To determine the value of Vd/Vt as a predictor of extubation failure in patients with mechanical ventilation admitted to the intensive care units.
DesignA prospective, observational cohort study conducted from 1 September 2010 to 1 March 2011.
SettingGeneral intensive care unit (G-ICU) of a third level university hospital.
Patients or participantsThe study included patients on mechanical ventilation (MV) for over 12h, and who in the process of weaning were subjected to low-level pressure support. Exclusion criteria were age under 18 years, ventilation via tracheotomy and patients failing to cooperate for different reasons.
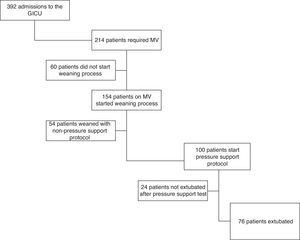
During the study, 392 patients were admitted to the G-ICU; of these, 214 required MV. The weaning process was started in 154 cases. Fifty-four patients were excluded from the study, and 24 were not extubated from MV. A total of 76 patients were finally extubated and analyzed.
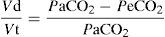
Variables of interestVd/Vt was calculated as the ratio (PaCO2−PeCO2)/PaCO2, with the recorded parameters.
ResultsLogistic regression analysis showed a significant association between the Vd/Vt and extubation failure, with OR=1.52 (95%CI 1.11–2.09, p=0.008).
The area under the ROC curve with respect to the prediction of extubation failure according to the Vd/Vt value was 0.94 (95%CI 0.86–0.98, p<0.0001).
ConclusionsVd/Vt is a powerful predictor of extubation failure in patients on MV.
Comprobar qué valor tiene la fracción de espacio muerto (Vd/Vt) como predictor del fracaso en la extubación de los enfermos que necesitaron ventilación mecánica (VM) ingresados en las unidades de cuidados intensivos.
DiseñoEstudio de cohortes, prospectivo, observacional. Desde el 1 de septiembre de 2010 hasta 1 de marzo de 2011.
ÁmbitoUnidad de cuidados intensivos generales (UCIG), del complejo hospitalario de tercer nivel Hospital Universitario Marqués de Valdecilla.
Pacientes o participantesSe han incluido en el estudio aquellos enfermos que recibían VM por un espacio de tiempo superior a las 12 horas; y quienes en el proceso de destete seguían un protocolo de presión soporte de bajo nivel. Han sido criterios de exclusión la edad inferior a 18 años, enfermos ventilados a través de traqueotomía y enfermos considerados no colaboradores por diversas causas.
Durante el periodo de estudio, ingresaron en UCIG 392 enfermos. De ellos 214 precisaron ventilación mecánica. En 154 se inició proceso de destete. Fueron excluidos del estudio 54 enfermos y no fueron extubados de VM 24. Finalmente 76 enfermos fueron extubados y analizados.
Variables de interés principalesSe calculó Vd/Vt como el cociente (PaCO2−Pє CO2)/PaCO2; con los parámetros registrados.
ResultadosEl análisis de regresión logística mostró una asociación significativa entre la variable Vd/Vt y el fracaso en la extubación con una OR de 1,52 (IC 95%: 1,11-2,09; p=0,008). El área bajo la curva ROC, con respecto a predecir el fracaso en la extubación mediante el valor de Vd/Vt fue de 0,94 (IC 95%: 0,86-0,98; p<0,0001).
ConclusionesConsideramos Vd/Vt un potente predictor del fracaso en la extubación de la VM.
The extubation of patients who have required invasive mechanical ventilation (MV) is common practice in Intensive Care Units (ICUs), but is not without problems. Between 25 and 40% of all patients develop signs of breathing difficulty after extubation.1–3 Extubation failure, defined as the need for re-intubation in the first 48h after extubation, occurs in 5–20% of all patients, depending on the population studied.4 In this context, the risk is greater in clinical and in neurological patients.
