The nutritional needs of the critical patient have not been clearly established, but are known to vary depending on the phase in which the disease process happens to be. In this regard, the early phases of critical disease are characterized by intense catabolism, followed in a later phase by anabolic activity during patient recovery. Knowing the optimum caloric and protein supply in the critical patient would require the conduction of randomized studies involving large numbers of patients. The decision regarding the amount of calories and proteins to be supplied is often based on the clinical judgment and experience of the prescribing physician, fundamentally taking into account the degree of stress and malnutrition of the patient.
What are the caloric needs of the critical patient and what method should we use to calculate them?The reference method for measuring energy expenditure is indirect calorimetry (IC), which uses the Weir equation to assess resting energy expenditure from the measurement of oxygen consumption and the production of CO2. However, its utilization is limited by cost considerations, the need for trained staff, and technical difficulties such as limitations imposed by air leakage, the need for high FiO2 levels, the use of renal replacement techniques and other problems which cause IC not to be used on a routine basis.1 The measurement of energy expenditure with IC is necessary in order to avoid under- and overfeeding, which can cause morbidity additional to that associated with the hypermetabolic state,2 particularly in patients with increased stress, malnutrition, obesity or burns, in which a poor correlation is observed with the energy needs calculated by means of predictive formulas. In a study comparing calculation of the energy supply with IC versus a formula (25 kcal/kg/day), the authors recorded a greater caloric and protein supply in the group of patients guided by IC, with a tendency towards lower in-hospital mortality.3
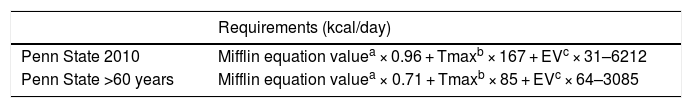
When IC is not available, the use of predictive formulas has been suggested, such as the Harris-Benedict formula, Mifflin-St. Jeor equation or the Penn State formula (Table 1). The latter is advocated in patients subjected to mechanical ventilation (MV), and a study involving 202 critical patients subjected to MV has found it to offer the best correlation to IC.4 Another option is the use of simplistic formulas based on body weight, which recommend between 20–30 kcal/kg/day; however, as has been mentioned, no strong correlation has been found between the requirements calculated with formulas and those measured by IC, since there are different metabolic characteristics and changes in body composition that can modify energy expenditure. In a recent study involving 1440 patients and 3573 IC measurements, Zusman et al. demonstrated great deviations and a lack of correlation between different formulas and energy expenditure as measured by IC.5
Penn State formula for the calculation of caloric requirements.
| Requirements (kcal/day) | |
|---|---|
| Penn State 2010 | Mifflin equation valuea × 0.96 + Tmaxb × 167 + EVc × 31–6212 |
| Penn State >60 years | Mifflin equation valuea × 0.71 + Tmaxb × 85 + EVc × 64–3085 |
Females: 10 × weight (kg) + 6.25 × height (cm) – 5 × age (years) – 161.
Classically, it has been considered that a caloric supply below the requirements in the first week of critical disease could prove harmful. However, there is now some evidence that this approach could even offer benefits for the patient. A retrospective observational study found the administration of 70% of the requirements as determined by IC to be associated to lesser patient mortality compared with individuals that received a caloric supply above or below this percentage.6 A meta-analysis involving critical patients receiving enteral nutrition (EN) found no differences in terms of mortality between those receiving all their caloric requirements versus those presenting hyponutrition.7 In this same line, a randomized trial comparing a hypocaloric (12 kcal/kg/day) and hyperproteic diet (1.4 g/kg/day) versus a normocaloric (20 kcal/kg/day) and hyperproteic diet (1.4 g/kg/day) likewise failed to detect differences between both groups of patients in terms of the outcomes—with the exception of a decrease in insulin requirements in the hypocaloric group.8 A possible explanation for these results has been offered by authors such as Preiser, who consider that the energy needs in the early phases of critical illness are practically covered by endogenous energy production; as a result, an added exogenous supply would produce hypernutrition or overfeeding, with its associated deleterious effects, due to non-suppression of endogenous energy production through the supply of such exogenous substrates.9 Furthermore, exogenous nutrient supply would inhibit autophagia—a mechanism that favors damaged tissue recovery.
