Incidence of post-intensive care syndrome at one month after hospital discharge in surviving critically ill COVID 19 patients and to identify associated factors.
DesignProspective cohort study.
SettingTwo multipurpose critical care units of the Araba University Hospital. Patients admitted to critical care units for severe acute respiratory failure secondary to COVID 19.
InterventionNone.
Variables of interestDemographic variables, length of stay, Charlson index, APACHE II, SOFA, days of mechanical ventilation, tracheotomy, delirium, tetraparesis of the critical patient, EuroQol 5D5L, Minimental Test.
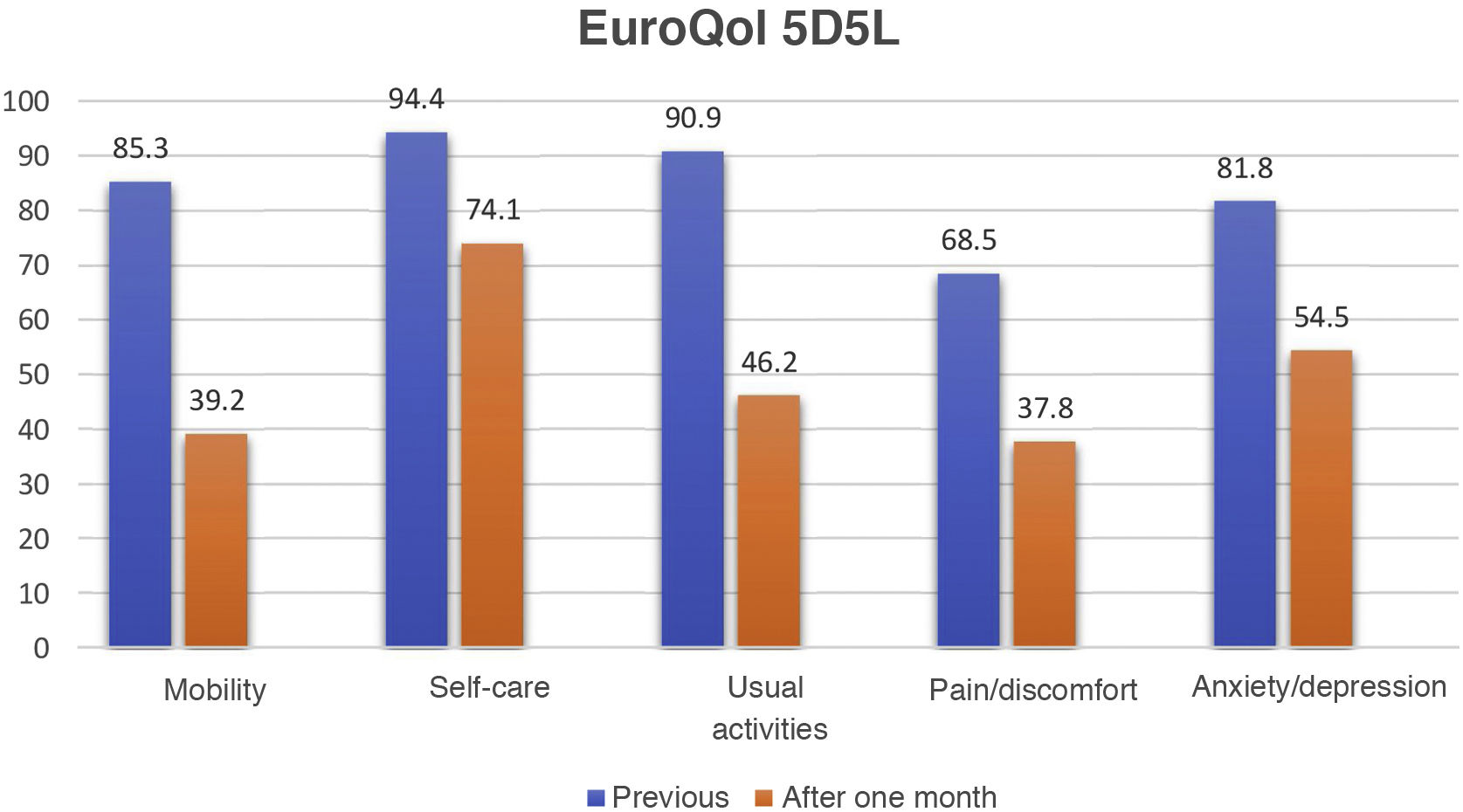
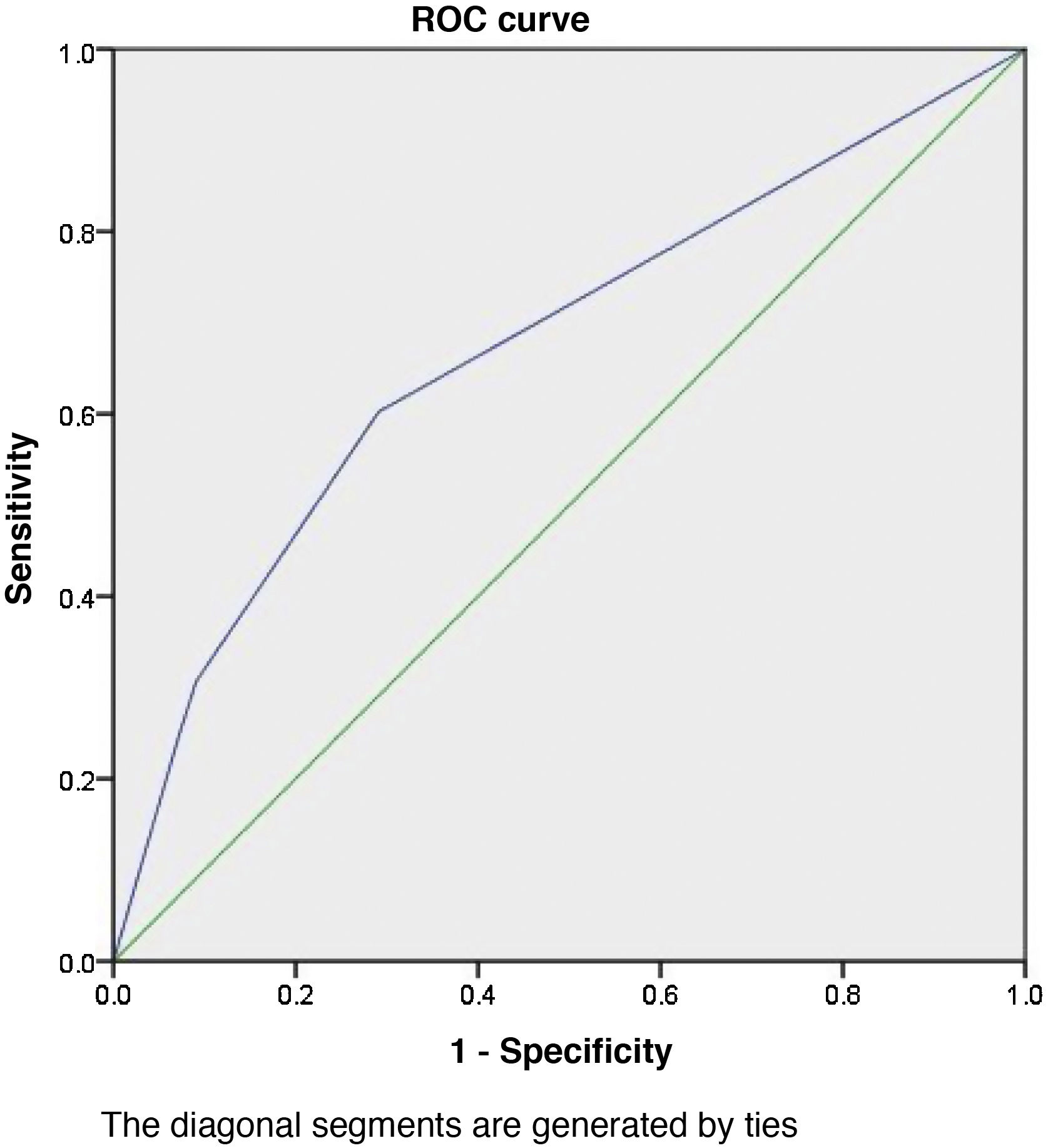
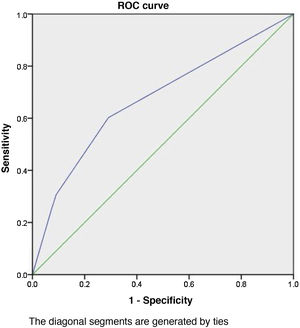
ResultsA deterioration in the EuroQol health index (HI) from 90.9±16.9 to 70.9±24.7 (p<0.001) was observed. The impairment of the five EuroQol domains is: mobility (46.1%), usual activities (44.7%), discomfort/pain (30.7%), psychological domain (27.3%) and self-care (20.3%). The 61.5% suffer a significant decrease in their health index. Multivariate analysis by logistic regression shows us that delirium (OR=3.01; 95%CI: 1.01–8.9; p=0.047) and tracheostomy (OR=2.37; 95%CI: 1.09–5.14; p=0.029) show association with drop in EuroQoL 5D5L SI. The area under the ROC curve of the model is 67.3%, with a confidence interval between 58% and 76%. The model is calibrated using the Hosmer-Lemeshow test (χ2=0.468; p=0.792). Only 1.2% of patients showed a score ≤ 24, clearly pathological, on the Folstein's Minimental Test.
ConclusionsDelirium and need for tracheostomy are associated with post-intensive care syndrome assessed by EuroQol 5D5L.
Incidencia del síndrome post-cuidados intensivos al mes del alta hospitalaria en pacientes críticos supervivientes de COVID 19 e identificar factores asociados.
DiseñoEstudio de cohortes prospectivo.