Re-intubated patients suffer greater in-hospital mortality and longer stays in the ICU and in hospital, with an increased need for tracheotomy, and often require greater long-term medical care.5–8 Avoidable delays in extubation prolong the stay in the ICU, increase the risk of pneumonia and in-hospital mortality,9 and generate total and daily hospital costs that double the costs generated by patients who are successfully extubated.10
A review fundamented upon medicine, based on evidence, and identified over 50 objective physiological variables (weaning predictors) as tools for evaluating the degree of preparation for spontaneous breathing among patients on MV. Of these weaning predictors, only 5 (negative inspiratory force, minute ventilation (Vm), respiratory frequency (Fr), tidal volume (Vt) and Fr/Vt ratio) were significantly associated to the probability of weaning success or failure — though their predictive capacity was not very high.11–13
The dead space (Vd) is the component of ventilation that is wasted, since it does not participate in gas exchange.14 The dead space fraction (Vd/Vt) has already been used in the identification of pulmonary thromboembolism,15,16 in the management of chronic obstructive pulmonary disease (COPD),17 in the determination of pulmonary dysfunction in adults with sepsis,18 and as a discriminant factor in weaning from MV among children.19,20
The main objective of the present study was to analyze the usefulness of Vd/Vt as a predictor of extubation success in patients subjected to MV in the ICU.
Patients and methodsA prospective, observational cohort study was carried out.
Study populationThe study population comprised patients admitted to the general ICU (GICU) of a third-level hospital (Marques of Valdecilla University hospital, Santander, Spain) and who met the following inclusion criteria: (a) MV for over 12h; (b) a weaning process following a low-level pressure support protocol in continuous positive airway pressure-assisted spontaneous breathing (CPAP+ASB) mode with an Evita 4 ventilator. The exclusion criteria were: age under 18 years, tracheostomy ventilation, and patients considered to be unable to collaborate for different reasons.
During the study period, a total of 392 patients were admitted to the GICU. Of these, 214 required MV, and weaning was started in 154 cases. We excluded 54 patients: 14 subjects who did not require MV for more than 12h, and 40 in which weaning did not involve a low-level pressure protocol. Of the 100 patients who started weaning, 24 failed to pass the test and were not extubated from MV. A total of 76 patients were therefore finally studied (Fig. 1).
Weaning protocolThe weaning protocol first comprised the checking of a series of criteria: manifest healing or improvement of the condition leading to MV; hemodynamic stability with vital signs within normal or acceptably safe limits; positive cough reflex (spontaneous or upon aspirating); absence of anemia; no need or high-dose vasoactive drugs; no uncontrolled signs of sepsis or presence of hyperthermia; good nutritional condition (body mass index (BMI) 18.5–24.9kg/m2; albuminemia≥3.5g/dl); patient mood stability (no signs of depression, irritability or loss of interest); acid–base and electrolyte balance with adequately safe margins (pH: 7.34–7.43; sodium 135–145meq/l; potassium 3.5–5.0meq/l; calcium 8.1–10.4mg/dl; magnesium 1.6–2.5mg/dl; chloride 95–105meq/l). Secondly, the circuit was equipped with a Dräger mainstream CO2 sensor affording continuous measurement of etCO2. In turn, a low-level pressure support test was performed. The respirator used in the study was the Evita 4 edition (Dräger) in CPAP+ASB mode, adjusting the positive end expiratory pressure (PEEP) (never>4) and the assisted spontaneous breathing pressure value (ASB). In this case the ASB value was at least 4mbar in patients with a 9mm endotracheal tube, 6mbar in 8mm tubes, and 8 mbar in the case of 7mm tubes. The test was performed with a trigger of 2l/min. With this reference we aimed to obtain tidal volumes of 6 and 10ml/kg ideal body weight. If the pressures required to achieve these volumes exceeded 20mbar in ASB, the patient was not considered amenable to weaning and extubation.
The duration of the CPAP+ASB test was at least 30min. This time could be extended according to medical criterion, though in no case could it exceed 120min. The patient was considered to have failed the test (and was therefore not regarded as a candidate for extubation) in the event of the following:
- a.
Maintenance of a respiratory frequency>35rpm during 5min.
- b.
