To assess the clinical impact of on-site thrombolysis vs referral to another hospital in patients with ischemic stroke attended in a hospital lacking a stroke unit.
DesignExpected value decision analysis and Monte Carlo simulation.
Patients and settingDecision analysis based on a cohort study (SIT-MOST) and a meta-analysis of randomized trials of thrombolysis vs placebo in patients with acute ischemic stroke.
InterventionsOn-site thrombolysis (in hospitals lacking a stroke unit) vs delayed thrombolysis in a reference hospital.
Main outcomesNeurological outcome (modified Rankin scale) three months after admission according to the delay in the introduction of thrombolysis.
ResultsAt baseline (initial delay of 135min, travel time 60min), on-site treatment was more effective than referral to another hospital (number of patients with favorable neurological outcome 45.3% vs 41.3%). In patients seen within 45min of the onset of symptoms, for every 10 patients transferred there was an additional case with an unfavorable neurological outcome that could have been avoided with on-site thrombolysis. In the Monte Carlo analysis, biased against on-site treatment by a reduction in effectiveness of 30%, on-site treatment was superior to patient referral in 77.2% of the cases.
ConclusionsThe available evidence does not support the recommendations of the national stroke strategy or some regional plans that discourage the administration of thrombolysis in hospitals without stroke units.
Cuantificar los resultados clínicos de la trombolisis in situ frente a la trombolisis diferida en un hospital de referencia en pacientes con ictus isquémico atendidos en un hospital sin unidad de ictus.
DiseñoAnálisis de decisiones de valor esperado y simulación de Monte Carlo.
Pacientes y ámbitoSimulación basada en un estudio de cohortes (SIT-MOST) y un meta-análisis de ensayos aleatorizados de trombolisis contra placebo en pacientes con ictus isquémico agudo.
IntervencionesTrombolisis in situ frente a la trombolisis diferida en un centro dotado de unidad de ictus.
Variables principalesResultados neurológicos (escala de Rankin modificada) a los tres meses del ingreso en función de la demora en la aplicación de la trombolisis.
ResultadosEn las condiciones basales del estudio SIT-MOST (demora inicial de 135 min, tiempo de transporte de 60 min) el tratamiento in situ fue más efectivo que la derivación a otro hospital (número de pacientes con resultado neurológico favorable de 45,3% frente al 41,3%). En los pacientes atendidos a los 45 minutos, de cada 10 pacientes trasladados se produce un caso adicional con resultado neurológico desfavorable, que se hubiera evitado con el tratamiento trombolítico in situ. En el análisis de Monte Carlo, sesgado en contra del tratamiento in situ mediante una reducción de la efectividad del 30%, el tratamiento in situ fue superior a la derivación de los enfermos en el 77,2% de los casos.
ConclusionesLa evidencia disponible no apoya las recomendaciones de la estrategia nacional del ictus y de los diversos planes autonómicos que desaconsejan la realización de trombolisis en hospitales sin unidades de ictus.
Early thrombolysis in ischemic stroke patients reduces the area of cerebral infarction and improves the functional outcome after three months.1 The benefit of such treatment decreases on a continuous basis with the time elapsed from symptoms onset2; administration therefore should be carried out as soon as possible.
In Spain, different autonomous regions have developed plans for the administration of thrombolysis in ischemic stroke. These strategies often disadvise thrombolysis in centers lacking a Stroke Unit, and recommend transferring the patient to a reference center.3–6 Unfortunately, this recommendation is not based on the best available evidence but on the opinions of experts, which are hampered by potential conflicting professional interests, and fails to take into consideration the added delay in treatment implied by patient transfer.
Quality evidence has recently become available on the efficacy of thrombolysis according to the time from symptoms onset,2 thereby allowing a rational approach to the problem, from the patient perspective.
The present study involves decision analysis to evaluate the relative effectiveness of transfer to a reference center vs on-site treatment of ischemic stroke in patients amenable to thrombolytic treatment.
MethodsThe analysis was based on a decision tree with two alternatives: on-site treatment vs referral to a reference hospital (Fig. 1). The primary clinical outcome (terminal nodes of the decision tree) was the recording of a favorable neurological outcome (defined as a score of 0–1 on the modified Rankin scale) after three months (Table 1).