ÁmbitoDos unidades de críticos polivalentes del Hospital Universitario Araba. Pacientes ingresados en unidades de críticos por insuficiencia respiratoria aguda grave secundaria a COVID 19.
IntervenciónNinguna.
Variables de interésVariables demográficas, estancias, índice de Charlson, APACHE II, SOFA, días de ventilación mecánica, traqueotomía, delirio, tetraparesia del paciente crítico, EuroQol 5D5L, Minimental Test.
ResultadosSe objetiva un deterioro en el índice de salud (IS) del EuroQol que pasa de 90,9±16,9 a 70,9±24,7 (p<0,001). La afectación de los cinco dominios del EuroQol es de: movilidad (46,1%), actividades habituales (44,7%), malestar/dolor (30,7%), dominio psicológico (27,3%) y autocuidado (20,3%). El 61,5% sufren un descenso significativo de su índice de salud. El análisis multivariante mediante regresión logística nos muestra que el delirio (OR=3,01; IC95%: 1,01-8,9; p=0,047) y la traqueotomía (OR=2,37; IC95%: 1,09-5,14; p=0,029) muestran asociación con la caída en el IS del EuroQoL 5D5L. El área bajo la curva ROC del modelo es del 67,3%, con un intervalo de confianza entre el 58% y el 76%. Se calibra el modelo mediante el test de Hosmer-Lemeshow:(χ2=0.468; p=0.792). Solamente el 1,2% de los pacientes mostraban una puntuación ≤ 24, claramente patológica, en el Minimental Test de Folstein.
ConclusionesEl delirio y la necesidad de traqueostomía se asocian a síndrome post-cuidados intensivos evaluado mediante EuroQol 5D5L.
The pandemic caused by SARS-CoV-2 has resulted in an increase in the number of patients admitted to the Intensive Care Unit (ICU) due to acute respiratory distress syndrome (ARDS) secondary to COVID-19. Such patients suffer high mortality, with both physical and psychological sequelae which are currently beginning to be evaluated.1,2 Many of them present physical, cognitive and/or psychological deterioration,3 with incidences that vary greatly depending on the authors and the analyzed moment in time. These signs and symptoms conform what has been known for some years as “post-intensive care syndrome” (PICS).
As commented above, a broad variety of tools have been used to identify and quantify the signs and symptoms of this syndrome in its different facets. The present study uses a health-related quality of life (HRQoL) indicator – the EuroQol – to assess the degree of patient involvement. This tool allows the integral assessment of patient-perceived health status, with the application of a “health index” (HI), and is able to discriminate between the different domains evaluated by the instrument.
Specifically, the present study has three objectives: to quantify the incidence of PICS based on the variations of the HI; assess the degree of involvement of the 5 domains of the EuroQol 5D5L; and try to identify the factors associated with the deterioration observed in those patients that have survived COVID-19.
