Acute respiratory failure (ARF) represents one of the most common causes of intensive care unit admission and oxygen therapy remains the first-line therapy in the management of these patients. In recent years, high-flow oxygen via nasal cannula has been described as a useful alternative to conventional oxygen therapy in patients with ARF. High-flow oxygen via nasal cannula rapidly alleviates symptoms of ARF and improves oxygenation by several mechanisms, including dead space washout, reduction in oxygen dilution and inspiratory nasopharyngeal resistance, a moderate positive airway pressure effect that may generate alveolar recruitment and an overall greater tolerance and comfort with the interface and the heated and humidified inspired gases. However, the experience in adults is still limited and there are no clinical guidelines to establish recommendations for their use. This article aims to review the existing evidence on the use of high-flow oxygen via nasal cannula in adults with ARF and its possible applications, advantages and limitations.
La insuficiencia respiratoria aguda supone una de las causas más frecuentes de ingreso en los servicios de Medicina Intensiva y la oxigenoterapia sigue constituyendo una terapéutica de primera línea en el manejo de estos pacientes. En los últimos años, la oxigenoterapia de alto flujo ha sido descrita como una alternativa útil a la oxigenoterapia convencional en los pacientes con insuficiencia respiratoria aguda. La oxigenoterapia de alto flujo permite administrar un flujo de gas totalmente acondicionado hasta a 60 L/min mediante cánulas nasales, obteniendo una rápida mejoría de los síntomas debido a diferentes mecanismos como, por ejemplo, una reducción de la resistencia de la vía aérea superior, cambios en el volumen circulante y la generación de cierto grado de presión positiva. Además, todo ello se consigue junto con una mejor tolerancia y comodidad por parte del paciente. Sin embargo, la experiencia en adultos es todavía limitada y no existen guías clínicas que establezcan recomendaciones para su uso. En este artículo se pretende revisar la evidencia existente sobre el uso de oxigenoterapia de alto flujo en pacientes adultos con insuficiencia respiratoria aguda, así como sus posibles aplicaciones, ventajas y limitaciones.
Acute respiratory failure (ARF) is a frequent cause of admission to Intensive Care,1 and oxygen therapy undoubtedly remains one of its first-line management options.2 Under conditions of ARF, oxygen can be administered on an invasive or noninvasive basis. However, whenever possible, we should try to avoid invasive ventilation support.
Noninvasive oxygen therapy can be administered in different ways, for example, through an oronasal mask or using nasal cannulas. However, noninvasive oxygen therapy has a number of limiting factors that condition its efficacy and therefore the correction of hypoxemia and the clinical manifestations associated to ARF. The main limiting factors are tolerance of the application system on one hand, and limitation of the administered oxygen flow on the other. The latter is generally limited to 15l/min,3 and the flow is normally administered under conditions that do not coincide with the ideal temperature and humidity specifications (37°C and 100% relative humidity). This limitation in administered flow implies dilution of the administered oxygen with room air, conditioned by the patient peak inspiratory flow. In this regard, the greater the peak inspiratory flow, the greater the dilution–thereby lowering the real fraction of inspired oxygen (FiO2) administered to the patient.2,4 This situation has little impact upon patients with mild hypoxemia, though in individuals with severe ARF and important hypoxemia with peak inspiratory flows of >30l/min, conventional oxygen therapy may not suffice to correct ARF. An alternative that would overcome these limitations of conventional oxygen therapy is the use of noninvasive mechanical ventilation (NIMV) systems–though the main problem with these systems is patient discomfort and poor tolerance of the interfaces.5
A recently introduced alternative is high-flow oxygen therapy (HFOT),6 which allows us to administer a gas flow of up to 60l/min using silicone nasal cannulas, with ideal conditions of administered gas temperature and humidity (i.e., 37°C and 100% relative humidity). Until a few years ago, this technique had been used mainly in newborn infants.7–9 However, its use in adult patients has increased exponentially in recent years.10
The use of HFOT affords better oxygenation through a series of different mechanisms such as reduced dilution of the administered oxygen with room air,11,12 dead space washout,12–14 increased tidal volume15,16 and the generation of continuous positive airway pressure (CPAP)16–19. The technique could also offer benefits at hemodynamic level,20 increase patient physical exertion capacity and wellbeing,5 and improve mucociliary transport thanks to the active humidification of the administered gas.21,22
The aim of the present study is to offer an update on the possible clinical applications of HFOT, examining the mechanisms whereby it may prove useful in adults with ARF, identifying the patients in which it may be most useful, and establishing the way in which the technique should be used.