A decrease in arterial oxygen saturation (SaO2) to <90% (as determined by blood gas measurements).
- c.
Tachycardia>140 bpm maintained during 2min.
- d.
Arterial hypertension with systolic blood pressure (SBP)>180mmHg or arterial hypotension with diastolic blood pressure (DBP)<90mmHg.
- e.
Appearance or increase in patient anxiety, diaphoresis or abdominal respiration.
If the patient passed the test, extubation was carried out. Instants before extubation, arterial blood gas determination was performed. Posterior patient follow-up lasted 48h, and in this period any possible failures were registered.
Extubation failure was defined by the following:
- a.
The need for re-intubation and connection to MV due to partial or total respiratory failure.
- b.
Repeat connection to MV due to diminished patient consciousness of respiratory origin.
- c.
The need for noninvasive MV due to partial or total respiratory failure.
- d.
Sudden and unexpected death in the first 48h.
- e.
Incapacity to manage secretions, resulting in the need for repeated aspiration by the nursing personnel every 15min.
The need for re-connection due to upper airway obstruction was not regarded as failure in disconnection from MV.
Registered variables. Analyzed variablesFor each patient we recorded personal and demographic data such as age and sex. The disease leading to the need for MV was registered, along with personal antecedents of chronic obstructive pulmonary disease (COPD) and the Acute Physiology and Chronic Health Evaluation II (APACHE II) score of the patient. Patient height was measured, and the ideal body weight was calculated using the Devine method:
Ideal male weight=50kg+0.91 (height [cm] – 152.4)
Ideal female weight=45.5kg+0.91 (height [cm] – 152.4)
Before the CPAP+ASB test, we recorded the patient heart rate (HR), SBP and DBP, and SaO2 (measured by pulsioximetry) and the Fr.
The parameters used during the test were registered: inspiratory oxygen fraction (FiO2), PEEP, ASB, and its duration in minutes. When the test was considered successful, we recorded the values corresponding to peak pressure, Vm, Vt and the expired CO2 volume (VCO2), obtained from the screen of the Evita 4 ventilator.
After completing the test we again measured the patient HR, SBP and DBP, SaO2 (measured by pulsioximetry) and Fr, as well as the arterial oxygen pressure (PaO2) and the arterial carbon dioxide pressure (PaCO2).
All the variables were entered in a datasheet, with calculation of the dead space fraction (Vd/Vt) based on the following equation:
where PaCO2 is obtained from the arterial blood gas measurements, and PeCO2 (carbon dioxide pressure in exhaled air) is calculated from the data obtained by the CO2 sensor of the Dräger respirator.Accordingly: PeCO2=FeCO2×Patm
FeCO2 (carbon dioxide fraction in exhaled air) is calculated from the following equation:
The values of VCO2 and Vm are obtained directly from the respirator screen. Atmospheric pressure (Patm) was taken to be a fixed value of the subtraction 760–47mmHg (the water vapor pressure value): 713mmHg. With the data obtained we also calculated the ratio between Fr and Vt in each patient, as well as the PaO2/FiO2 ratio.
All the variables were recorded by medical personnel blinded to the Vd/Vt value obtained at the time of deciding both extubation and re-intubation, where required.
Statistical analysisContinuous variables were expressed as the mean±standard deviation (SD), while categorical variables were expressed as percentages with the corresponding 95% confidence interval (95%CI).
The univariate analysis between the extubation failure and success groups compared the values of the continuous variables using the Student's t-test. Categorical variables in turn were compared using the chi-squared test or the Fisher exact test, as applicable.
Logistic regression analysis explored the association to extubation failure, expressed as the odds ratio (OR) and 95%CI, for those values showing statistical significance or a tendency towards significance in the univariate analysis.
Receiver operating characteristic (ROC) curves were used to plot sensitivity (Y-axis) versus the proportion of false-positive readings (1−specificity) (X-axis), establishing the cutoff point corresponding to maximum diagnostic discrimination of the scale, together with its global assessment as expressed by the area under the curve (AUC). The diagnostic characteristics were estimated from the calculation of sensitivity and specificity, with determination of the positive and negative predictive values of the optimum cutoff point. The statistical analysis was carried out using the MedCalc® 11.4.2.0 statistical package. The study was authorized by the Clinical Research Ethics Committee of Cantabria (Spain).