MethodsThe study was carried out at Hospital Universitario Araba (Vitoria-Gasteiz, Basque Country, Spain), which comprises two hospital centers: Santiago Apóstol and Txagorritxu. Since 1995, these centers each have a multipurpose ICU with 13 and 20 beds, respectively.
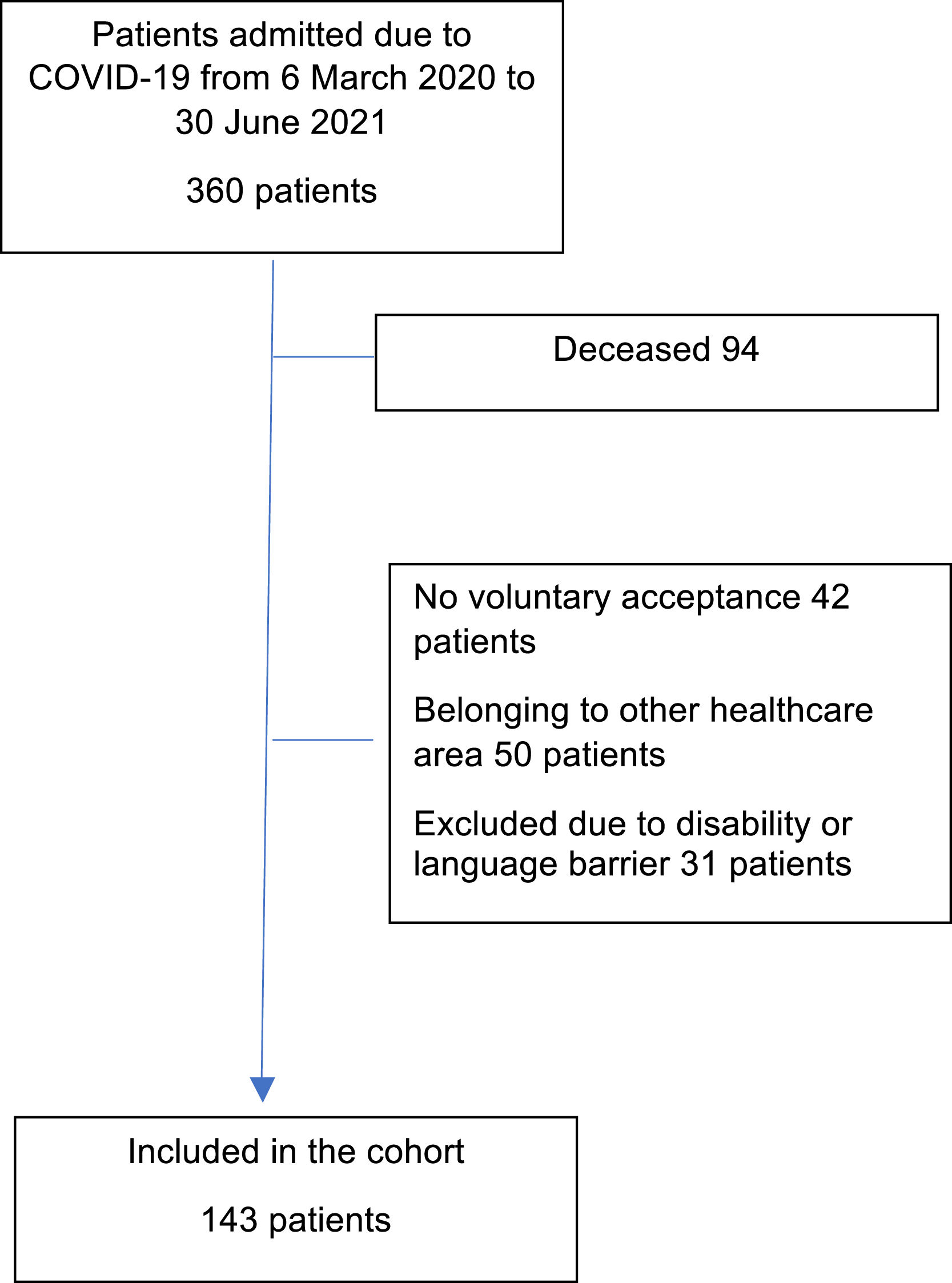
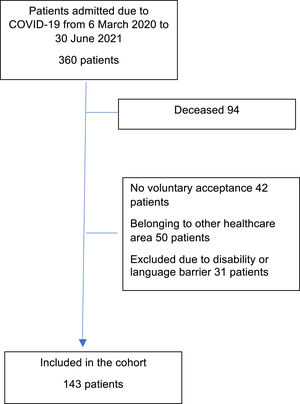
A prospective cohort design was adopted, including patients over 18 years of age who survived an ARDS episode secondary to COVID-19 and were admitted to our Units between 6 March 2020 and 30 June 2021. Patients with COVID-19 admitted for reasons other than secondary respiratory failure were excluded. The study was approved by the local Research Ethics Committee, and written informed consent was obtained from all the included patients.
Individuals that declined to participate in the study were excluded, as were those unable to give consent, patients in transit or belonging to other healthcare areas (since the evaluation was made on a face-to-face basis), and patients with language barriers complicating assessment.
We recorded demographic parameters, prior comorbidities with the Charlson index,4 ICU and hospital stay, severity indicators such as the APACHE II (Acute Physiological and Chronic Health Evaluation)5 and SOFA (Sequential Organ Failure Assessment),6 the presence of delirium diagnosed with the CAM-ICU,7 tetraparesis of the critical patient diagnosed from the Medical Research Council (MRC) Sum Score and defined as MRC<36 points, symmetrical strength loss and diminished osteotendinous reflexes,8 days of mechanical ventilation, and the need for tracheotomy.
The incidence of post-intensive care syndrome was evaluated using the EuroQol 5D5L,9–11 which contemplates 5 dimensions: mobility, self-care, usual activities, discomfort/pain and psychological domain (anxiety/depression). Each dimension is scored from 1 point (no limitation) to 5 points (total disability). The EuroQol allows quantification of health based on a visual analog scale (VAS) from 0 to 100 points (where 100=best health possible) and a Health Index (HI), standardized for the Spanish population. We considered PICS to imply a clinically significant worsening of HRQoL, defined as a 10% decrease in HI. The incidence of cognitive deterioration was evaluated by asking the patient or representing person whether he/she had noticed such deterioration, and if affirmative, we applied the Folstein Minimental test (MMT),12 which evaluates the following aspects based on a total score of 0–30 points: orientation in time (0–5), orientation in space (0–5), fixation (0–3), calculation (0–5), recall (0–3) and language (0–9). A total score of ≥ 27 was considered normal, while 26−25 points was rated as doubtful, 12–24 pathological, and < 12 points was taken to indicate dementia.
The assessment was made using a face-to-face interview, of a multidisciplinary nature, with the participation of a psychologist, one month after discharge from the hospital. The patient was asked to rate his/her HRQoL one month before admission due to COVID-19 and at the time of the interview, using the hetero-applied EuroQol.