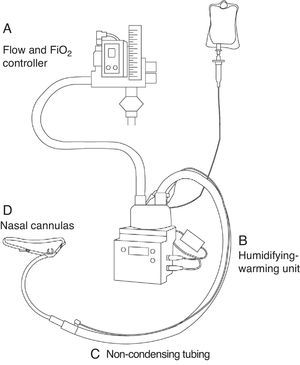
EquipmentThe administration of HFOT requires four elements: (1) a patient interface; (2) a high-flow administration system allowing control of the administered flow and FiO2; (3) a humidifying-warming system; and (4) non-condensing tubing (Fig. 1).
The patient interface consists of special silicone nasal cannulas that are longer than the conventional cannulas. The silicone cannulas come in different sizes, and we must choose the size that best adjusts to the nostrils of each individual patient. Adaptors are also available for tracheotomized patients.
Fraction of inspired oxygen (FiO2)A system capable of administering a high gas flow (0–60l/min) and of adjusting the administered fraction of inspired oxygen (FiO2) is required. Two different systems are able to do this:
- -
Mixing of oxygen and compressed air through two independent wall outlets connected by a Y-tube, or using commercial respirators (Dräger, Lübeck, Germany).
- -
Mixing of oxygen with room air by means of a turbine (Airvo™ system, Fisher & Paykel Healthcare Ltd., Auckland, New Zealand).
The fundamental element for clinical use of the technique is effective humidification of the administered gas. The most widely used commercial systems are Optiflow™ (Fisher & Paykel Healthcare Ltd., Auckland, New Zealand) and Vapotherm™ Precision Flow (Vapotherm, Exeter, USA). These systems allow us to administer the gas warmed to body temperature (37°C) and with a relative humidity of 100%.
Non-condensing tubingA number of commercial tubing systems are available. The important issue in deciding which system to use is that we need mechanisms for preventing or minimizing condensation in the tubes, since condensation has been shown to favor infections.23
Physiological mechanisms of action and clinical effects of high-flow oxygen therapyHigh-flow oxygen therapy has a series of characteristics and mechanisms of action that may be particularly beneficial for patients with severe ARF. A review is provided below of the main mechanisms underlying the beneficial effects of HFOT.
Improved oxygenationOne of the main benefits of HFOT is the improvement of hypoxemia in patients with ARF. The main mechanisms underlying this phenomenon are lesser dilution with room air of the gas administered during inspiration, and a certain pressurization of the airway, giving rise to a certain CPAP-like effect.
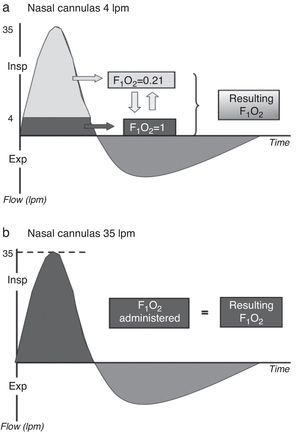
Lesser dilutionOne of the benefits of HFOT is the possibility of providing sufficient flow to satisfy the peak inspiratory flow (PIF) demand of the patient, where the administered FiO2 comes close to the real value received by the patient. This is because the administered gas flow is not diluted with room air (Fig. 2). Under normal conditions, the PIF is about 30–40l/min24; consequently, this in principle could be regarded as the recommended flow range when starting to use HFOT. In patients with severe ARF, the PIF is probably higher, however. For this reason, these are precisely the patients in which the oxygen dilution phenomenon is particularly important. The above would at least partially account for the improvement in oxygenation of these patients with HFOT.25,26 On the other hand, thanks to minimization of the dilution of the administered oxygen with room air, we achieve better control of the administered oxygen concentration.27–29
Dilution of the administered oxygen using a low- (a) and high-flow system (b). Dark gray: oxygen; light gray: room air. During normal inspiration, the peak inspiratory flow (PIF) demand is 30–40l/min. With the use of high-flow oxygen therapy, the administered FiO2 would equal the real FiO2, while in the case of a low-flow system the real FiO2 would be less than the administered FiO2.