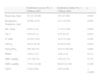
ResultsDescriptive analysis of the sampleThe main demographic characteristics of the 100 patients that started the weaning process are reported in Table 1, stratified according to whether extubation was achieved or not. The mean duration of the CPAP+ASB test was 52min (SD 21.77). Table 2 shows the principal variables obtained on completing the weaning protocol, again stratified according to whether extubation was achieved or not.
Main characteristics of the 100 patients of the study cohort, stratified according to whether extubation was carried out or not.
| Extubated patients No.=76Mean (SD) | Non-extubated patients No.=24Mean (SD) | |
| APACHE II | 12.86 (6.82) | 13.50 (6.90) |
| Age | 64.39 (11.96) | 66.25 (12.03) |
| Ideal weight | 64.62 (3.2) | 66 (3.4) |
| No. (%) | 95%CI | No. (%) | 95%CI | |
| Sex (males) | 47 (69) | 50–73 | 15 (62) | 41–84 |
| Known COPD | 20 (26.31) | 15.75–36.87 | 6 (25) | 9.77–46.71 |
| Cause of MV | ||||
| COPD exacerbation | 17 (22.36) | 12.34–32.39 | 6 (25) | 9.77–46.71 |
| Pneumonia | 12 (15.78) | 6.93–24.64 | 4 (16.66) | 4.73–37.38 |
| Stroke | 11 (14.47) | 5.90–23.04 | 3 (12.5) | 2.65–32.36 |
| Subarachnoid bleeding | 1 (1.31) | 0.03–7.11 | 0 (–) | – |
| Status epilepticus | 1 (1.31) | 0.03–7.11 | 0 (–) | – |
| Heart failure | 4 (5.26) | 1.45–12.93 | 2 (8.33) | 1.02–26.99 |
| Pulmonary thromboembolism | 1 (1.31) | 0.03–7.11 | 0 (–) | – |
| Septic shock | 20 (26.31) | 15.75–36.87 | 8 (33.33) | 12.39–54.27 |
| Hypovolemic shock due to UDB | 4 (5.26) | 1.45–12.93 | 0 (–) | – |
| Cardiorespiratory arrest | 3 (3.94) | 0.82–11.10 | 1 (4.16) | 0.10–21.12 |
| Complicated postoperative course | 2 (2.63) | 0.32–9.18 | 0 (–) | – |
APACHE II: Acute Physiology and Chronic Health Evaluation II; SD: standard deviation of the mean; COPD: chronic obstructive pulmonary disease; UDB: upper digestive bleeding; 95%CI: 95% confidence interval; No.: number of patients; MV: mechanical ventilation.
Variables obtained at the end of the weaning protocol, stratified according to whether extubation was carried out or not.
| Extubated patients No.=76Mean (SD) | Non-extubated patients No.=24Mean (SD) | |
| Hours on MV | 106.25 (160.78) | 130.80 (210.60) |
| f/Vt | 41.95 (15.87) | 46 (18.25) |
| Systolic blood pressure, mmHg | 137.44 (21.04) | 138.65 (25.34) |
| Diastolic blood pressure, mmHg | 72.53 (12.95) | 72.67 (14.56) |
| SpO2 | 97.48 (2.27) | 96.780 (4.45) |
| Heart rate | 95.40 (20.83) | 102.87 (42.54) |
| Respiratory frequency | 21.89 (5.26) | 32.42 (6.45) |
| Mv, l/min | 10.09 (2.57) | 11.60 (3.42) |
| Vte, l | 0.55 (0.12) | 0.42 (0.14) |
| P ASB | 10.71 (3.73) | 18.45 (6.56) |
| PaCO2, mmHg | 40.48 (6.20) | 41.89 (5.89) |
| PaO2/FiO2 | 281.66 (66.16) | 270.88 (82.85) |
| Vd/Vt | 0.52 (0.11) | 0.56 (0.26) |
APACHE II: Acute Physiology and Chronic Health Evaluation II; SD: standard deviation of the mean; COPD: chronic obstructive pulmonary disease; f/Vt: respiratory frequency/tidal volume ratio; UDB: upper digestive bleeding; No.: number of patients; P ASB: pressure support; PaCO2: arterial carbon monoxide pressure; PaO2/FiO2: arterial oxygen pressure/inspiratory oxygen fraction ratio; SpO2: arterial oxygen saturation measured by pulsioximetry; Vd/Vt: dead space fraction; MV: mechanical ventilation; Mv: minute volume; Vte: expiratory tidal volume.
