Interfascial plane block of anterior and lateral cutaneous branches of intercostal nerves, known as pecto-intercostal fascial plane block (PIFB) and serratus–intercostal plane block (SIFB), is an anesthetic procedure for ribcage anesthesia not previously reported in the setting of critical care. A similar anesthetic technique has proven adequate pain control during and after abdominal and breast surgery.1–5
Patients with chest trauma and rib fractures or patients with endothoracic drainage tubes (EDTs) often need deep sedoanalgesia, hindering weaning. The use of ultrasound-guided interfascial plane block in critically ill patients opens up several possibilities to improve pain control, decreasing the need of other forms of conventional analgesia.
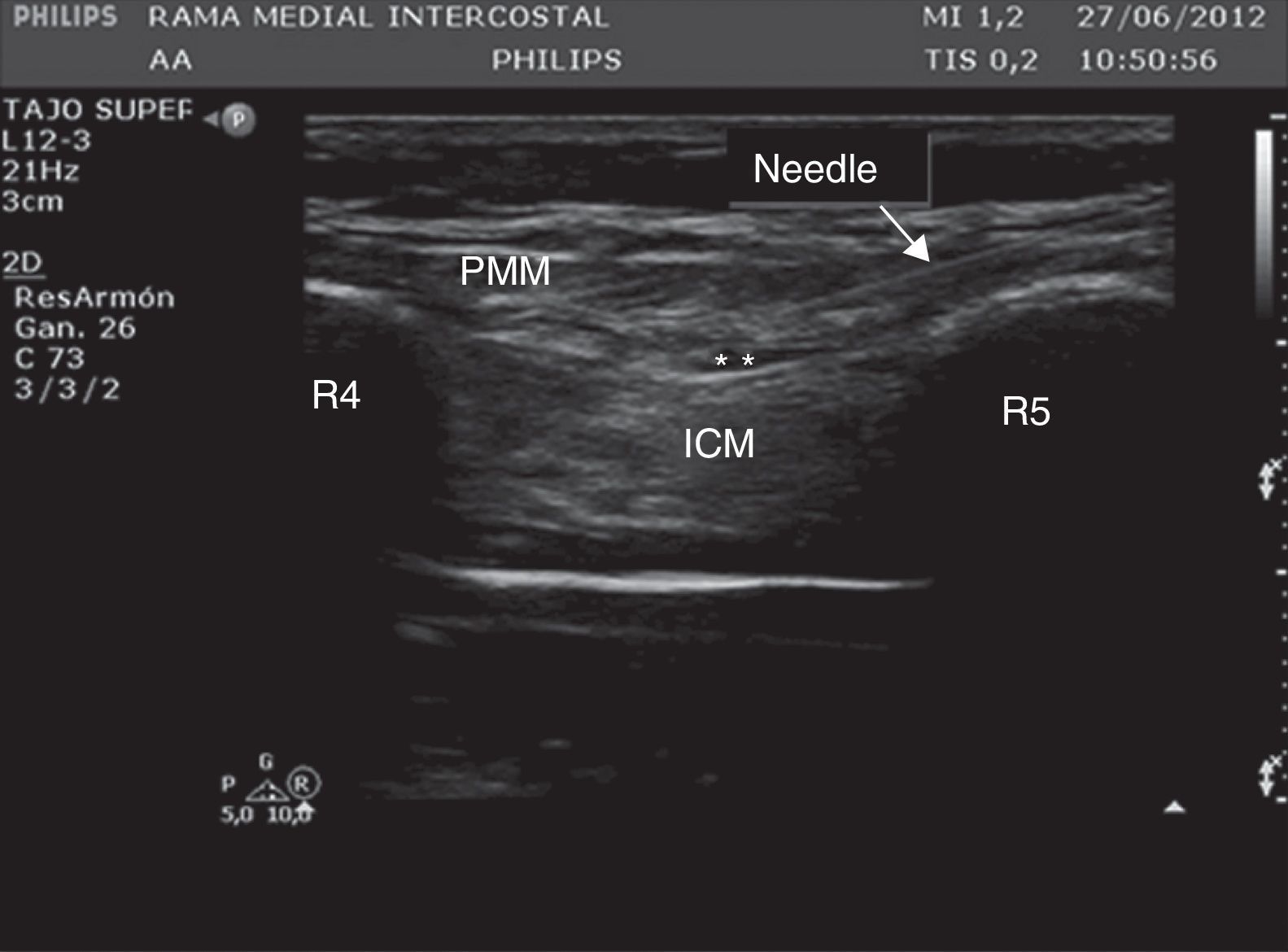
Description of interfascial plane blockFor carrying out PIFB a linear ultrasound (US) probe is placed at 2cm from the sternal body. On the surface plane, the subcutaneous tissue is identified, in the intermediate plane, the pectoralis major muscle, the intercostal muscles and the ribs, and in the deep plane, the pleura and the lungs (Fig. 1).