Another potential mechanism of action underlying the effects of HFOT is the generation of a certain positive airway pressure. This pressure increment has been demonstrated at nasopharyngeal level and in the oral cavity, as well as in the end-expiratory esophageal and tracheal pressure values obtained.17–19
A number of studies have shown that the flows in the order of 35–60l/min result in mean expiratory pressures at pharyngeal level of 2–3cmH2O with the mouth open, and of 5–7cmH2O with the mouth closed.18,19 Furthermore, it has been seen that the use of HFOT allows an increase in lung impedance at the end of expiration15,16–this parameter in turn being correlated to lung volume. This is important, since it means that the improvement in oxygenation would be partially due to improved alveolar recruitment,5,26,30 attributable at least in part to the mentioned increase in airway pressure.
Dead space washoutAnother aspect to be taken into account is that the flow directly administered to the nasopharynx effectively washes out CO2 from the anatomical spaces, which in turn avoids re-inhalation and affords a reservoir of fresh gas.14,31 This phenomenon reduces the anatomical dead space and increases alveolar ventilation,12 giving rise to improved exercise tolerance,32 less dyspnea, and improved oxygenation.17
Decrease in respiratory work and the metabolic cost of gas conditioningThe use of fully conditioned gas (i.e., administered at ideal temperature and humidity) results in improved tolerance and comfort for patients with ARF,5,33 though it also allows a decrease in respiratory frequency5,16,29 and improves oxygenation. Conditioning of the administered gas with HFOT directly affects oxygenation. In effect, active humidification improves mucociliary function, facilitates the expulsion of secretions and reduces the formation of atelectasis–thereby improving the ventilation/perfusion ratio and oxygenation.5 Furthermore, the administration of fully conditioned gas allows a decrease in airway resistance, which in turn lessens the respiratory work of the patient.4,26
Effect upon the ventilatory and hemodynamic patternDuring inspiration, the negative pressure limits the inspiratory flow due to nasopharyngeal collapse. High-flow oxygen therapy, by generating a certain positive airway pressure, is able to counter this phenomenon.34 Since HFOT allows us to administer flows equal to or greater than the patient PIF, the technique could help minimize upper airway resistance, with a reduction in respiratory work.12 Improved thoraco-abdominal synchrony has moreover been demonstrated with HFOT versus conventional oxygen therapy.35
On the other hand, the use of HFOT increases lung impedance and thus raises the tidal volume.15,16 This situation is usually accompanied by a decrease in respiratory frequency, without changes in PaCO2.5,26,30 Both this change in ventilatory pattern–which could imply a decrease in respiratory work–and the generation of a certain positive intrathoracic pressure could lead to changes in the hemodynamic profile of patients with ARF.36 A recent study has analyzed the hemodynamic effect of HFOT in patients with stable heart failure.20 This effect would consist of a decrease in right ventricle preload (as measured by a decrease in inferior vena cava collapse), which could imply hemodynamic improvement in patients with ARF secondary to myocardial dysfunction.20
Increased patient comfortFailure of NIMV is often due to patient intolerance of the interfaces. In effect, patients may experience claustrophobia or anxiety, as well as erythema, pain or ulceration of the bridge of the nose, and nasal dryness and congestion, irritation of the eyes and gastric bloating. Furthermore, possible air leakage adds discomfort and can interfere with triggering and cycling of the respirator.
All the existing scientific evidence in this respect indicates that the tolerance of HFOT is as good if not better than that of other oxygen therapy techniques,30 since it affords superior patient wellbeing5,36 and generates less noise37 and less nasal dryness.5 In addition, HFOT facilitates verbal communication and allows food intake without requiring circuit disconnections.
Main clinical indicationsAs a result of the different mechanisms of action described above, HFOT has a broad range of clinical indications.38 The main areas in which there is evidence for use of the technique are specified below. In addition, Table 1 summarizes these indications, analyzing the main studies published in the literature and the existing levels of evidence.
