Penetrating neck trauma is potentially fatal due to the high risk of damage to the airways and vascular structures.
The management of injuries, depending on the neck region that is affected, has been extensively covered since the 1970s. However, the advances made in imaging modalities make some authors advocate for replacing this classic management for an algorithm that includes performing more specific imaging modalities such as computed tomography (CT) scans, or angio-TC scans regardless of the affected area.
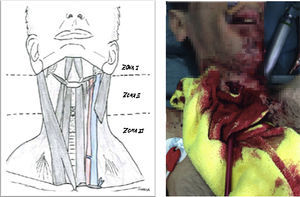
We present here the case of a 46 year-old-male with schizophrenia transferred to the ER after an attempted suicide. His most serious injuries were: injury caused by an arrow penetrating the neck region and injury caused by a bladed weapon penetrating the epigastrium (Fig. 1). The early management of the patient starts by performing one peripheral venous cannulation followed by resuscitating procedures using 500cc of physiological saline solution during the transfer. Upon arrival at the hospital, the patient was conscious and well-oriented, scored 14 points at the Glasgow Come Scale (GCS), was eupneic, his oxygen saturation levels reached 97 per cent, his blood pressure levels were around 120/90mmHg and his heart rate, 90bpm. The patient had a penetrating injury caused by an arrow that was still stuck to the anterior region of his neck, with scarce bleeding, crepitus to palpation, and one 2cm-long penetrating injury in the epigastrium caused by a bladed weapon without evisceration. There were no injuries in the patient's chest and the medical tests revealed no further alterations. There is presence of abdominal peritonism.
The blood sample tests show no alterations except for 14,800 leukocytes/mm3 with a percentage of neutrophils of 72 per cent, and hemoglobin levels of 11.3g/dl.
Since the patient was hemodynamically stable, one CT scan with IV contrast of the patient's neck, thorax, and abdomen was performed that showed the tip of the metallic projectile located in the airway (Fig. 1), but no damage to the blood vessels of the neck. In the abdomen there were bubbles of pneumoperitoneum and a moderate amount of dense free fluid both in left paracolic gutter and between loops.
Surgery was performed and one definitive airway through endotracheal intubation was established in the operating room. Afterwards, the arrow was removed from the neck region with carotid-jugular control, and any injuries at that level were completely ruled out. In the absence of bleeding from the large blood vessels of the neck, we proceeded to monitor the injury of the airway caused by the tip of the arrow in the second tracheal ring, using one 8-Fr non-fenestrated single cannula tube. Simultaneously, one exploratory laparotomy showed one discrete hemoperitoneum with bleeding of the gastroepiploic artery that was ligated at both ends, without any other major findings. After the surgery, the patient was referred to the intensive care unit where he recovered from surgery without any major complications. Six days after surgery the patient was decannulated and discharged from the hospital the very next day.
In order to be able to disclose the clinical case and publish any images related to such case, informed consent was required.
The initial algorithm that divided the neck into three areas and mandatorily required (Fig. 2) the performance of one endoscopy and one angiography in patients with injuries at areas II and III, and the surgical exploration of injuries located in the area II is known as “selective approach” and has remained in force for years.1 Little by little new studies are being published suggesting that patients without any clear signs of vascular or visceral damage could benefit from observational strategies.2 Thus, the selective management of injuries located in the area II has prevailed as the standard of care in asymptomatic patients.3
Although today we still do not have enough evidence, several studies advocate for managing this type of patients with protocols like the Advanced Trauma Life Support (ATLS) method that has proven it can reduce the rates of avoidable mortality, or potentially avoidable deaths of these patients in the hospital setting.4
In the case of a neck injury, the first assessment should include the impending or potential compromise of the airway. In the case of impending or potential compromise of the airway, the initial care should include the definitive control of such airway. In this case, and given the potential risk of the airway, the best time to establish one definitive airway would have been before the performance of the CT scan with the help of one videoscopic image capture device since the airway could have been suddenly compromised during the transfer or while establishing it, since the arrow could have been located exactly in the airway. In this case and given the patient had dyspnea, was conscious and that, in our setting, it is easy to perform CT scans, one CT scan with endovascular contrast of the patient's neck, thorax, and abdomen was performed. This circumstance is exceptional since usually the care recommended requires the initial definitive control of the airway.
The CT scan confirmed that the metallic edge of the projectile was located in the airway – one fundamental piece of information for surgical planning purposes.
When it comes to hemorrhagic control, in the first place, the surgical exploration of the neck region was performed that ruled out any damage to large blood vessels. Simultaneously, one exploratory laparotomy was performed due to the presence of free peritoneal fluid in the CT scan. Once the intra-abdominal hemorrhage was resolved, the tracheal injury was repaired. This approach is debatable since, when in suspicion of an abdominal hemorrhage, the first control maneuver should have been the exploratory laparotomy. However, the exploration of the neck in order to rule out damage to the large blood vessels should also be contemplated since a large number of neck injuries affecting vascular structures are misdiagnosed in the imaging modalities.5
In conclusion, when in the presence of penetrating neck injuries, it is vital to secure the airway even if it may be potentially compromised. Once the airway has been secured and after checking that there are no ventilation issues whatsoever, when in suspicion of bleeding or when bleeding is confirmed, it is mandatory to immediately control the hemorrhage.
Well-structured protocols like the ATLS method provide us with algorithms that help us during the management of patients with multiple traumatic injuries by establishing the course of action to be followed with polytraumatized patients.
FundingNo funding whatsoever was required for the completion of this project.
AuthorsVirginia Durán, MD, and Juan José Segura, MD followed the case, conducted the reference search, and wrote the manuscript.
Francisco López, MD, and Juan José Segura, MD performed the surgery and did the follow-up of the patient.
Amando Marchal, MD, and Juan José Segura, MD helped in the process of design and concepts.
Juan José Segura, MD, Felipe Pareja, MD, and Francisco López, MD did a critical review of the paper to the best of their ability.
All authors approved the final version of this paper.
Please cite this article as: Muñoz-Cruzado V, Segura-Sampedro JJ, Marchal Santiago A, López Bernal F, Pareja Ciuró F, Padillo Ruiz FJ. Traumatismo cervical penetrante por flecha en intento autolítico. Med Intensiva. 2017;41:379–381.