Extubation failed in 22% (17 out of 76) of the patients. No patients were re-intubated due to glottic edema.
Comparative univariate analysis between the extubation failure and success groupsTable 3 shows the comparative analysis of the studied characteristics, according to extubation success or failure. Likewise, Table 4 reports the differences between the analyzed variables according to extubation success or failure.
Comparative univariate analysis of extubation success or failure according to the characteristics of the patients of the study cohort.
| Extubation success, No.=59Mean (SD) | Extubation failure, No.=17Mean (SD) | p | |
| APACHE II | 12.78 (6.75) | 13.17 (7.27) | 0.837 |
| Age | 64.78 (11.52) | 63.05 (13.65) | 0.604 |
| No. (%) | 95%CI | No. (%) | 95%CI | p | |
| Sex | |||||
| Male | 35 (59) | 46–73 | 12 (71) | 44–89 | 0.576 |
| Female | 24 (41) | 27–54 | 5 (29) | 10–55 | |
| Cause of MV | 0.213 | ||||
| COPD exacerbation | 14 (24) | 12–35.45 | 3 (17) | 3.8–43.43 | |
| Pneumonia | 9 (15) | 5.32–25.27 | 3 (17) | 3.8–43.43 | |
| Stroke | 9 (15) | 5.23–25.27 | 2 (12) | 1.4–36.44 | |
| Subarachnoid bleeding | 1 (1.7) | 0.04–9.9 | 0 (–) | – | |
| Status epilepticus | 0 | – | 1 (6) | 0.14–29 | |
| Heart failure | 4 (6.78) | 1.87–16.45 | 0 | – | |
| Pulmonary thromboembolism | 0 | – | 1 (6) | 0.14–29 | |
| Septic shock | 13 (22) | 10.61–33.4 | 7 (41) | 18.44–67 | |
| Hypovolemic shock due to UDB | 4 (7) | 1.87–16.45 | 0 | – | |
| Cardiorespiratory arrest | 3 (5) | 1–14.14 | 0 | – | |
| Complicated postoperative course | 2 (3) | 0.4–11.71 | 0 | – | |
APACHE II: Acute Physiology and Chronic Health Evaluation II; SD: standard deviation of the mean; COPD: chronic obstructive pulmonary disease; UDB: upper digestive bleeding; 95%CI: 95% confidence interval; No.: number of patients; MV: mechanical ventilation.
Comparative univariate analysis of extubation success or failure according to the variables of the patients obtained prior to extubation.
| Extubation success No.=59Mean (SD) | Extubation failure No.=17Mean (SD) | p | |
| Heart rate, bpm | 93.22 (18.06) | 103 (27.80) | 0.082 |
| Respiratory frequency, rpm | 20.96 (4.47) | 25.11 (6.56) | 0.003 |
| Mv, l/min | 9.80 (2.14) | 11.10 (3.60) | 0.064 |
| Vte. l | 0.55 (0.11) | 0.55 (0.12) | 0.952 |
| P ASB | 10.78 (3.87) | 10.47 (3.28) | 0.764 |
| PaCO2 | 39.51 (6.14) | 43.84 (5.29) | 0.010 |
| PaO2/FiO2 | 293 (63.75) | 242.27 (60.49) | 0.004 |
| PEEP | 2.59 (1.17) | 2.94 (1.5) | 0.311 |
| SBP, mmHg | 137 (20.72) | 139 (22.73) | 0.732 |
| DBP, mmHg | 73.61 (12.40) | 68.82 (14.46) | 0.180 |
| Vd/Vt | 0.48 (0.09) | 0.65 (0.08) | <0.0001 |
SD: standard deviation of the mean; l/min: liters per minute; bpm: beats per minute; mmHg: millimeters of mercury; No.: number of patients; P ASB: pressure support; PaCO2: arterial carbon dioxide pressure; PAD: diastolic blood pressure; PaO2/FiO2: arterial oxygen pressure/inspiratory oxygen fraction ratio; PAS: systolic blood pressure; PEEP: positive end expiratory pressure; rpm: respirations per minute; Vd/Vt: dead space fraction; Mv: minute volume; Vte: expiratory tidal volume.