However, some investigators have reported a decrease in mortality with a supply closer to the calculated requirements, from the early stages of disease, and particularly in patients with previous malnutrition. In a study of the effect of the amount of calories and proteins supplied in the acute phase of the disease, among septic patients subjected to mechanical ventilation and with EN, Elke et al. concluded that an increase of 1000 kcal, as well as of 30 g of protein daily, with respect to the averages obtained (14.5 kcal/kg/day and 0.7 g/kg/day, respectively), is associated to lesser patient mortality (odds ratio [OR] 0.61; 95% confidence interval [95%CI], 0.48–0.77; P < 0.001) and to a greater number of MV-free days (2.81 days; 95%CI, 0.53–5.08; P = 0.02).10
Based on the recommendations of experts, a reasonable caloric supply in the first week of critical illness would be about 70% of that calculated by IC or between 15–20 kcal/kg/day, particularly in the absence of previous malnutrition. Once the acute phase has been left behind, the recommendation would be to supply about 25 kcal/kg, increasing this to 30–35 kcal/kg body weight (b.w.) in the anabolic phase, once the inflammatory situation of the patient has been resolved.
With regard to the patient body weight to be entered in the formulas, it is advisable to use that recorded immediately before injury, since the current weight may exhibit broad variations secondary to initial resuscitation.
What are the requirements and what type of proteins should be administered to the critical patient?It has been demonstrated that caloric supply to the critical patient, particularly in the form of EN, is suboptimal—covering less than 70% of the caloric target or objective according to most studies. This in turn is accompanied by a low protein supply, in most cases of less than 0.8 g/kg body weight.11 Such a supply falls short of the minimum daily requirements of a healthy individual, resulting in protein deficits in patients with increased needs, since proteins are the key macronutrients required for wound healing, immune function and the maintenance of muscle mass. Such a low protein supply could explain the contradictory results of the different studies, independently of whether the caloric supply is low or close to meeting the energy requirements. A multicenter observational study of over 2800 patients classified according to stay (>4 or >12 days) reported lesser mortality among those individuals in both groups that received at least 80% of their protein requirements.12 A posterior analysis of the same group of patients moreover assessed the relationship between mortality and the energy and protein supply, and nutritional risk (high or low) as measured by the NUTRIC score—concluding that a greater protein and caloric supply affords better outcomes, particularly in patients at increased nutritional risk and a longer stay in the Intensive Care Unit (ICU).13 Another prospective cohort study carried out by Allingstrup et al. reported lower mortality in those patients that received an increased protein supply, independently of the energy supply they received.14 Likewise, another study involving critical patients subjected to mechanical ventilation found that a caloric and protein supply close to meeting the requirements reduces patient mortality versus patients that only achieve an adequate caloric supply.15
Following this tendency towards an increased protein supply, and since no randomized studies have evaluated different doses adjusted to an adequate caloric supply, the consensus-based recommendation is to perform the calculation with formulas fundamented on usual body weight, seeking to supply between 1.2–2 g/kg/day of proteins, which could be raised to 2.5 g/kg/day in patients with important losses, such as burn victims or individuals subjected to renal replacement therapy.16
What are the requirements and what type of carbohydrates should be administered to the critical patient?Carbohydrates remain the main energy source and represent approximately 50% of the total energy requirements. In critical patients it is advisable to maintain normoglycemia (approximately 150 mg/dl), avoiding strict glycemic control (80–110 mg/dl) due to the increased risk of hypoglycemia and mortality. At present, the target is a glycemia level of 150 mg/dl, above which insulin treatment should be started to keep the blood glucose levels below 180 mg/dl.17 In 2014, Kalfon et al. published a multicenter study comparing monitored strict glycemic control versus conventional control. The authors observed no decrease in mortality after 90 days in the strict control group, though the patients in this group suffered frequent and severe hypoglycemic episodes.18
Stress hyperglycemia is common in critical patients, even in those without diabetes, and is attributable to a series of factors such as the release of stress hormones, the use of certain drugs such as corticosteroids, increased insulin resistance and the release of inflammatory mediators as in sepsis. It therefore may be advisable to use formulas with carbohydrates characterized by a low glycemic index, incorporating non-hydrolyzed starches, oligosaccharides such as maltodextrins, polyols (maltitol) or disaccharides such as isomaltulose.19
The source of carbohydrates in parenteral nutrition (PN) is glucose—which should be supplied in amounts of no more than 3.5 g/kg/day, in order to avoid the complications associated to excessive exogenous glucose administration.20
What are the requirements and what type of lipids should be administered to the critical patient?The administration of lipids in nutritional support should be contemplated with a view to avoiding essential fatty acid deficits. Lipid formulations moreover supply liposoluble vitamins and components that participate in cell membrane structure and function and in receptor activity, regulating eicosanoid synthesis and modulating the expression of genes involved in metabolic pathways and inflammatory mediators.