Decision tree. T1: Symptoms-treatment decision time: Triangular (135/45/270). T2: Secondary transfer time: Triangular (60/30/120).
Po: A priori probability of a favorable neurological outcome: Triangular (0.34/0.25/0.45). Px: Penalization due to lack of a Stroke Unit: Triangular (0.3/0/0.5). In the case of on-site treatment, the odds ratio is penalized by the variable Px. In the case of treatment in a reference center, the delay is penalized by the transfer time.
Modified Rankin classification.
| 0 | No symptoms |
| 1 | No important disability. Able to perform routine activities and obligations |
| 2 | Mild disability. Unable to carry out some previous activities, but able to care for personal interests and issues without help |
| 3 | Moderate disability. Symptoms which significantly restrict lifestyle or preclude fully autonomous living (e.g., needs some help) |
| 4 | Moderately severe disability. Symptoms that clearly impede independent living, though without the need for continuous care (e.g., unable to attend personal needs without help) |
| 5 | Severe disability. Totally dependent, requiring constant help day and night |
| 6 | Death |
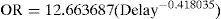
The association between the efficacy of thrombolytic treatment and the time elapsed from symptoms onset was based on the study published by Lees et al.,2 a metaanalysis of 8 randomized clinical trials estimating the effectiveness (odds ratio) of thrombolysis according to the time to treatment. To this effect, we adjusted a geometric function to the data of the mentioned metaanalysis, based on linearized models. The resulting function showed an excellent data fit (r2=0.9787):
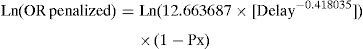
where OR=odds ratio of a favorable neurological outcome of thrombolytic treatment vs placebo; Delay=minutes from symptoms onset to treatment.With the purpose of evaluating the possible impact of the lack of a Stroke Unit, the OR in the case of on-site thrombolysis was penalized by a fictitious variable (Px), according to the following expressions:
where Ln (OR)=Naperian logarithm of OR; Px=penalization due to the lack of a Stroke Unit (a probability ranging from 0=absence of penalization to 1=penalization of 100%); exp=exponential.The OR values were transformed into relative risk (RR) values by means of the following expression7:
where RR=relative risk (variable according to the time elapsed); Po=baseline prevalence of a favorable neurological outcome (without thrombolysis).The practical meaning of these expressions is shown in Table 2.
Relative risk of a favorable outcome with thrombolysis involving different degrees of penalization due to the lack of a Stroke Unit.
| Penalization | Symptoms onset-treatment time (minutes) | |||||
| 45 | 90 | 135 | 180 | 225 | 270 | |
| 0 | 1.68 | 1.47 | 1.34 | 1.25 | 1.19 | 1.13 |
| 0.30 | 1.47 | 1.32 | 1.24 | 1.18 | 1.13 | 1.09 |
| 0.50 | 1.33 | 1.23 | 1.17 | 1.12 | 1.09 | 1.07 |
The probability of a favorable neurological outcome without thrombolysis is assumed to be 0.34.
The number needed to treat (NNT) was calculated as follows:
where NNT=number needed to treat to secure an additional case of favorable neurological outcome after three months; DR=absolute difference of the expected prevalences of favorable neurological outcome between the referral and on-site treatment strategies.The impact of treatment delay and of penalization due to the lack of a Stroke Unit was assessed by means of sensitivity analysis. To this effect, the expected value of each strategy was recalculated for different values of these variables, checking whether the optimum strategy changed or not.8 However, traditional sensitivity analysis is not very practical for jointly assessing the effect of more than two variables. As a result, the deterministic sensitivity analysis was completed by a Monte Carlo simulation9,10–a probabilistic sensitivity analysis taking into account all the variables subject to uncertainty simultaneously. To this effect, instead of directly including the values of the variables in the decision tree, it is assumed that each variable included in the model has a probability distribution. In our case the variables were: the baseline prevalence of a favorable neurological outcome without thrombolytic treatment, the interval from symptoms onset to treatment, the transfer time to the reference center, and the penalization due to the lack of a Stroke Unit. These variables in turn were transformed into triangular distributions with most frequent/minimum/maximum values of 0.34/0.25/0.45; 135/30/160; 60/45/120; and 0.3/0/0.5, respectively. These four distributions were randomly sampled in 10,000 simulations, registering the number of cases in which each alternative was of choice. The end result offers a compact measure of the uncertainty of the results associated to the probabilistic nature of the input variables.