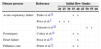
Level of evidence supporting the main clinical indications of high-flow oxygen therapy (HFOT).
| Reference | Type of study | Design | Results | Comments | Level of evidence | |
|---|---|---|---|---|---|---|
| Acute respiratory failure | Sotello et al.38 | Systematic review | Inclusion was made of all the trials (randomized or otherwise) and case series between June 1982 and December 2013, published in English or Spanish | Fifteen studies were included: 5 randomized, 5 non-randomized and 5 retrospective. Patients with ARF: 943 (410 postsurgical, 183 oncological and 143 with pneumonia) | HFOT improved PaO2 in the hypoxemic patients compared with conventional oxygen therapy, and reduced the need for positive pressure ventilation | Ia |
| Roca et al.40 | Retrospective cohort study | Thirty-seven lung transplant patients were included (40 episodes). Conventional oxygen therapy was compared with HFOT | HFOT was associated to a decrease in absolute risk of IMV of 29.8% (OR 0.11; 95%CI 0.02–0.69; p=0.02). NNT=3. The patients not ventilated showed better survival (20.7% vs 100%) | HFOT reduced the need for IMV in the lung transplant patients and thus improved the survival rate | IIb | |
| Frat et al.41 | Randomized, controlled, prospective multicenter trial | Patients with severe ARF. Three groups were compared: HFOT, conventional oxygen therapy and NIMV | Reduction of the OTI rate and of mortality after 90 days in the sub-group of patients with more severe hypoxemia | HFOT showed benefits vs conventional oxygen therapy and NIMV in terms of mortality and reduction of the OTI rate in patients with severe ARF | Ia | |
| Sztrymf et al.26 | Non-randomized prospective study | Thirty-eight patients with ARF or with persistent ARDS. HFOT FiO2 0.88 vs mask FiO2 0.98 | Greater increase in PaO2/FiO2 after 1h HFOT (p=0.036). Greater decrease in RF, HR, dyspnea and thoracoabdominal discoordination | Thirty-nine percent of patients with pneumonia. Non-reduction of RF, PaO2/FiO2 or the persistence of discoordination were identified as predictors of HFOT failure | IIa | |
| Roca et al.5 | Non-randomized prospective study | Twenty patients with ARF. Oronasal mask (FiO2 0.5) during 30min followed by HFOT 20–30lpm 30min | HFOT was associated to higher PaO2 (127 vs 77mmHg; p=0.002) and lower RF (21 vs 28rpm; p=0.001), with no differences in PaCO2 or pH, and with superior tolerance | Pneumonia was the cause of ARF in 65% of the patients | IIa | |
| Sztrymf et al.30 | Non-randomized prospective study | Twenty ICU patients with ARF. Conventional oxygen therapy vs HFOT | HFOT decreased RF (p=0.006) and increased PaO2 (p=0.001). HFOT presented a failure rate of 30% (comparable to that of NIMV) | Fifty percent of patients with pneumonia. After 1h, HFOT improved all the respiratory parameters. HFOT failure rate similar to that of NIMV | IIa | |
| Rello et al.39 | Retrospective cohort study | Thirty-five patients with H1N1 pneumonia | HFOT failure was associated to increased mortality (27.3%) | Delayed intubation in the case of HFOT failure did not imply an increase in mortality | IIb | |
| Post-cardiac surgery | Corley et al.16 | Non-randomized prospective study | Twenty post-heart surgery patients with ARF. Conventional oxygen therapy vs HFOT | HFOT increased the mean airway pressure 3.0 cmH2O (95%CI 2.4–3.7) and also end-expiratory impedance (25.6%; 95%CI 24.3–26.9) | HFOT gave rise to increased airway pressures and tidal volume, and therefore lowered RF and dyspnea, and improved SpO2 | IIa |
| Parke et al.29 | Randomized prospective study | Sixty cardiac ICU patients with mild/moderate hypoxemia. Conventional oxygen therapy vs HFOT 35lpm | Fewer patients in the HFOT showed respiratory failure (26/29 vs 15/27; p=0.006). The need for NIMV was lower in the HFOT group (10 vs 30%; p=0.10). No significant differences in PaO2/FiO2 (p = 0.08) | The use of HFOT appeared to decrease the need for NIMV in these patients | Ib | |