Critical illness is generally characterized by an inflammatory state accompanied by different metabolic disturbances, which in the case of lipids comprise hypertriglyceridemia, increased free fatty acids and a decrease in cholesterol and LDL and HDL lipoproteins secondary to a drop in lecithin-cholesterol-acyltransferase activity. Another common finding is a reduction in enteral fat absorption, increased lipolysis and a decrease in carnitine levels, giving rise to alterations in mitochondrial function and in fatty acid oxidation.21
The types of lipids provided in nutritional-metabolic support can influence and affect the inflammatory processes. The ω-3 fatty acids present in fish oil exert antiinflammatory effects; the ω-9 fatty acids contained in olive oil exert neutral action; and the ω-6 fatty acids present in soy and sunflower oil have proinflammatory effects22—hence the potential importance of the type of lipid used. In recent decades it has been suggested that mixtures of different fatty acids could reduce the proinflammatory effects of the ω-6 fatty acids contained in the standard emulsions and thus afford better outcomes among the critically ill. These strategies referred to the reduction of ω-6 fatty acids involve the formulation of mixtures of different oils comprising olive oil, fish oil, medium chain triglycerides and soy and sunflower oils. The studies published to date have yielded heterogeneous results. A meta-analysis conducted by Manzanares et al.23 concluded that strategies seeking to reduce ω-6 fatty acids could reduce mortality, days on mechanical ventilation and the duration of stay in intensive care—though further studies are needed to confirm this. In a later study, Grau-Carmona et al. investigated the effects of ω-3 fatty acids upon the prevalence of nosocomial infections and other clinical outcomes in surgical critical patients, observing a significant decrease in the number of nosocomial infections. However, no significant differences were recorded in terms of hospital stay, days on mechanical ventilation, or mortality.24 A more recent meta-analysis conducted by Kreyman et al., investigating the effect of mixtures enriched with fish oil in 6 studies involving critical patients, recorded the same results as in the study of Grau-Carmona et al., i.e., a decrease in nosocomial infections without a reduction in ICU stay. The authors concluded that these results need to be confirmed by further studies.25 A more recent trial by Donoghue et al. involved a randomized double-blind design with 75 critical patients comparing PN with a mixture of four fatty acids (30% soy, 30% medium chain fatty acids, 30% olive oil and 15% fish oil) versus a mixture containing 100% soy oil. The authors concluded that the mixture is safe and improves the ω-6/ω-3 ratio; however, no differences were observed in terms of different biochemical parameters, severity scores (SOFA), ICU stay or patient mortality.26
In view of the heterogeneity of the studied patients and mixtures, no generalized recommendations for critical patients may be made, though it can be affirmed that emulsions enriched with fish oil improve the ω-6/ω-3 ratio, which would have antiinflammatory effects.
Based on the recommendation of experts, the advised lipid dose is 0.7–1.3 g/kg/day or 25%–40% of the caloric supply, and should be reduced in cases where the plasma triglyceride levels are >400 mg/dl.27
What are the needs in terms of micronutrients (vitamins and oligoelements) and fiber in critical patients?Micronutrients are to be administered at doses at least large enough to avoid their deficiency. A supply of 1500 kcal of an EN formula usually suffices to cover the daily requirements, and the use of PN always requires the addition of vitamins and oligoelements. The needs in the critical patient have not been established and are based on the recommendations of experts.