Ultrasound of the chest wall showing the structures visualized in the anterior chest. PMM: pectoralis major muscle; ICM: intercostal muscles; R4: fourth rib; R5: fifth rib; * denotes hydrodissection of the interfascial plane with the anesthetic solution inside this space. The arrow points the position of the needle crossing from the subcutaneous tissue up to the interfascial plane.
A needle is introduced following the lower edge of US probe, directing the tip from the bottom of the sternum and positioning the needle tip between the pectoralis major and the external intercostal muscles.
Twenty milliliters of a solution of 0.25% levobupivacaine plus epinephrine (5mcg/ml) are diluted in 250ml of 0.9% sodium chloride solution. Anesthetic boluses of 5ml are introduced to perform hydrodissection of the interfascial plane. The catheter must be allocated 3–5cm beyond the tip of the needle and is connected to an elastomeric pump, containing the anesthetic solution, at the infusion rate of 5ml/h.
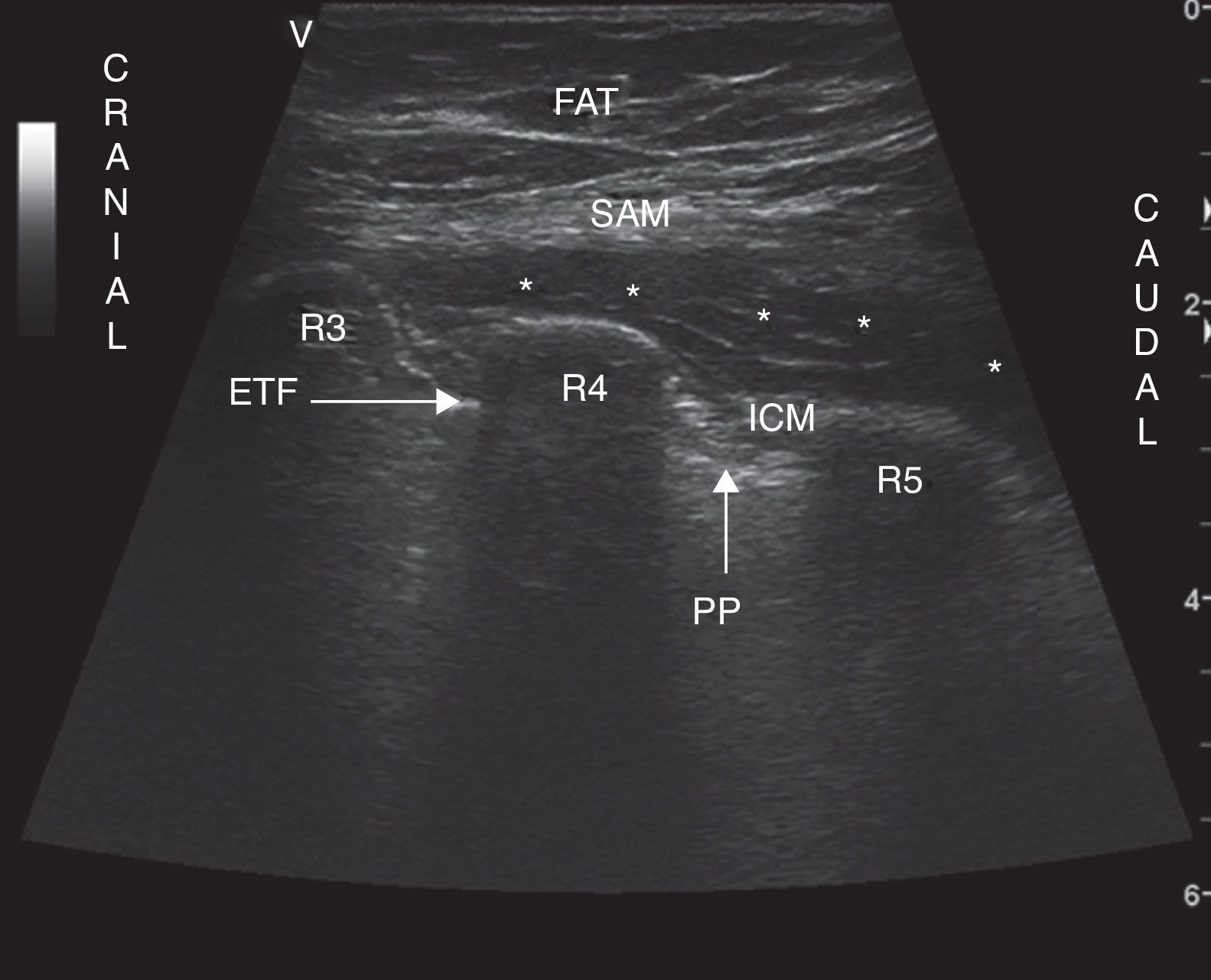
For SIFB, US probe is located on the lateral thoracic longitudinal axis, at the midaxillary line. On the surface plane subcutaneous tissue is identified, in the intermediate plane the anterior serratus muscle, the ribs and the intercostals muscles and in the deep plane the pleura and the lung. The needle is located between the serratus anterior muscle and the external intercostal muscle (Fig. 2). The needle is directed following the lower edge of US probe, from caudal to cranial, to locate it between the serratus anterior and the external intercostal muscles. Hydrodissection of the interfascial plane is made and 3ml of the anesthetic solution is administered for every segment desired to be blocked. The catheter is allocated 3–5cm beyond the tip of the needle and is connected to the elastomeric pump.