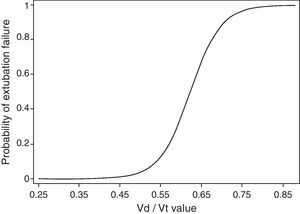
Logistic regression analysis was carried out, taking failed extubation as the dependent variable and examining the different variables which showed at least a tendency towards statistical significance in the univariate analysis (with a value of p<0.1). The analysis revealed a significant association between the variable Vd/Vt and extubation failure, with OR 1.53 (95%CI 1.12–2.09; p=0.001) (Table 5), for each 0.01 of Vd/Vt (Fig. 2). In the same analysis, the PaO2/FiO2 value was seen to exert a protective effect against extubation failure, with OR 0.96 (95%CI 0.93–0.99; p=0.04).
Results of the logistic regression analysis, taking failed extubation as the dependent variable and examining the different variables which showed at least a tendency towards statistical significance in the univariate analysis (p<0.1).
| Variable | Odds ratio | 95%CI | p |
| Hours on MV | 1.00 | 0.99–1.01 | 0.100 |
| fr/Vt | 0.89 | 0.73–1.08 | 0.264 |
| Heart rate | 1.01 | 0.95–1.08 | 0.690 |
| Respiratory frequency | 1.26 | 0.75–2.09 | 0.369 |
| Mv, l/min | 0.81 | 0.49–1.36 | 0.446 |
| PaCO2 | 1.05 | 0.83–1.33 | 0.652 |
| PaO2/FiO2 | 0.96 | 0.93–0.99 | 0.041 |
| Vd/Vt | 1.52 | 1.11–2.09 | 0.008 |
fr/Vt: respiratory frequency/tidal volume ratio; 95%CI: 95% confidence interval; l/min: liters per minute; mmHg: millimeters of mercury; PAD: diastolic blood pressure; PAS: systolic blood pressure; Vd/Vt: dead space fraction; MV: mechanical ventilation; Mv: minute volume.
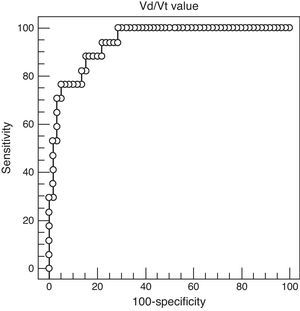
The area under the ROC curve (Fig. 3), with respect to the prediction of extubation failure based on the Vd/Vt value, was 0.94 (95%CI 0.86–0.98; p<0.0001).
The Vd/Vt cutoff value offering the best sensitivity and specificity was 0.58, with a sensitivity of 88.24% (95%CI 63.6–98.5) and a specificity of 84.75% (95%CI 73.0–92.8). The positive predictive value was 62%, with a negative predictive value of 96%.
DiscussionThe most important conclusion of the present study is the definition of the dead space fraction (Vd/Vt) as a potent predictor of mechanical ventilation as an extubation success.
However, the analysis made has a series of limitations. The main limitation may be the heterogeneity of the study sample, based on the disease leading to the indication of MV. Nevertheless, we consider that a non-selected population of patients in the GICU is the best way to reflect the daily clinical activity of many ICUs in our setting.