| Parke et al.44 | Randomized prospective study | A total of 340 post-heart surgery patients randomized to conventional oxygen therapy vs HFOT 45lpm during 48h postextubation | Greater SpO2/FiO2 ratio with HFOT (OR 1.18; 95%CI 0.77–1.81; p=0.45). HFOT involved a lesser need to increase ventilatory support (p=0.01) | This study recommended preventive HFOT in post-heart surgery patients before respiratory failure develops | Ib | |
| Stéphan et al.47 | Randomized prospective multicenter study. Non-inferiority study | A total of 830 post-heart surgery patients with a high risk of postextubation ARF | HFOT was not inferior to BiPAP in terms of treatment failure (21.0% vs 21.9%; risk difference 0.9%; p=0.003) or in-ICU mortality (5.5% vs 6.8%; p=0.66). The incidence of ulcers decreased, however (3% vs 10%; p<0.001) | In post-heart surgery patients at risk of ARF, the use of HFOT was not found to be inferior to BiPAP | Ia | |
| Pre-intubation | Miguel-Montanes et al.43 | Non-randomized prospective study | A total of 101 patients included. Control group subjected to preoxygenation with reservoir bag and intervention group subjected to HFOT | SpO2 during OTI was greater with HFOT (100% vs 94%; p<0.0001). The patients with HFOT suffered fewer severe hypoxemia episodes (2% vs 14%; p=0.03) | Preoxygenation with HFOT afforded protection against episodes of severe hypoxemia during OTI (OR 0.146; 95%CI 0.01–0.90; p=0.037) | IIa |
| Postextubation | Maggiore et al.46 | Randomized prospective study | A total of 105 patients with PaO2/FiO2≤300 postextubation. MV (n=52) vs HFOT (n=53) during 48h | PaO2/FiO2 was greater in the HFOT group (287±74 vs 247±81; p=0.03), in the same way as wellbeing. The need for re-OTI was lower with HFOT (4% vs 21%; p=0.01) | The use of HFOT after extubation was associated to a lower reintubation rate | Ib |
| Rittayamai et al.45 | Randomized prospective study | Seventeen patients with IMV. Randomized cross-over study of HFOT or MV during 30min postextubation | The patients with HFOT suffered less dyspnea (p=0.04), with a lower RF (p=0.009) and lower HR (p=0.006), and greater wellbeing (p=0.07) | This study showed that HFOT may play a beneficial role after extubation | Ib | |
| Tiruvoipati et al.28 | Randomized prospective study | Fifty ventilated patients. Randomized cross-over study with HFOT and conventional oxygen therapy | HFOT was better tolerated (p=0.001), but there were no significant differences in either gas exchange or RF | Only one patient required reintubation after 4h | Ib | |
| Invasive procedures | Lomas et al.49 | Clinical case | Myasthenia gravis with severe ARF | Good tolerance of FBS, without desaturation | HFOT could be useful for performing FBS in hypoxemic patients, and may lessen the risk of OTI | III |
| Lucangelo et al.48 | Randomized prospective study | Forty-five patients. MV 40lpm vs nasal mask vs HFOT 60lpm during FBS | At the end of FBS the patients with HFOT showed greater PaO2, PaO2/FiO2 and SpO2 | HFOT 60lpm was superior to MV during FBS | Ib | |
| Simon et al.50 | Randomized prospective study | Forty patients with ARF. HFOT vs NIMV during FBS | SpO2 was greater with NIMV, with no differences in RF, HR or BP | NIMV appeared to be superior in moderate/severe ARF. HFOT was well tolerated in patients with mild ARF | Ib | |
| Heart failure | Roca et al.20 | Non-randomized prospective study | Ten patients with functional class III HF received HFOT with 20 and 40lpm | The use of HFOT was associated to a decrease in inferior vena cava collapse (37% basal, 28% with HFOT20 and 21% with HFOT40; p<0.05), with an attributable reduction of 53% with OAF40 (95%CI 36–67) | The results showed that HFOT could offer benefit in patients with HF | IIa |
| Carratalá Perales et al.36 | Case series | Five patients with acute HF and ALE | These patients were treated satisfactorily with HFOT, with clinical and blood gas improvement, and no complications or failures associated with the technique | HFOT was found to be a good alternative to conventional oxygenation systems in ARF secondary to acute HF in ALE with refractory hypoxemia | IV | |
