Severity scores are routinely used in clinical practice for various purposes, including to predict mortality. Scores are updated periodically, mainly to take improved treatments into account. The latest versions of the most commonly used scores (SAPS3 and APACHE IV) were developed more than 15 years ago.1,2
Many patients are now admitted to intensive care units (ICUs) with orders to withhold some life-support measures. Our recent multicenter study found that more than 7% of all patients admitted to participating ICUs had limitations on life support; although nearly one-third survived more than 30 days, standard severity scores underestimated their high mortality.3 The accuracy of severity scores’ predictions within centers varies due to variations in performance or in case-mix. Advances in treatments since the most recent version of the score are associated with progressively reduced accuracy.4
Here we report a new analysis including all patients registered in the clinical database at our mixed ICU in a university-affiliated hospital from 2009 through 2017. The UCH Ethics Committee approved the study. Throughout this period, our ICU's admission criteria and case-mix remained unchanged. We admitted 6821 patients (mean age, 65.6 yr; ICU stay, 4.6 days). Hospital mortality was 16.2% and SAPS3-predicted mortality was 27.6%, yielding a standardized mortality ratio (SMR) of 0.59.
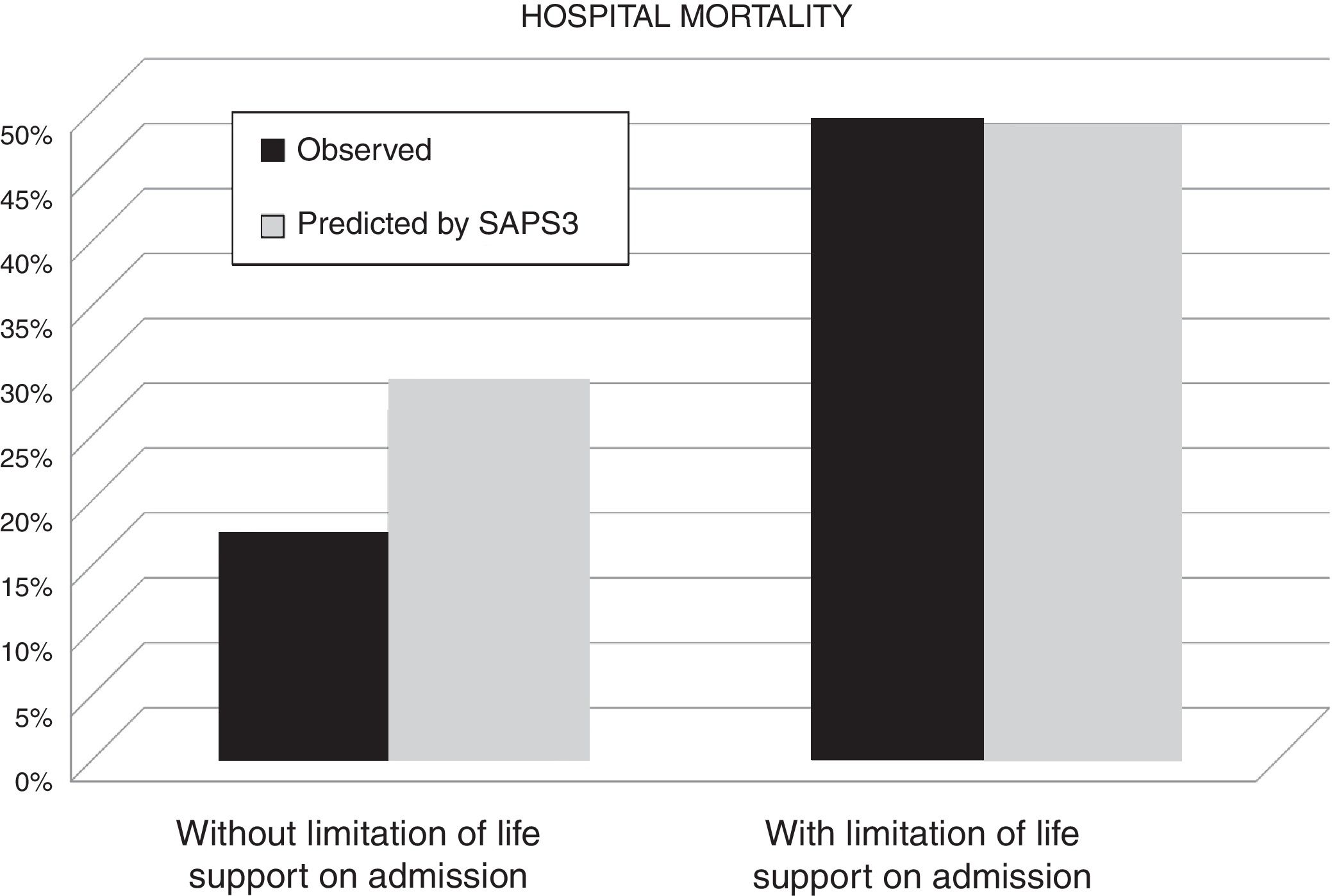
A total of 242 (3.5%) patients had limitations on life support at admission. In this subgroup, hospital mortality was 47.1% and SAPS3-predicted mortality was 46.5% (SMR 1.01); by contrast, in patients without limitations, hospital mortality was 15.1% and SAPS3-predicted mortality was 26.9% (SMR 0.56). We found no significant differences along the years of the study.
Multivariable logistic regression showed that hospital mortality was independently associated with SAPS3 (OR 1.05 [1.051–1.058]; p<0.001) and limitations on life support at admission (OR 2.85 [2.11–3.85]; p<0.001). The area under the receiver operating characteristic curve (AUROC) for the model including these variables was 0.85, similar to the original value for the APACHE IV.2 Not including limitations on life support in the model yielded similar accuracy (AUROC 0.84), probably due to the small proportion of patients with limitations. Nevertheless, the mortality risk in patients with limitations on life support at admission was twice that predicted by standard severity scores (Fig. 1).
The results of our single center analysis are somewhat different from those of a recent multicenter trial. The rate of limitations on life support at admission was lower (3.5% vs. 7.8%) and hospital survival was better (53% vs. 41%), but severity scores’ underperformance in patients with limitations was similar. Taken together, the two studies show the same trend in more than 10,000 patients.
Research networks focused on predictive models will probably update current severity scores in the near future, and we suggest they explore the possibility of including limitations on life support at admission in the new algorithms.