and the use of sedation for other procedures were associated with care times of less than one hour. To date, no studies in our setting have assessed the resources assigned by the Departments of Intensive Care Medicine to the treatment of critical patients in the emergency care area. Likewise, there are no national descriptions of the care of potentially critical trauma patients, and thus no adequate comparisons can be made. Therefore, the value of this study is that it assesses the resources dedicated to the management of these patients in the emergency care setting. The time spent by the professionals is a valuable resource, and its knowledge can be a crucial management factor in monitoring programs and determining human resources. Furthermore, our study found significant differences between the theoretically estimated care times and the actual care times. Therefore, in order to avoid inaccurate estimates, it is important to record the different processes in an objective manner. We believe that the observed differences between the theoretical and the actual care times can be explained by factors such as protocolized care, coordination between teams and training, which result in shorter than expected patient care times. Limitations of the present study include its observational nature. In addition, a number of unaccounted for factors may have influenced the processes and patient care times. Mention also must be made of the influence of epidemiological and operating differences between centers. All this may affect future comparisons of the data and their extrapolation. In conclusion, we believe that the presence of specialized intensive care teams working in emergency care settings proves to be efficient, and that the systematic activity of these teams is useful for improving the quality of patient care.