| Emergency care | Lenglet et al.37 | Non-randomized prospective study | Seventeen patients with ARF. Oronasal mask 9–15lpm vs HFOT 30–40lpm | The use of HFOT was associated to lesser dyspnea, lower RF and improved SpO2 | Pneumonia was the cause of ARF in 53% of the patients | IIa |
| Palliative care | Peters et al.51 | Non-randomized prospective study | Fifty patients with ARF admitted to ICU | HFOT improved SpO2 from 89.1% to 94.7% (p<0.001) and RF from 30.6 to 24.7rpm (p<0.001). NIMV was started in 9 patients (18%), while HFOT was maintained in 82%. The latter was continued an average of 30h | HFOT could ensure adequate oxygenation in patients with vital support limitations | IIa |
BiPAP: Bilevel positive airway pressure; ALE: Acute lung edema; FBS: Fibrobronchoscopy; HR: Heart rate; RF: Respiratory frequency; HF: Heart failure; 95%CI: 95% confidence interval; OTI: Orotracheal intubation; ARF: Acute respiratory failure; MV: Venturi mask; NNT: Number needed to treat; HFOT: High-flow oxygen therapy; OR: Odds ratio; ARDS: Acute respiratory distress syndrome; BP: Blood pressure; ICU: Intensive Care Unit; IMV: Invasive mechanical ventilation; NIMV: Noninvasive mechanical ventilation; PaO2: Arterial partial pressure of oxygen; FiO2: Fractional inspired oxygen; SpO2; Oxygen saturation.
Levels of evidence according to the United States Agency for Health Research and Quality (Ia: Metaanalysis or several randomized, controlled trials. Ib: At least one randomized, controlled trial. IIa: At least one well-designed non-randomized, controlled trial. IIb: At least one cohort study. III: Well-designed non-experimental descriptive studies, such as comparative studies, correlation studies or case-control studies. IV: Expert committee opinions or documents, or clinical experiences or case series).
Roca et al.5 were the first to demonstrate the benefits of the use of HFOT in patients with ARF. After only 30min of application of the technique, significant improvements were noted in both the clinical and physiological parameters. These results were subsequently confirmed by Sztrymf et al.,30–who corroborated a decrease in respiratory frequency and improved oxygenation in these patients.
Furthermore, the use of HFOT allows better handling of the respiratory secretions30,39–a fact which could prove particularly important in patients with ARF of infectious origin.
On the other hand, the use of HFOT could lessen the need for NIMV and even for invasive mechanical ventilation (IMV) in patients with ARF. This possible benefit of HFOT has been analyzed in four studies.26,29,30,40 Sztrymf et al.30 reported an HFOT failure rate of about 30%, which is comparable to that of NIMV.30 In turn, Parke et al.29 found that only 10% of the patients with moderate to severe ARF treated with HFOT required IMV, while this percentage was seen to reach 30% in those cases where an oronasal mask was used. More recently, in a population of lung transplant patients with ARF, HFOT was seen to significantly lessen the need for IMV, with a decrease in absolute mechanical ventilation risk of 30%. Only three patients were needed to avoid a case of intubation, with potential effects upon morbidity–mortality and the cost-effectiveness of the system.40
However, the main issue of whether the use of HFOT lessens the need for IMV remains to be settled. Many clinicians have the impression that HFOT effectively avoids intubation in many patients with ARF, though to date this has not been demonstrated by any controlled clinical trial. A recent study on the clinical impact of HFOT in patients with severe ARF reported a 68% success rate, with the need for mechanical ventilation (invasive or otherwise) in only 32% of the patients.26 Even more notorious are the findings of the FLORALI study,41 which reported the benefits of HFOT compared with conventional oxygen therapy and NIMV in terms of mortality and reduction of the intubation rates in patients with severe hypoxemia. This study analyzed patients with severe ARF treated with HFOT, conventional oxygen therapy or NIMV. The authors documented a lesser intubation rate, as well as a reduction in mortality in the subgroup of more seriously ill patients (with PaO2/FiO2<200mmHg) subjected to HFOT.