ResultsThe baseline scenario assumed a prevalence of favorable neurological outcomes in the control group (i.e., not subjected to thrombolysis) of 34%, an interval from symptoms onset of 135min (similar to the data of the SIT-MOST study11), and an additional delay due to transfer to the reference center of 60min. Under these conditions, the expected prevalence of favorable neurological outcomes was 45.3% in the on-site treatment group vs 41.3% in the patients transferred to the reference center (number needed to treat [NNT]=25).
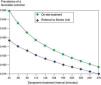
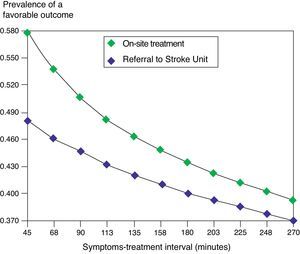
The relative benefit of on-site treatment was greater during the first hours following symptoms onset (Fig. 2). Accordingly, the NNT varied from 10 (45min after symptoms onset) to 44 (270min).
Sensitivity analysis of the variable symptoms-treatment decision time. The prevalence of a favorable outcome decreases as the time from symptoms onset to thrombolysis treatment decision increases. In the considered time range, the expected prevalence of favorable outcomes is always greater with the on-site treatment strategy. The difference between the two strategies is greater at the start of the clinical condition, and decreases over time.
The sensitivity analysis showed that within the time range considered, when the penalization of on-site treatment is under 17%, the treatment of choice is on-site thrombolysis.
In the Monte Carlo analysis, biased against on-site treatment through a 30% reduction in effectiveness, on-site therapy was found to be superior to patient referral in 77.2% of the cases.
DiscussionMany studies show Stroke Units to improve the clinical outcome of ischemic stroke patients compared with conventional treatment in the ward.12–14 Unfortunately, however, the number of such Units is limited, and sometimes transfer to the reference center cannot be made in an acceptable period of time. Under such conditions it is necessary to decide between patient transfer to a Stroke Unit (with the associated additional delay) or on-site treatment in any of its variants (admission to Intensive Care,15 telemedicine-assisted thrombolysis,16,17 thrombolysis and referral–“drip and ship”18–etc.).
In the absence of randomized clinical trials establishing face-to-face comparisons of these two strategies, our study involves a decision analysis based on the best available evidence regarding the impact of a delay in thrombolysis upon the clinical outcome, and biased in favor of patient transfer to a Stroke Unit. According to the results obtained, the treatment of choice in a baseline situation similar to that described in different epidemiological studies11,13 is on-site patient treatment. Transfer to another center would only be justified when the effectiveness of on-site thrombolytic treatment is taken to be far less effective than that administered in a hospital with a Stroke Unit.
This latter assumption does not appear reasonable, since it contradicts the evidence derived from observational studies that support the following conclusions: (1) thrombolysis in patients without signs of bleeding in the computed axial tomography study is safe19; (2) following a brief training intervention, the clinical results of thrombolysis obtained in centers with physicians not specialized in stroke are comparable to those reported by the published clinical trials11; (3) the neurological outcome is not associated to initial care provided by a neurologist20; (4) the bleeding complications of thrombolysis increase when the door-to-needle interval exceeds 60min.21
These results would advise urgent modification of some of the Spanish regional plans, authorizing “stroke teams” to administer fibrinolytic agents on-site after establishing a correct indication, guaranteed through adequate training and accreditation of the clinicians and/or remote assistance provided by an expert.
The data obtained also point to the need for the health authorities to be sufficiently flexible to adapt to the local realities and to take all the available resources into account–independently of the limits imposed by the specialty as such.
Conflict of interestThe authors declare no conflicts of interest.
Please cite this article as: Latour-Pérez J, Galdos Anuncibay P. Trombolisis en el ictus isquémico agudo en centros sin unidad de ictus: ¿derivación a centro de referencia o tratamiento in situ? Med Intensiva. 2012;36:324–8.