In assessing the possible factors involved in the observed deterioration of the scores, the Student t-test for independent samples was used in application to quantitative variables, while the chi-square test was used in the case of qualitative variables. We selected those variables found to be statistically significant (p<0.05) or with p<0.150 for the univariate logistic regression analysis. In turn, those variables selected by the univariate analysis (p<0.05) were entered in the multivariate logistic regression analysis. The final predictive model was established using the backward stepwise (Wald) method, incorporating those variables that were seen to remain statistically significant. The calibration of the model was based on the Hosmer-Lemeshow test, and its discriminating capacity was analyzed from the area under the receiver operating characteristic (ROC) curve. The comparison of related means was used to analyze the variations in VAS score and the EuroQol HI. Data analysis was performed using the SPSS version 23 statistical package and R version 4.1.2.
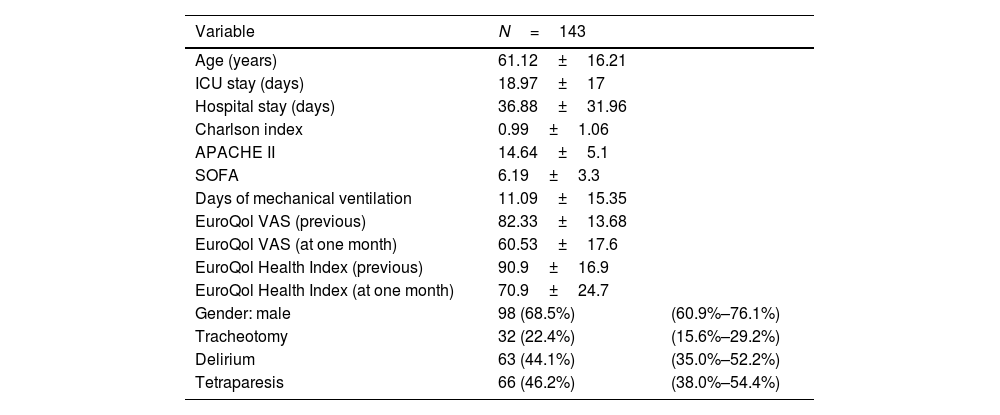
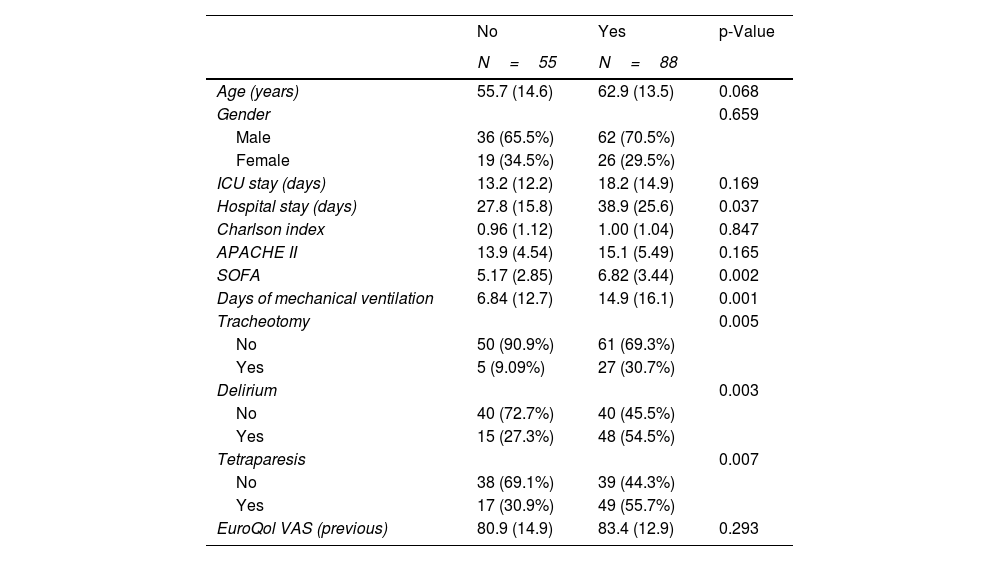
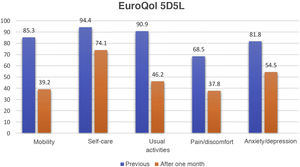
ResultsDuring the period between 6 March 2020 and 30 June 2021, a total of 360 patients with severe ARDS secondary to COVID-19 were admitted to our Units. After applying the exclusion criteria, a total of 143 patients, representing 53.76% of the overall survivors and 77.3% of the eligible subjects, were included in the study (Fig. 1). The characteristics of the cohort are described in Table 1. The comparison of related samples revealed statistically significant reductions in the scores one month after discharge in relation to the values recorded prior to admission. Specifically, the HI decreased from 90.9±16.9 to 70.9±24.7 (p<0.001), while the VAS score decreased from 82.33±13.7 to 60.53±17.6 (p<0.001). On comparing the different domains of the EuroQol (Fig. 2), the greatest decreases in absolute terms among the patients without limitations corresponded to mobility (46.1%), followed by usual activities (44.7%), pain/discomfort (30.7%) and anxiety/depression (27.3%). The least affected domain was self-care, with a decrease of 20.3%. We also found that 88 patients (61.5%) presented a decrease in HI of ≥ 10%, considered to be clinically significant. As can be seen in Table 2, these patients had a longer hospital stay, a higher SOFA score, more days of mechanical ventilation, and a higher incidence of tracheostomy, delirium and tetraparesis of the critical patient.