On the other hand, it is important to mention that there are a number of early predictors (within the first 12h) of HFOT failure, such as the persistence of tachypnea, thoraco-abdominal discoordination, and the absence of improvement in patient hypoxemia.26
In sum, the use of HFOT in patients with severe ARF could allow: (1) rapid improvement of dyspnea; (2) improvement of hypoxemia; (3) improved management of the respiratory secretions; and (4) a lesser need for mechanical ventilation.
Preoxygenation in tracheal intubation maneuveringIn critical patients, orotracheal intubation maneuvering is associated to a 20% incidence of potentially serious complications basically related to the appearance of hypoxemia in the context of the actual procedure.42 Noninvasive mechanical ventilation could be used to pre-oxygenate the patient before intubation is carried out. However, it must be suspended during laryngoscopy, and therefore does not allow patient oxygenation during the procedure. In contrast, HFOT does not interfere with laryngoscopy and so could allow the administration of oxygen in the course of the technique.14 Miguel-Montanes et al. have demonstrated that the use of HFOT during preoxygenation lowers the prevalence of severe hypoxemia during intubation maneuvering compared with the use of a reservoir-equipped mask.43 Likewise, a recent experimental study has shown the administration of oxygen at a flow of 10l/min to delay the appearance of severe hypoxemia during apnea–thus evidencing that the use of HFOT during orotracheal intubation might prove useful particularly in hypoxemic patients.42
Weaning from mechanical ventilationThe use of HFOT after suspending IMV may be useful both for preventing and treating post-extubation respiratory failure.14,44 Four studies have been published in this regard, and all of them have reported improvement of all the respiratory parameters,45,46 as well as of patient wellbeing when compared with the use of an oronasal mask,28,46 with a decrease in the need for increased ventilatory support,44 and a drop in reintubation rate (from 21% to 4%).46 Recently, the group led by Bérnard47 has published a non-inferiority of HFOT versus NIMV (specifically BiPAP) study in post-heart surgery patients at risk of suffering respiratory failure. The mentioned study recorded no differences in terms of treatment failure or mortality in the Intensive Care Unit (ICU) between the two systems, though the use of HFOT was associated to a significant decrease in skin lesions within the first 24h of use. On the other hand, the use of HFOT in the decannulation of tracheotomized patients is another promising possibility, though no studies have been published in this concrete field to date.
Oxygen therapy during invasive proceduresDuring the conduction of invasive procedures such as fibrobronchoscopy, it is common to observe worsening of hypoxemia as a result of the hypoventilation produced and the use of sedatives. This worsening of hypoxemia can be even greater in the case of bronchoalveolar lavage, and can persist for several hours after completion of the exploration.48 The use of HFOT has demonstrated beneficial effects in the form of lesser worsening of hypoxemia and greater patient comfort compared with conventional oxygen therapy.48,49 Recently, Simon et al.50 reported lesser hypoxemia during the performance of fibrobronchoscopy in favor of NIMV in patients with severe hypoxemia; however, patient tolerance and wellbeing proved far superior with the use of HFOT.50 In the same way, the utilization of HFOT should also be considered in the context of other invasive procedures such as transesophageal echocardiography or digestive tract endoscopic explorations.14,31
Heart failureIt is not uncommon to find patients with acute heart failure who suffer persistent hypoxemia and dyspnea once stabilized, despite the use of conventional oxygen therapy. The results of a recent study show that in these patients HFOT improves dyspnea due to a decrease in respiratory frequency and the improvement of hypoxemia.36 On the other hand, it has also been seen that HFOT in patients with stable chronic heart failure gives rise to a decrease in inferior vena cava collapse without a drop in cardiac output–thus evidencing that HFOT reduces right ventricle preload probably through the generation of a certain positive intrathoracic pressure and an increase in lung volume.20 Hence, the improvement afforded by HFOT in patients of this kind fundamentally could be explained by improved oxygenation and improvement of the hemodynamic profile.11,20,36 However, no studies have compared NIMV versus HFOT in the acute phase of lung edema.