Two important aspects should be considered in this study. One aspect is the use of a low-level pressure support protocol. This choice was based on the fact that the latter afforded simple breathing, with unlimited flow upon demand, and allowed control of the patient inspiration index. Likewise, this type of protocol facilitated data measurement and registry, fundamentally of the variables obtained from the capnography sensor. We consider that the pressure support mode is comfortable for the patient and facilitates patient–ventilator synchronization. In addition, it is recognized as one of the weaning methods offering the best results.2–4
The second aspect requiring mention is the percentage of extubation failure observed in our series. In effect, the recorded 22% may be considered too high. However, as was commented in “Introduction” section, the poorest results correspond to the clinical and neurological cases, and these were the largest groups in our cohort. Moreover, it must be pointed out that extubation failure was considered not only when re-intubation proved necessary but also when there were clear and strict indications to the effect. In a meta-analysis of 2486 patients, the proportion of cases of failed weaning was found to be 31.2%, with a 13% re-intubation rate.21
The fact that Vd/Vt was seen to be a good predictor of extubation failure can be explained by its behavior as an indicator of the possible imbalance between the demand and the actual ventilation capacity of the patient. Ventilation demand depends not only on the ventilation requirements, but also on the respiratory system of each patient. Thus, when the MV needed to maintain normal alveolar ventilation exceeds the capacity of the patient, weaning will not be satisfactory.
These ventilation requirements are determined by VCO2, the dead space, and the respiratory stimulus at central nervous system level. Since Vd/Vt in a single parameter comprises two of the components that determine the ventilation requirements, its efficacy in predicting extubation failure can be explained.
However, the work of breathing (WOB) as another of the main determinants of ventilation demand or load has not been weighted in the measurement of Vd/Vt. The mechanical characteristics of the respiratory system, airway resistance and thoraco-pulmonary compliance determine WOB through its two components: resistive work and elastic work. In other words, situations of bronchospasm, upper airway obstruction, bronchial hypersecretion and certain characteristics of the external circuits of the ventilator that imply an important increase in resistive work by raising airway resistance are not contemplated by the Vd/Vt based prediction. The same applies to situations involving an increase in the elastic component of WOB (loss of compliance, effusion, pneumothorax, etc.).22
In the medical literature, the first investigations in relation to Vd/Vt date back to 196523 with studies of its role as a marker of acute lung injury (ALI). More recently, in 1983, Pierson24 identified values of Vd/Vt>60 as indicators of intubation. However, despite these old studies, Vd/Vt traditionally has not been included in the clinical guides as a parameter to be considered in the extubation of adults subjected to MV. This may be attributed to the complex task of collecting the measurements needed to calculate the fraction, before technological advances simplified this work by introducing new ventilator and sensor measurement and calculation techniques.
Recently,25 emphasis has been placed on the role of Vd/Vt in predicting extubation. Based on a cohort of 35 patients, it has been postulated that the highest Vd/Vt values measured on the first day of hospitalization could be an early predictor of extubation failure. In this case, the sensitivity, specificity, positive predictive value, negative predictive value and a Vd/Vt cutoff point of ≥0.60 in predicting extubation failure according to the ROC curve were 70%, 72%, 58%, 81% and 71%, respectively.
In this same sense but with a different working philosophy we have the study published by Farah et al.,26 which attempts to clarify the effect of Vd/Vt in the weaning from MV of patients with COPD. On analyzing their registry of 49 patients, the authors concluded that Vd/Vt does not afford a reliable value in estimating the duration of MV in patients with acute respiratory failure due to COPD.
The studies with a methodology and physiological basis more akin to those of this article have been carried out in the pediatric setting. In this sense, Hubble et al.,20 in an analysis of 45 pediatric patients, found Vd/Vt values of ≤0.50 calculated 30min before extubation to be associated with success, while Vd/Vt>0.65 was identified with the need for additional respiratory support after extubation. For a cutoff point of Vd/Vt=0.50, the study showed a sensitivity of 0.75% and a specificity of 0.92%.