The administration of supplements of certain micronutrients with antioxidant effects (vitamins C, E and A, copper, zinc and selenium) has not been shown to reduce the number of infections or the duration of admission.28,29
Benefit may be obtained from the administration of thiamine supplements, not only in alcoholic and malnourished patients but also in individuals with septic shock, critical burn victims, polytraumatized patients and in cases of heart failure or unexplained lactic acidosis. Furthermore, if the critical patient receives only PN, supplementing should last at least three consecutive days, with higher doses of thiamine.30
Anemia is common in the critical patient, due to the existence of real and functional iron deficiency. However, the administration of iron via the oral or intravenous route has not been shown to reduce the transfusion requirements or improve morbidity-mortality in the critically ill.31
The administration of fiber (soluble and insoluble in the same proportion) is recommended in all critical patients receiving enteral feeding support, provided it is not contraindicated (severe alterations in gastrointestinal motility or Clostridium difficile positivity), in amounts ranging from 10 to 20 g daily.32 The administration of fiber has been shown to prevent complications of and intolerance to the enteral diet, and forms part of the management of complications such as diarrhea.
Is permissive underfeeding indicated in the critical patient? When is trophic enteral nutrition indicated?There is important controversy referred to the utilization of permissive underfeeding, trophic EN and feeding close to the calculated requirements. While the older studies33,34 reported poorer outcomes among those patients in which an important energy debt was generated in the first days of their clinical course, more recent studies such as the EDEN,35 PERMIT36 and EPaNIC37 trials have evidenced no differences in outcomes on comparing permissive underfeeding with standard nutrition during the first week of the clinical course of the critical patient, versus a greater supply. A meta-analysis conducted by Marik and Hooper including two studies with trophic EN (20% of the caloric target) and four studies with underfeeding (49% of the target), compared with complete nutritional support (>70% of the target), found no differences in mortality, infections, duration of stay or days without mechanical ventilation.38 Another recent meta-analysis has reported similar findings, with improved outcomes in patients with moderate underfeeding versus those receiving more marked underfeeding and versus those with full coverage of the nutritional requirements.39
Since the data in support of one recommendation or other are contradictory, due to the heterogeneity of the patients included in the studies in terms of the degree of malnutrition and of metabolic stress, the most reasonable recommendation for malnourished or high nutritional risk critical patients would be to avoid underfeeding once the acute phase has been left behind. Probably, patients with a low catabolic level and in previous good nutritional condition could explain the results of those studies comparing hypocaloric nutrition versus normocaloric feeding, and would be the candidates for such underfeeding in the first days of the critical illness.40
The aim of trophic EN is to avoid intestinal atrophy. In a study of patients with respiratory failure, trophic EN administered during the first 6 days of feeding yielded the same outcomes as complete nutritional support in individuals at low or moderate nutritional risk.30 At present it is only possible to indicate trophic EN in patients at low nutritional risk, and not beyond the first week of the critical disease process.
How should the caloric/protein supply of micronutrients and fiber be adjusted in the hemodynamically unstable patient?The energy needs of hemodynamically unstable patients vary greatly, being more dependent upon a number of factors such as the level of catabolism, inflammatory status or associated organ dysfunction than on the hemodynamic situation in itself, and individualized nutritional management is required in such cases. Whenever possible, IC should be used to calculate the caloric needs. In a study carried out among 9 heart surgery patients with hemodynamic instability in which IC was used to determine the energy needs, the authors found a caloric target or goal of close to 25 kcal/kg/day in patients of this kind (presenting a body mass index [BMI] within normal limits) to have only a small margin of error with respect to the value as determined by IC. This target has been used as reference in later clinical studies.41–43 However, the mentioned result might not be applicable to other sub-populations of critical patients with hemodynamic instability, such as septic shock patients.
Therefore, on the basis of the above, it is presently not possible to establish significant differences in terms of the macro- and micronutrients requirements versus the recommendations established for critical patients in general.
In patients of this kind the main problem is to cover the caloric-protein needs via the enteral route alone37,38—with complementary PN being necessary in some cases.38
With regard to the provision of fiber, cases of non-occlusive intestinal ischemia have been reported after starting EN rich in insoluble fiber—though without clearly specifying the hemodynamic condition of the patients prior to onset of the complication.44 No clinical studies have compared different types of dietetic fiber in patients of this kind. Since this subgroup of critical patients is at high risk of non-occlusive mesenteric ischemia, it is advisable not to supply fiber in the early phases, and to administer it in soluble form when fiber is considered necessary.