Descriptive and clinical data of the study cohort.
| Variable | N=143 | |
|---|---|---|
| Age (years) | 61.12±16.21 | |
| ICU stay (days) | 18.97±17 | |
| Hospital stay (days) | 36.88±31.96 | |
| Charlson index | 0.99±1.06 | |
| APACHE II | 14.64±5.1 | |
| SOFA | 6.19±3.3 | |
| Days of mechanical ventilation | 11.09±15.35 | |
| EuroQol VAS (previous) | 82.33±13.68 | |
| EuroQol VAS (at one month) | 60.53±17.6 | |
| EuroQol Health Index (previous) | 90.9±16.9 | |
| EuroQol Health Index (at one month) | 70.9±24.7 | |
| Gender: male | 98 (68.5%) | (60.9%–76.1%) |
| Tracheotomy | 32 (22.4%) | (15.6%–29.2%) |
| Delirium | 63 (44.1%) | (35.0%–52.2%) |
| Tetraparesis | 66 (46.2%) | (38.0%–54.4%) |
Qualitative variables are reported as percentages with the corresponding 95%CI, and quantitative variables are reported as the mean±standard deviation (SD).
Bivariate analysis according to the decrease in Health Index (≥10%).
| No | Yes | p-Value | |
|---|---|---|---|
| N=55 | N=88 | ||
| Age (years) | 55.7 (14.6) | 62.9 (13.5) | 0.068 |
| Gender | 0.659 | ||
| Male | 36 (65.5%) | 62 (70.5%) | |
| Female | 19 (34.5%) | 26 (29.5%) | |
| ICU stay (days) | 13.2 (12.2) | 18.2 (14.9) | 0.169 |
| Hospital stay (days) | 27.8 (15.8) | 38.9 (25.6) | 0.037 |
| Charlson index | 0.96 (1.12) | 1.00 (1.04) | 0.847 |
| APACHE II | 13.9 (4.54) | 15.1 (5.49) | 0.165 |
| SOFA | 5.17 (2.85) | 6.82 (3.44) | 0.002 |
| Days of mechanical ventilation | 6.84 (12.7) | 14.9 (16.1) | 0.001 |
| Tracheotomy | 0.005 | ||
| No | 50 (90.9%) | 61 (69.3%) | |
| Yes | 5 (9.09%) | 27 (30.7%) | |
| Delirium | 0.003 | ||
| No | 40 (72.7%) | 40 (45.5%) | |
| Yes | 15 (27.3%) | 48 (54.5%) | |
| Tetraparesis | 0.007 | ||
| No | 38 (69.1%) | 39 (44.3%) | |
| Yes | 17 (30.9%) | 49 (55.7%) | |
| EuroQol VAS (previous) | 80.9 (14.9) | 83.4 (12.9) | 0.293 |
Comparison of qualitative variables with the chi-square test, and of quantitative variables with the Student t-test. The following present p<0.150 and are thus selected for the univariate analysis: age, hospital stay, SOFA, days of mechanical ventilation, tracheotomy, delirium and tetraparesis of the critical patient.
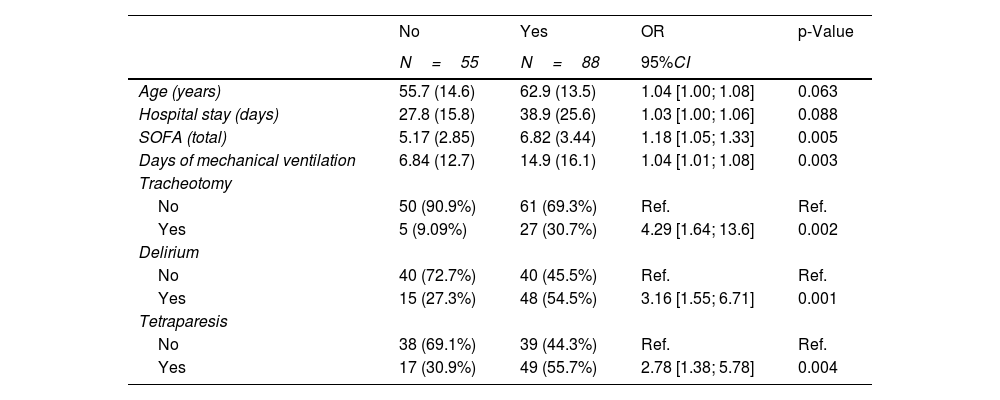
In Table 3, the univariate logistic regression analysis shows the SOFA score, days of mechanical ventilation, tracheotomy, delirium and tetraparesis of the critical patient to be associated with a worsening of the HI of ≥ 10%. In turn, the multivariate logistic regression analysis found delirium (OR=3.01; 95%CI: 1.01–8.9; p=0.047) and tracheotomy (OR=2.37; 95%CI: 1.09–5.14; p=0.029) to be correlated to worsened HRQoL as assessed by the EuroQol.
