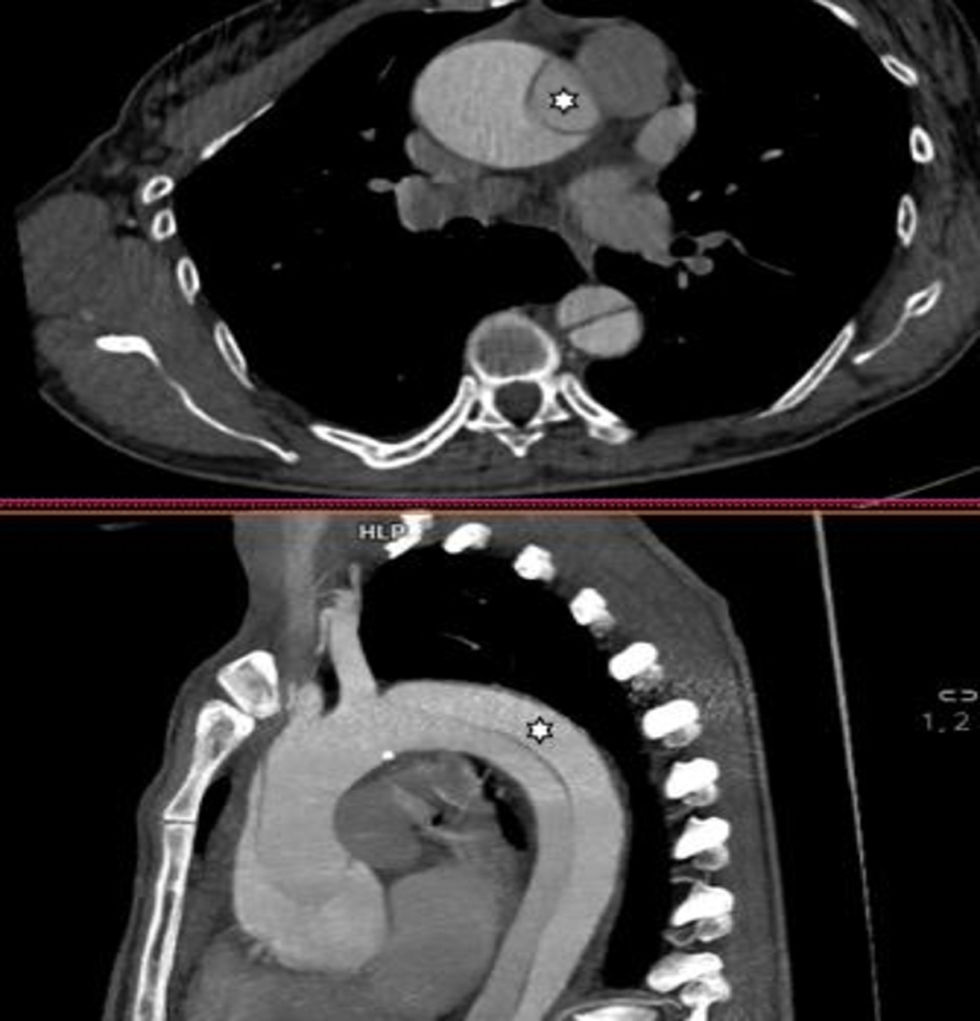
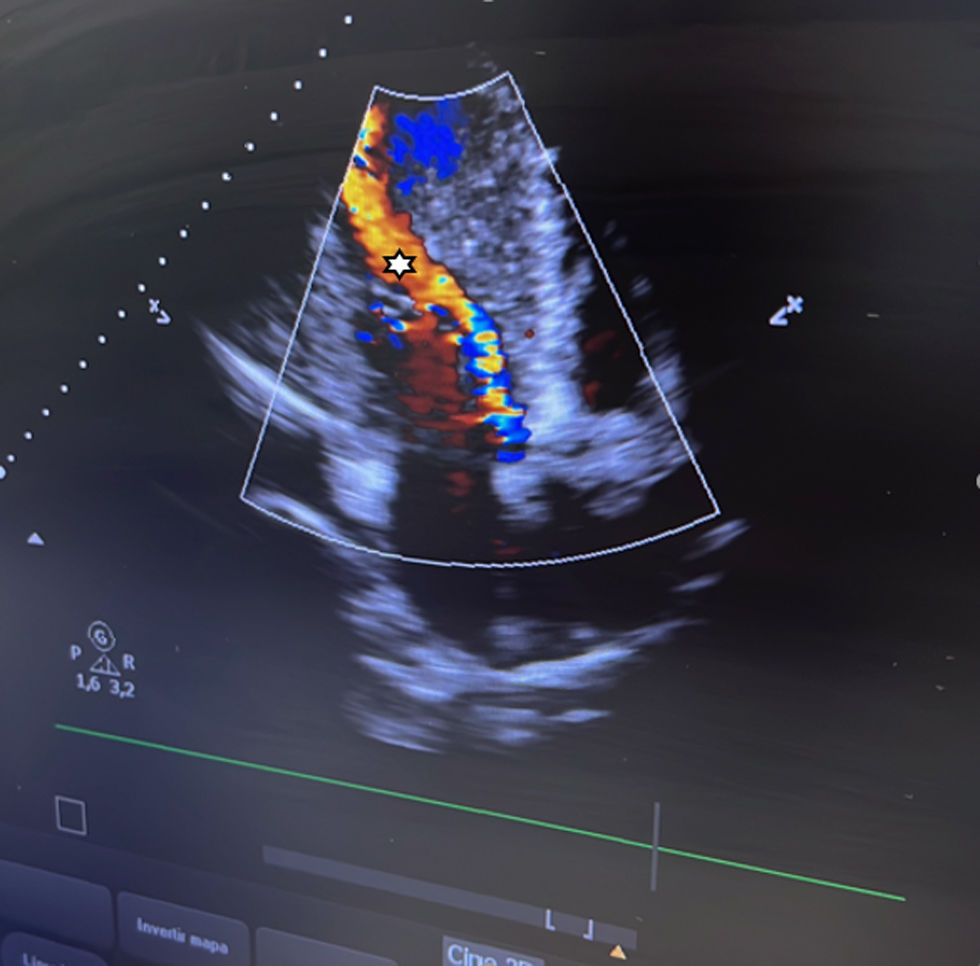
A 47-year-old woman with a past medical history of bicuspid aortopathy in her paternal grandfather; her parents died young in a traffic accident. Due to palpitations, the outpatient echocardiogram performed revealed the presence of a dilated ventricle with a left ventricular end-diastolic diameter of 71mm, indexed 3.4mm/m², left ventricular ejection fraction of 55–60%, in addition to a bicuspid aortic valve with fusion between the right and left coronary cusps that triggered severe aortic regurgitation (Fig. 2) with an aortic root of 40mm. A computed tomography scan was requested for preoperative study (Fig. 1), which was performed 3 weeks later, evidencing a Stanford/DeBakey type A aortic dissection I with an intimal flap at root level that extended longitudinally (Fig. 3) and spirally towards the left common iliac artery, involving the right brachiocephalic trunk without compromising its flow. In light of these findings, the patient was transferred to the cardiac intensive care unit for emergency surgery, undergoing David surgery with independent reimplantation of the brachiocephalic trunk.
FundingNone declared.
None declared.