Ultrasound of the chest wall showing the planes visualized in the lateral chest. SAM: serratus anterior muscle; ICM: intercostal muscles; R3: third rib; R4: fourth rib; R5: fifth rib; PP: parietal pleura; ETF: enthoracic fascia; FAT: subcutaneous fat; * denotes hydrodissection of the interfascial plane with the anesthetic solution inside this space.
A 31-year-old man was admitted to the intensive care unit (ICU) due to severe community-acquired pneumonia and acute respiratory distress syndrome. Orotracheal intubation and prolonged mechanical ventilation were needed. Bilateral pneumothorax complicated respiratory progress. EDTs were placed on the left (lateral and anterior) and on the right (upper) chest.
When the weaning was thought to be suitable, three days after EDTs placement, sedoanalgesia with a morphine chloride infusion (0.42mcg/kg/min) and propofol (55.56mcg/kg/min) were needed because of severe ribcage pain when sedation windows were planned in multiple attempts of weaning. Sedative drugs hindered an adequate level of consciousness and collaboration for weaning.
PIFB was thought to be the best option for ribcage pain management. Five hours after the start of PIFB, intravenous sedative drugs were withdrawn and the patient could be extubated 1h later. The following days, the patient remained painless, not requiring any other analgesic. On the seventh day, PIFB catheters were removed. No germs grew in the cultures of catheters.
Case 2A 61-year-old man was admitted to the ICU after thoracic trauma. The patient showed fractures from the third to the eleventh ribs on the right thorax, fractures from the third to the twelfth ribs on the left thorax, fractures of the left L1–L4 transverse apophysis, fracture of the sacrum and fracture of the right iliac blade.
The patient required endotracheal intubation and mechanical ventilation due to respiratory failure, and surgery for pelvic external fixation. Sedoanalgesia with mizadolam (7.5mcg/kg/min) and morphine chloride (0.5mcg/kg/min of) was started.
Four days later, in anticipation of an expected difficult weaning, SIFB was performed on both hemithorax with an infusion of levobupivacain 0.0625% at a 10ml/h rhythm. The concentration of levobupivacain infusion was intentionally reduced, with an increased infusion rhythm (larger volume infused) to achieve a wider spread of the anesthetic, due to patient obesity (body mass index, 34.6). After 5h of levobupivacain infusion, midazolam and morphine chloride were withdrawn. Metamizol (2g/6h, IV) and paracetamol (1g/6h) were prescribed due to painful fractures outside the chest. Dipotassium clorazepate (20mg/8h, IV) and clonidine (300mg/8h, through the nasogastric tube) were initiated to prevent deprivation syndrome. Ninety hours after intravenous midazolam and morphine chloride were withdrawn, the patient was awake and collaborative. He showed no ribcage pain and he was extubated successfully in the first attempt. The patient denied ribcage pain after extubation, even with mobilizations.
Catheters were kept in place for ten days and its cultures were sterile.
CommentsPIFB and SIFB have not been described previously as anesthesia for critically ill patients.
In Case 1, PIFB was clearly effective for ribcage pain control, preventing prolonged weaning and avoiding the use of other analgesic drugs. In Case 2, anti-inflammatory drugs were added for pain due to pelvis and vertebral fractures. Anyway, the use of non-steroidal anti-inflammatory agents appeared to be insufficient for the control of pain after multiple and bilateral rib fractures. The patient could not be extubated before sedative drugs had no effects on consciousness; ribcage pain was not an obstacle for weaning after PIFB was initiated.
The patients we report were pain free even with cough and mobilization after PIFB and SIFB. Elastomeric pumps were changed every 48h. No significant increase in the nursing staff workload, compared to administration of intravenous analgesics, was needed.
Possible PIFB and SIFB indications in ICU may include chest trauma (sternum and/or ribs fractures), thoracic and heart surgery, EDT maintenance, etc.