How should the caloric/protein supply of micronutrients and fiber be adjusted in the obese critical patient?Obese critical patients have a greater risk of suffering complications, conditioned to their BMI, but this has not been shown to be associated to increased mortality, except in individuals with extreme BMI values.
Overfeeding has a negative impact upon the outcome of critical patients in general, though it is among obese patients where the administration of hypocaloric and hyperproteic diets have shown outcomes equal to or even better than when normocaloric and hyperproteic diets are provided.45 Dickerson et al. compared hyper- and hypocaloric diets, with a hyperproteic supply in both groups, and found no differences in terms of nitrogen balance. Nevertheless, the authors recorded a decrease in the duration of antibiotic treatment, ICU and hospital stay, and mechanical ventilation.46 In these patients, which often also have other concomitant problems such as hyperglycemia and hypertriglyceridemia, these feeding regimens may be of help, facilitating improved metabolic control and ensuring net proteic anabolism or a reduction in negative nitrogen balance in the critical patient.
It is advisable for the caloric requirements to be estimated by means of IC, since in patients of this kind the predictive equations may generate greater error.47 In obese patients subjected to mechanical ventilation and in the absence of IC, the Penn State formula is recommended, with application of its modified version in patients over 60 years of age.42
Based on the mentioned previous studies, it is advisable for nutrition of the obese patient to be hypocaloric, covering about 50%–70% of the energy requirements (in simplistic terms, 14 kcal/kg current body weight/day or 22–25 kcal/kg ideal body weight/day), and hyperproteic (2–2.5 g proteins/kg ideal body weight/day)—adjusting the amounts in order to secure an acceptable nitrogen balance.48,49
In the same way as with the rest of critical patients, adequate glycemic control is indicated—the objective being <150 mg/dl.50 Likewise, EN with fiber is recommended, as it also facilitates glycemic control, among other benefits. Monitoring of blood glucose and lipid profile is necessary, with the control of hypercapnia, water overload and fatty liver, which are often already present before admission to the ICU. With regard to lipids, the recommendations are the same as in the case of the rest of critical patients.
It is advisable to quantify iron, folate, zinc, copper, selenium and vitamins B12 and D,51 since these patients often have vitamin deficits, particularly if they have undergone bariatric surgery.
How should the caloric/protein supply of micronutrients and fiber be adjusted in the patient acute renal failure?In relation to the energy requirements, acute kidney injury (AKI) in itself does not imply differences in management with respect to the rest of critical patients, though it must be noted that increased AKI results in greater caloric requirements; frequent re-evaluation is therefore needed.52 Indirect calorimetry should be used whenever possible, though this technique has limitations in the case of patients requiring continuous renal replacement therapy (CRRT).53 In this respect, the use of bicarbonate-containing solutions within the system (with consequent modification of the pCO2 values), or the changes in body temperature secondary to the use of these techniques, may alter determination of the energy expenditure of the patient. Occult energy provision through replacement fluids (citrate, glucose, lactate, etc.) must be monitored in order to avoid overfeeding.46 This is particularly applicable to citrate, used for regional anticoagulation of the system, and which may supply as much as 250–400 kcal during a full day of CRRT. On the other hand, greater severity of AKI, particularly if it implies increased intensity of replacement therapy (use of high volume techniques and high permeability filters), requires an increase in protein supply to 1.5–2.5 g/kg/day in order to compensate losses through the system and losses associated to hypercatabolism.54 However, the impact of this measure upon clinically relevant parameters has not been established in interventional studies involving patients of this kind. There is no evidence to recommend a specific amino acid profile in the protein supply.55 In accordance with the above, the use of renal failure-specific formulas (which are usually hypercaloric and hypoproteic) is not advised on a routine basis in critical patients with AKI, particularly in those with greater hypercatabolism or with a need for CRRT.