Utilization outside the Department of Intensive Care MedicineHypoxemia and dyspnea are also among the most common symptoms found in patients admitted to the Emergency Care Department. Lenglet et al.37 examined the potential beneficial effects and feasibility of the use of HFOT in patients with ARF (in most cases secondary to respiratory infection or acute lung edema) admitted to the Emergency Care Department, in comparison with conventional oxygen therapy. The results showed HFOT to offer comparatively faster recovery of dyspnea, oxygenation and the rest of respiratory parameters, and the technique was better tolerated and more comfortable for the patients. In turn, HFOT did not involve greater difficulties of use than conventional oxygen therapy. The application of HFOT to the out-hospital transport setting remains to be evaluated.
Palliative careIn those patients in which IMV is not indicated, HFOT could be of benefit,15 since it reduces dyspnea and improves hypoxemia and cough. Furthermore, it is well tolerated by the patients, who can communicate and even be fed with this system.37,51–53 Indeed, a constant finding in many of the studies published to date is improved patient wellbeing with HFOT.
Exacerbation of chronic obstructive pulmonary diseaseIn the case of hypercapnic respiratory failure, HFOT could also offer benefit by reducing PaCO2 and improving the pH value, probably as a consequence of the pressure increase generated in the upper airway.54 However, it is important to mention that the administration of high gas flows could be useful in these patients subject to the condition that we use low FiO2 levels in order to lessen the risk of hypercapnia. Furthermore, these patients with chronic respiratory disease can especially benefit from the improved mucociliary function afforded by HFOT.54,55 Nevertheless, further studies are needed, comparing the use of HFOT versus NIMV/CPAP in this patient sub-group.
Starting HFOTTable 2 summarizes the gas flows used in the different studies. In general, an initial flow of 30–40l/min could be used. As regards FiO2, the administered level should allow us to achieve the desired arterial oxygen saturation values. On the other hand, it is important to make sure that the system reaches the appropriate temperature (37°C) for administration of the gas.
Weaning from the systemIt is difficult to establish guidelines for weaning from HFOT and its replacement by conventional oxygen therapy. However, it would seem reasonable to first lower FiO2 and then the flow.6 An acceptable recommendation could be maintenance of the administered flow until correct oxygenation is achieved with FiO2<0.5. The reduction in flow should be slow (5l/min every 6–8h). Lastly, once correct oxygenation has been achieved with ≤20l/min and FiO2<0.5, we could consider switching from HFOT to conventional oxygen therapy.56 Nevertheless, some patients require the intermittent use of HFOT during the weaning phase.
Contraindications and complicationsNo important adverse effects have been described in relation to the use of HFOT. Active humidification systems allow the administration of fully conditioned gas, thereby minimizing the side effects at nasopharyngeal level. In patients with chronic obstructive pulmonary disease (COPD), the use of high oxygen concentrations can cause respiratory acidosis due to the reduction of respiratory frequency and ventilation-perfusion alterations.57
A number of high-flow systems are available. The ideal choice is a system offering maximum patient comfort with the best humidification and warming characteristics, and involving the use of non-condensation tubing. Such systems should be fitted with mechanisms to prevent or minimize condensation in the tubing, since it may give rise to infectious processes such as the colonization or infection episode produced by Ralstonia, reported by the United States Food and Drug Administration (FDA) with the Vapotherm™ system,23 which has already been controlled.
ConclusionsIn sum, HFOT is a new oxygen therapy option allowing the administration of fully conditioned warmed and humidified gas at very high flow rates–improving patient oxygenation and wellbeing, and minimizing the adverse effects at nasopharyngeal level. Based on the current body of evidence, HFOT is an attractive and useful option in patients with ARF, since it improves oxygenation, lessens respiratory work, and affords improved patient wellbeing. However, further studies are needed to determine its potential impact in terms of morbidity–mortality and cost-effectiveness.
Conflict of interestFisher & Paykel collaborates with the Institut Mar d’Investigacions Mèdiques (IMIM) through a post-doctorate research grant.
Please cite this article as: Masclans JR, Pérez-Terán P, Roca O. Papel de la oxigenoterapia de alto flujo en la insuficiencia respiratoria aguda. Med Intensiva. 2015;39:505–515.