In contrast to the above are the results published by Bousso et al.19 in another pediatric study. In this case the Vd/Vt value obtained in the analysis of the ROC curve was found to be poor as a predictor of extubation failure (with an area under the curve (AUC) of 0.62). Using a cutoff point of 0.65 yielded no significant differences in the correlation of this point with the incidence of extubation success or failure, as established from the logistic regression analysis.
However, there are important differences between the two studies commented above, on considering the populations involved. The population in the study by Bousso et al. was younger (mostly neonates) and with greater lung damage prior to extubation, compared with the study published by Hubble et al. Accordingly, the younger the patients, the lesser their resistance to muscle fatigue, cough proves less effective, the patients are less able to eliminate secretions, and their airway is moreover narrower. All these characteristics are not quantified in the measurement of Vd/Vt.
Lastly, Mohr et al.27 studied Vd/Vt 24h before and after tracheotomy in 45 adults admitted to a surgical ICU. The authors concluded that MV weaning success or failure could not be predicted on the basis of the Vd/Vt value, since Vd/Vt did not vary following tracheotomy. In relation to this study, it must be mentioned that the patients were ventilated in intermittent mandatory ventilation (IMV) pressure support mode from the planning of tracheotomy, and that the values for calculating Vd/Vt were registered while the patients were being ventilated with a minimum prefixed Vt adjusted to body weight, and with pressure support according to the needs of the patient. We consider that the fact that the patients received ventilatory support apparently sufficient to maintain adequate alveolar ventilation may have masked the Vd/Vt values obtained in this study. Nevertheless, we consider that this study should be taken into account in that its conclusions are opposed to the data obtained in our own work.
On comparing the results obtained for Vd/Vt with the multiple predictors analyzed in the literature, we could rank the dead space fraction at a level comparable to the CROP index (compliance, respiratory rate, oxygenation and pressure) and the IWI (integrative weaning index). In this sense, the CROP index, developed by Yang and Tobin in a prospective study with a cutoff point of 13ml/rpm, yielded a positive predictive value and a negative predictive value of 0.71% and 0.70%, respectively. In turn, the IWI, studied by Nemer et al. and calculated as the product of static compliance and SaO2 divided by the Fr/Vt ratio, with a cutoff point of 25ml/cmH2O/FiO2 yielded a sensitivity of 0.97% and a specificity of 0.94% in predicting extubation failure.28,29 Undoubtedly, these values imply a very high level of success, though when extubation failure predictors are compared, not only the numerical values of the statistical analyses must be taken into account. In this field a very important consideration is the complexity of application, integration and interpretation of the values obtained. On the other hand, in calculating Vd/Vt, use of the CO2 sensor can be considered, as well as the conduction of arterial blood gas measurements—this being an already standardized and routine practice in ICUs of third-level hospitals. However, indices such as the CROP or IWI involve increased complexity of calculation, based on the integration of several formulas, with the added difficulty of measuring static compliance of the respiratory system in spontaneously breathing patients.30
Lastly, our analysis shows that improved patient oxygenation, as measured with the PaO2/FiO2 ratio, behaves as a protective factor against extubation failure. Our data are consistent with the literature. Thus, in the study of Khamiees et al.,31 involving a majority of clinical patients (89%), a PaO2/FiO2 ratio of between 120 and 150 predicted extubation success in four out of every 5 patients. Likewise, Krieger et al.32 found a PaO2/FiO2 ratio of 238 to have a positive predictive value of 90%.
It can be concluded that the present article is the first study in adults methodologically designed to determine whether Vd/Vt is a good predictor of extubation failure in patients subjected to at least 12h of MV in an ICU. Based on the results obtained, it can be affirmed that the dead space fraction (Vd/Vt) is a valid tool in support of the difficult task of deciding the best moment for extubation.
Conflicts of interestThe authors have no conflicts of interest to declare.
The authors wish to express deep gratitude for the support received from the medical, nursing and auxiliary personnel of the General Intensive Care unit of Marqués de Valdecilla University Hospital.
Please cite this article as: González-Castro A, et al. Valor de la fracción de espacio muerto (Vd/Vt) como predictor de éxito en la extubación. Med Intensiva. 2011;35:529–38.