With regard to micronutrients and fiber, very few high quality studies are available. In patients subjected to CRRT, there have been reports of significant phosphorus, magnesium, selenium and water-soluble vitamin losses. Supplementing is therefore needed, in some cases at doses higher than the usual doses, particularly in the context of high-volume CRRT and prolonged treatments.56 If citrate is used for regional anticoagulation, frequent monitoring of the calcium levels is indicated, as well as of the acid/base balance. As a general rule, the specifications referred to the provision of fiber are similar to those applicable to the rest of critical patients.
How should the caloric/protein supply of micronutrients and fiber be adjusted in the sarcopenic elderly patient?In elderly patients, the resting energy expenditure is reduced by 15%–20%, although the cause of this reduction has not been clearly established. In order to calculate the caloric requirements in the absence of IC, use can be made of the Harris-Benedict equation, adding a correcting factor of about 1.2.57 Regarding the supply of carbohydrates and lipids, the needs are similar to those of other critical patients.
A protein supply of 1.2 g/kg/day has been suggested as the minimum needed for a healthy elderly individual. In the context of critical disease, higher doses would be needed, even exceeding those prescribed in younger critical patients, due to increased resistance to protein synthesis in the elderly. However, no studies have clearly defined the protein requirements in the elderly critical patient; the consensus-based recommendation is 1.2–1.5 g/kg/day.58
In order to prevent sarcopenia and stimulate protein synthesis in the healthy elderly individual, supplementing of certain amino acids has been advocated, particularly leucine and β-hydroxy-β-methylbutyrate (HMB)—the active metabolite of leucine that stimulates protein synthesis at cell level. However, no studies in elderly patients have defined its use to date.59,60
The requirements in terms of vitamins, minerals and trace elements are no different from those of the healthy population, with the possible exception of vitamin D. A randomized study of critical patients in general, with vitamin D deficiency, concluded that the provision of this vitamin does not modify the outcomes, except in individuals with severe deficiency (<12 ng/ml).61 Considering the high prevalence of vitamin D deficiency in the elderly, supplementing could be considered in elderly critical patients with severe vitamin D deficiency, though the latest published meta-analysis does not warrant the use of vitamin D supplements in the critical patient.62
There are no conclusive studies recommending the use of antioxidants in the sarcopenic elderly, and as regards the use of fiber, the recommendations in the elderly population are 20–35 g/day of soluble and insoluble fiber.63
How should the caloric/protein supply of micronutrients and fiber be adjusted in the diabetic patient and in individuals with stress hyperglycemia?The supply of macronutrients in these patients is no different from that indicated in critical patients in general, though it is possible to use strategies designed to reduce glycemia through diets specifically formulated for the diabetic patient. The reduction of carbohydrates with respect to lipids, the use of carbohydrates with a low glycemic index, or the provision of monounsaturated fatty acids can reduce the blood glucose levels and insulin requirements.64 A Spanish prospective study comparing two diabetes-specific diets versus a standard enteral diet in critical patients evidenced improved glycemic control, lesser insulin requirements and a decrease in nosocomial infection risk in the specific diet groups, though with no impact upon either patient stay or mortality.17
There is no clear evidence of benefits of supplementing with vitamins or minerals in diabetic patients without underlying deficiencies. It is therefore advisable to provide the micronutrients (including vitamin E and C, selenium, zinc and copper) needed to cover the international dietetic recommendations and avoid the deficiencies that may manifest in the acute phase of the disease process. The efficacy of antioxidants in the prevention or control of the complications associated to hyperglycemia in the critical patient likewise has not been demonstrated.
Fiber-rich diets exert a protective effect in the diabetic patient, reflected by a significant decrease in glycosylated hemoglobin concentration and in basal glycemia.65 The main mechanisms by which dietetic fiber can improve the glycemic profile are delayed gastric emptying, a decrease in carbohydrate absorption rate in the small bowel, and lowered insulin resistance. The recommendations referred to fiber intake in diabetics are 14 g/1000 kcal, and it is advisable for at least 50% of the supplied fiber to be in soluble form, because this improves the carbohydrate profile (by incrementing the viscosity of the food bolus, thereby slowing nutrient absorption) and also the lipid profile, secondary to the production and posterior absorption of short chain fatty acids after fermentation in the colon. However, the existing evidence does not allow us to firmly define the type of fiber best suited to the diabetic patient.66
Recommendations- -
When available, IC is suggested as the method of choice for calculating the caloric requirements in patients subjected to mechanical ventilation. (Level of evidence: moderate. Grade of recommendation: high).