Univariate analysis according to the decrease in Health Index (≥10%).
| No | Yes | OR | p-Value | |
|---|---|---|---|---|
| N=55 | N=88 | 95%CI | ||
| Age (years) | 55.7 (14.6) | 62.9 (13.5) | 1.04 [1.00; 1.08] | 0.063 |
| Hospital stay (days) | 27.8 (15.8) | 38.9 (25.6) | 1.03 [1.00; 1.06] | 0.088 |
| SOFA (total) | 5.17 (2.85) | 6.82 (3.44) | 1.18 [1.05; 1.33] | 0.005 |
| Days of mechanical ventilation | 6.84 (12.7) | 14.9 (16.1) | 1.04 [1.01; 1.08] | 0.003 |
| Tracheotomy | ||||
| No | 50 (90.9%) | 61 (69.3%) | Ref. | Ref. |
| Yes | 5 (9.09%) | 27 (30.7%) | 4.29 [1.64; 13.6] | 0.002 |
| Delirium | ||||
| No | 40 (72.7%) | 40 (45.5%) | Ref. | Ref. |
| Yes | 15 (27.3%) | 48 (54.5%) | 3.16 [1.55; 6.71] | 0.001 |
| Tetraparesis | ||||
| No | 38 (69.1%) | 39 (44.3%) | Ref. | Ref. |
| Yes | 17 (30.9%) | 49 (55.7%) | 2.78 [1.38; 5.78] | 0.004 |
The area under the ROC of the model was 67.3%, with a confidence interval between 58–76% (Fig. 3). The Hosmer-Lemeshow test (chi-square=0.468; p=0.792) showed a good correlation between the prediction of the model and the actual values observed.
With regard to the assessment of cognitive condition, 28 patients (19.6%) reported a degree of cognitive impairment, particularly in the form of concentration difficulties or frequent memory lapses. Upon evaluation with the Minimental test (MMT), only two of these patients (1.2%) yielded a clearly pathological score of ≤ 24.
DiscussionAlthough most of the patients admitted to our Units as a result of ARDS secondary to COVID-19, currently known as COVID-19 associated acute respiratory distress syndrome (CARDS),13 survive, there is now abundant evidence that these individuals suffer a high incidence of PICS. The incidence varies greatly, though the reported figures generally range between 51–80%.1,14,15
Different authors agree that PICS is characterized by physical, cognitive and emotional deterioration, though in the case of worsened health condition no threshold beyond which the disorder should be regarded as clinically significant has been established. Although the EuroQol is designed to assess perceived HRQoL, we decided to use it because it moreover also allows an integral assessment of PICS, as postulated by authors such as Major et al.,9 Busico et al.10 and recently also Maley et al.,14 where this instrument has been used to evaluate physical activity. In addition, the 5L version of the tool has improved its sensitivity by lowering the ceiling effect of the 3L version. The results of the EuroQol afford a population standard for Spain, and the instrument constitutes a reference for establishing comparisons between groups of patients and the general population, in addition to facilitating follow-up of the evolution of patient health.11 In the absence of established thresholds, we consider that a 10% decrease in the Health Index (HI) could reflect clinically significant deterioration, based on the national health survey conducted in 2011-201211 and published by the Spanish Ministry of Health in 2014. The HI in the population of the Basque Country aged 55–65 years (the age range corresponding to our study cohort) was found to be 90.7, which is consistent with our own recorded figure of 90.9. In the 75–84 years of age group (20 years older), the index was 85 (i.e., a difference of 6.3%). On the other hand, the availability of a quantitative indicator facilitated the identification of factors associated with PICS. We are aware that the application of a scale on a retrospective basis with respect to the situation before the disease may result in recall bias, but the fact that the EuroQol was hetero-applied and that emphasis was placed during the interview on differentiating between the two evaluated moments overcame this possible bias.
