Uterotonics are widely used as prophylactic and therapeutic drugs for uterine atony, the major cause of direct maternal mortality due to postpartum hemorrhage.1,2 Carbetocin [1-deamino-1-carba-2-tyrosine-(0-methyl)-oxytocin], a synthetic oxytocin analogue effective for treating and preventing post-partum hemorrhage, increases intracellular calcium, stimulates myosin phosphorylation and contraction in uterine smooth muscle cells; has an onset of action of 2min and a plasma half-life six to seven times longer than oxytocin. It can be administered by intravenous (IV) and intramuscular route. Despite its safety profile, chest tightness, palpitations and breathing discomfort are frequently reported after its administration,3,4,5 therefore prescription information and some reviews recommend caution when it is administered to patients with asthma or cardiovascular disease. Herein we report a case of near fatal bronchospasm and bradycardia after carbetocin administration.
A 22 years-old pregnant female, with a past history of a ruptured ectopic tubal pregnancy two years earlier and asthma diagnosed during the first trimester of her current pregnancy, was admitted with at 39-week pregnancy to the obstetric ward for an elective Cesarean-section, current medication were two puffs of dose metered inhaled albuterol on a per needed basis. Surgery was performed under regional anesthesia. Due to uterine hemorrhage after birth, a bolus of 100mcg of intravenous carbetocine was administered by intravenous infusion over 60s, 2min later, she presented sudden onset of dyspnea, wheezing, disseminated rash, hypotension and severe bradycardia – irresponsive to 1mg of intravenous atropine – that progressed to a complete cardiac arrest; four minutes of advanced cardiopulmonary resuscitation which included 1mg epinephrine was needed to restore pulse. After tracheal intubation severe wheezing and hypotension persisted, a single dose of 1.5mg/kg IV methylprednisolone and a norepinephrine drip were initiated. Bleeding stopped, so surgery was finished and the patient was transferred to the Intensive Care Unit (ICU).
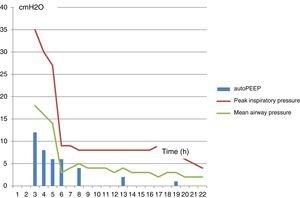
She was admitted to the ICU on mechanical ventilation, pulmonary mechanics reported high intrathoracic pressures with an auto-PEEP of 12cm H2O and a peak inspiratory pressure of 35cm H2O. Arterial blood gases reported: PCO2 91mmHg, PaO2 224mm Hg, pH 6.99, HCO3 19meq/L, SaO2 93. An ECG was obtained in sinus rhythm, with a heart rate of 95min without conduction abnormalities. The chest X-ray ruled out pneumothorax or hyperinflation. After analgesia, sedation, and paralysis with vecuronium, under controlled mechanical ventilation, ventilator settings were modified to reduce respiratory rate and increase expiratory time, which gradually lowered intrathoracic pressures and allowed us to stop vasopressors. Albuterol 2.5mg and ipratropium bromide 500 mcg were nebulized every 20min, hydrocortisone and a single dose of 2g of intravenous magnesium sulphate were also needed to finally totally overcome bronchospasm 3h after ICU admission. Sedation was stopped, the patient regained consciousness, and 20h after admission she was extubated and then discharged from the ICU (Fig. 1).
Asthma is estimated to occur in approximately 4% of pregnancies, frequently as a pre-existing disease, although sometimes – like in this case –, asthma may initially present during pregnancy. Prospective studies show that about 28% of pregnant asthmatics improve, 33% remain unchanged and nearly 35% deteriorate usually between 24 and 36 weeks of gestation. During labor and delivery only 10% of asthmatics report symptoms and less than 5% require treatment.6-8 Arrhythmias are an infrequent adverse event; however, alterations such as QT interval prolongation have been reported. These electrocardiographic alterations appear to be time and dose dependent.9
Pulmonary mechanics at admission to the ICU and without neuromuscular blockade did not correlate with the severity of the clinical presentation, which could be related to the way we perform clinical measurements of gas trapping, which rely in the assumption that through all expiration, all of the airways remain in communication with the proximal airway; but frequently in severe bronchoconstriction, all of them may not be in communication with the proximal airway due to heterogeneous distribution of bronchial edema, secretions and mucus plugging; therefore, flow, pressure or gas volume cannot be accurately measured from a noncommunicating airway. In addition, expiratory muscle contraction can elevate auto-PEEP without adding to dynamic hyperinflation, therefore for accurate measurements of auto-PEEP the patient should be relaxed.10,11
Although we did not find severe bronchospasm reported after carbotecin administration in our medical literature search; profound reversible intraoperative bradycardia during cesarean section has been reported recently as a novel occurrence associated with the use of carbetocin.5
Carbetocin prescription should have a clear indication and should be carefully individualized, based on individual medical and obstetric risk factors like prolonged labor, previous oxytocin administration, multiparity, multiple pregnancies, macrosomy, general anesthesia, and any condition that overdistends the uterus or interfere with effective uterine contraction.
Clinical medicine is full of uncertainties, ambiguous data, unusual presentations, and atypical therapeutic responses as this case, until we gather more data, and based on the approximately 4% prevalence of asthma during pregnancy, it seems wise to avoid carbetocin in asthmatic pregnant women, as well as in those with a past medical history that suggest bronchial hyperreactivity.
FinancingNo funding was received for this paper.
Conflict of interestNo conflict of interest for disclosure.
None.