- -
In the absence of IC, predictive formulas are advised, particularly the Penn State equation, in patients subjected to mechanical ventilation, or simplistic formulas based on body weight. (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
During the first days of the critical disease (acute phase), it is advisable to supply about 70% of the energy expenditure as measured by IC or 20–25 kcal/kg usual body weight/day. Following this period (patient in stable phase), the recommended supply is 25–30 kcal/usual body weight/day. (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
An early hyperproteic supply is advised of between 1.2–1.5 g/usual body weight/day of proteins in the early phase, and between 1.5–2 g/usual body weight/day in the stable phase, particularly in patients at high nutritional risk. (Level of evidence: low. Grade of recommendation: moderate).
- -
In patients receiving PN, it is advisable not to exceed 3.5 g/usual body weight/day of glucose (use adjusted weight in obese individuals with BMI ≥ 30 kg/m2). (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
In critical patients in general, the suggested daily lipid supply is 0.7–1.3 g/kg usual body weight/day (use adjusted weight in obese individuals with BMI ≥ 30 kg/m2), with a reduction in supply if the plasma triglyceride levels exceed 400 mg/dl. (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
No generalized recommendations can be made in critical patients regarding the type of lipids to be supplied, though the use of mixed formulas that reduce the ω-6/ω-3 ration could be useful as a pharmacological strategy associated to artificial nutrition.
- -
It is advisable for nutrition of the obese critical patient to be hypocaloric, covering approximately 50%–70% of the estimated energy requirements, and hyperproteic, with between 2–2.5 g proteins/kg of ideal body weight/day, adjusting the supply to secure an acceptable nitrogen balance. (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
The caloric and protein supply in patients with AKI requires frequent re-evaluation according to the degree of catabolism and the need for renal replacement techniques. (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
In patients with CRRT, the advised protein supply is at least 2 g/kg usual body weight/day, without exceeding 2.5 g/kg usual body weight/day (use ideal weight in obese patients with BMI ≥ 30 kg/m2). (Level of evidence: low. Grade of recommendation: moderate).
- -
Supplementing with vitamins and trace elements is advised in cases of prolonged stay and the prolonged use of CRRT. (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
In diabetic patients it is advisable to administer a fiber-enriched diet (with at least 50% of the fiber in soluble form). (Level of evidence: expert opinion. Grade of recommendation: moderate).
- -
In sarcopenic elderly patients with vitamin D deficiency, supplementing is advised in those individuals with severe vitamin D deficiency. (Level of evidence: low. Grade of recommendation: moderate).
Dr. Serón-Arbeloa has received payment from Fresenius Kabi, Baxter and Nestlé for participation in conferences and in scientific congresses and training courses. Dr. Martínez de la Gándara has received payment for participation in activities financed by Abbott Nutrition, Baxter, Nestle and Fresenius Kabi, involving training and counseling activities, and participation in scientific congresses and courses. Dr. León-Cinto declares that she has no conflicts of interest. Dr. Flordelís has received payment for participation in activities financed by Vegenat Nutrición and Fresenius Kabi, involving research studies and participation in scientific congresses. Dr. Márquez-Vácaro has received payment from Fresenius Kabi and Abbott for conferences, and from Fresenius Kabi for participation in scientific congresses.
Note to supplementThis article forms part of the supplement “Recommendations for specialized nutritional-metabolic management of the critical patient. Metabolism and Nutrition Working Group of the Spanish Society of Intensive and Critical Care Medicine and Coronary Units (SEMICYUC)”, with the sponsorship of Abbott Nutrition.
Please cite this article as: Serón Arbeloa C, Martínez de la Gándara A, León Cinto C, Flordelís Lasierra JL, Márquez Vácaro JA. Recomendaciones para el tratamiento nutrometabólico especializado del paciente crítico: requerimientos de macronutrientes y micronutrientes. Grupo de Trabajo de Metabolismo y Nutrición de la Sociedad Española de Medicina Intensiva, Crítica y Unidades Coronarias (SEMICYUC). Med Intensiva. 2020;44:24–32.