A total of 61.5% of our patients showed a decrease in the HI of the EuroQol of at least 10% with respect to their previous situation. It is difficult to compare the different published studies in relation to PICS and thus establish the true dimensions of the problem. In our opinion, this is because the instruments used for assessment, and the timepoints involved, were different. As an example, the COMEBAC study1 used the SF-36, and the first assessment – made by telephone – took place 3–4 months after hospital discharge. Latrónico et al.15 likewise used the SF-36, but at three months after ICU discharge, and assessment in this case was conducted on a face-to-face basis. In turn, Marra et al.16 used the Katz ADL three months after hospital discharge, and Maley et al.14 administered the EuroQol 5D at 6 months post-hospital discharge, by telephone. In any case, the magnitude of the problem makes it necessary to identify risk factors for the development of PICS on which to intervene in order to facilitate both primary and secondary prevention.2,17,18 Among the 5 domains assessed by the EuroQol, the highest percentages of patients with some limitation corresponded to the domain of mobility, followed by usual activities and pain. However, one month after hospital discharge, 74.1% of the patients continued to show no limitations in relation to self-care. These data are consistent with those of other studies in which motor activity was found to be the most affected domain, though not to the point of causing the majority of patients to become dependent for basic activities of daily living.1,15,19,20 The fifth dimension evaluated by the EuroQol refers to anxiety/depression, which is one of the dimensions affected in PICS. Specifically, 18.2% suffered anxiety/depression before admission. We did not discard patients with prior psychiatric problems, since the availability of prior assessment would allow us to detect the changes after patient discharge from the ICU. Nevertheless, this was the least affected domain, after self-care, with a 27.3% increase in the number of affected patients one month after hospital discharge. These figures are consistent with those published by Davydow et al.21 in a systematic review, or by Premraj et al.22 in a meta-analysis, but far lower than those reported by Maley et al.,14 where the incidence of PCS reached 80% - though in this case all the patients had required mechanical ventilation. Taking into account that the EuroQol considers symptoms of anxiety or depression and not a diagnosis of these conditions, we may be overestimating the seriousness of the problem.
On analyzing the possible factors associated with an increased risk of HI worsening ≥ 10%, a higher SOFA score, longer duration of mechanical ventilation, tracheotomy, delirium and tetraparesis of the critical patient were seen to be associated with an increased probability of worsened HRQoL as assessed by the HI.
In the multivariate model, tracheotomy and delirium were respectively associated with a three and over two times greater risk of significantly worsened quality of life, one month after hospital discharge.
In our Units, most of the tracheotomies (84.3%) were percutaneous – the surgical procedures being restricted to anatomical requirements – and the patients were moved to the hospital wards following decannulated in the Unit, for safety reasons. Therefore, we believe that tracheotomy in itself does not account for an increased risk of PICS but rather for what it implies. On one hand, in our cohort the tracheotomized patients were characterized by very prolonged mechanical ventilation: 35.65±12.7 days versus 4.9±6.7 days among the non-tracheotomized individuals. On the other hand, this difference in days of mechanical ventilation very likely implies more days of sedation, immobilization, healthcare-related infections, etc., resulting in increased deterioration and thus implying slower patient recovery.
Delirium, characterized by inattention accompanied by disorganized thought or altered level of consciousness, showed an incidence intermediate within the range published in the literature, even though this was a group of patients presenting most of the known risk factors, prolonged mechanical ventilation, prolonged sedation, and the use of benzodiazepines.23,24 Our study supports the high incidence of delirium in ARDS due to COVID-19 and the hypothesis that delirium is clearly associated with PICS and to consequent worsening of HRQoL. Because of its complexity, in our study the duration of delirium and its possible association with the use of benzodiazepines were not recorded.
Another evaluated dimension was cognitive deterioration as one of the aspects considered in PICS. Different authors have reported incidences ranging widely from 16 to 80%,15,25 and some studies have found it to persist after one year.2,25 Several risk factors have been identified, including delirium during ICU stay, prior cognitive deterioration, sepsis and ARDS.25–28 It is known that SARS-CoV-2 affects both the central and the peripheral nervous system, giving rise to a broad spectrum of neurological conditions,29,30 though it may be difficult to establish whether deterioration is a consequence of COVID-19 or of PICS itself, independently of the underlying cause.31 In our cohort, although 19.6% of the patients reported some degree of cognitive deterioration particularly in the form of frequent memory lapses and concentration difficulties, application of the MMT only found two patients (1.2%) to have a clearly pathological score (≤24 points). Such “memory lapses” and “concentration difficulties” did not pose a serious handicap for leading a normal life. The tool used possibly has low sensitivity in detecting mild cognitive alterations, and consequently may underestimate the seriousness of the problem.
It can be concluded that most patients who survive ARDS secondary to COVD-19 present PICS that is reflected in worsened HRQoL, as assessed by the EuroQol — particularly in the domains of mobility, usual activities and pain, and less so in relation to emotions or self-care. Such deterioration in turn is associated with the development of delirium and the need for tracheotomy during admission to the ICU.
In relation to what has been published on this issue to date, we consider that our study contributes to the usefulness of the HI of the EuroQol and the identification of factors associated with this syndrome, and also highlights the need to work on the diagnosis, quantification and identification of risk factors allowing us to prevent PICS and facilitate posterior patient monitoring and treatment.
Financial supportFunding was received through the Convocatoria Intramural Extraordinaria for Covid-19 projects of the Fundación Vital Fundazioa – Bioaraba.
Author contributionsAll the authors contributed to data acquisition, critical review of the intellectual content of the article and final approval of the submitted version of the manuscript. S. Iribarren, A. Vallejo and R. Barreira were in charge of study conception and design. C. Bermúdez and S. Iribarren carried out data analysis and interpretation.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Funding was received through the Convocatoria Intramural Extraordinaria for Covid-19 projects of the Fundación Vital Fundazioa – Bioaraba.