To compare readmission rates to the intensive care unit (ICU) before and after the implementation of a rapid response team (RRT), and to identify risk factors for readmission.
DesignA quasi-experimental before–after study was carried out.
SettingA University Hospital.
PatientsAll patients discharged from the ICU from January to December 2008 (control group) and from January 2010 to December 2012 (intervention group).
InterventionImplementation of an RRT.
Main variables of interestThe data included demographic parameters, diagnoses upon admission, ICU readmission, APACHE II, SOFA, and TISS 28 scores, and routine daily assessment by an RRT of patients discharged from the ICU.
ResultsDuring the study interval, 380 patients were analyzed in the period prior to the implementation of the RRT and 1361 after implementation. There was a tendency toward decreased readmission rates one year after RRT implementation. The APACHE II score and SOFA score at ICU discharge were independent factors associated to readmission, as well as clinical referral to the ICU.
ConclusionsThe RRT intervention resulted in a sustained decrease in readmission rates one year after implementation of this service. The use of a specialized team in health institutions can be recommended for ICU survivors.
Comparar las tasas de reingreso en la UCI antes y después de la implementación de un equipo de respuesta rápida (RRT) e identificar los factores de riesgo para la readmisión.
DiseñoEstudio cuasiexperimental before-after.
LugarHospital universitario.
PacientesTodos los pacientes que fueron dados de alta de la UCI de enero a diciembre de 2008 (grupo control) y de enero 2010 a diciembre 2012 (grupo intervención).
IntervenciónImplementación de un RRT.
Principales variables de interésLos datos incluidos demográfica, los diagnósticos de ingreso, readmisión UCI, APACHE II, SOFA y TISS 28 puntuación y de evaluación de los pacientes dados de alta de la UCI por un TSR.
ResultadosDurante el período de estudio, 380 pacientes fueron analizados en el período anterior a la implementación de la RRT y 1,361 después de la implementación. Hubo una tendencia a disminuir las tasas de reingreso después de un año de la implementación de un RRT. APACHE II y SOFA de alta de la UCI fueron factores independientes asociados a la readmisión, así como lo tipo de paciente médico.
ConclusionesLa intervención del RRT resultó en una reducción sostenida de las tasas de reingreso un año después de la implementación de este servicio. El uso de un equipo especializado en instituciones de salud puede ser recomendado para los pacientes supervivientes de la UCI.
Despite the great advances in artificial support systems for organ dysfunction and failure, the resources available for health are limited. In this scenario the management of health care quality and optimization of available resources are essential factors for maintaining good health systems functioning.1
In order to evaluate health care quality in the field of intensive care, readmission is an indicator of great importance, since it applies both to patient safety and optimization of health resources.2 Identifying patients who have a higher risk for readmission and indicating the follow-up of a specialized team in the intensive care post-discharge period are useful tools in this context.3
The risk factors most often identified in the literature for readmission to the ICU are respiratory and cardiovascular dysfunctions at the time of discharge. The most frequent readmission diagnoses are hypoxic respiratory failure, inadequate bronchial toilet, gastrointestinal bleeding, neurological disorders, and sepsis.4
Patient follow-up by a specialized team in the post intensive care period in order to prevent readmissions resulted in reduced readmission rates in pediatric patients3; however, the results are conflicting for adult patients.5 An early proactive detection of severity called “ICU without walls” was able to decrease mortality in adult patients.6 Identifying the benefits of implementing a rapid response team and defining the scope of its activities in health institutions are critical factors for optimizing the cost-effective performance of this specialized team.
The aim of this study was to compare readmission rates in the ICU before and after the implementation of a Rapid Response Team and identify risk factors for readmission in these patients.
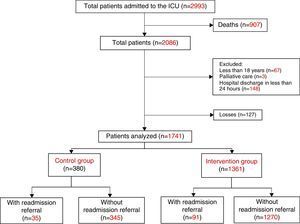
Patients and methodsThis quasi-experimental before–after study was conducted from January to December 2008 and January 2010 to December 2012 (before and after the implementation of the RRT, respectively) in a University Hospital. The study was conducted in a public university hospital with 330 beds, situated in the south of Brazil, serving a geographic region with an estimated population of 1,790,000 inhabitants. The ICU for adults consists of 20 beds, and had an occupancy rate above 95% throughout the study period. All consecutive patients who were discharged from the ICU during the study periods were included. Patients discharged in the first period of the study (January to December 2008) were considered as the control group. Patients discharged in the second period of the study, who were cared for by the RRT, were considered as the intervention group. Patients under the age of 18, in a palliative care condition at the time of ICU discharge, and those who were discharged from hospital less than 24h after ICU discharge were excluded.
General data were collected, such as gender, age, length of time in hospital and type of ICU referral classified as clinical or surgical according to Acute Physiology and Chronic Health Evaluation (APACHE II) definitions, trauma patients were classified as surgical if they were admitted to the ICU in the immediate post-operative period. Diagnosis at admission to the ICU, the ICU and hospital discharge dates, and the outcome on the date of discharge from the ICU and 30 days after discharge from the ICU were also collected.
The data collected during the ICU stay were: presence of chronic disease, need for mechanical ventilation, use of vasoactive drugs, and the APACHE II, Sequential Organ Failure Assessment (SOFA) and Therapeutic Intervention Scoring System (TISS 28) scores. The TISS 28 was denominated TISSa at the time of ICU admission and TISSd at discharge from the ICU. Other variables collected were the length of hospital stay and time in the ICU.
The RRT at the investigated institution was implemented in 2009 and was composed of an intensive care physician and physical therapist. The RRT operated in handling the requests for treatment of code events in the adult patient wards and also as an ICU-without-walls model.7 One of the functions of the RRT was the performance of daily assessments (in the morning and afternoon) of critically ill patients who were not admitted to the intensive care unit (ICU) due to lack of available beds. This activity was performed throughout the period that the patient waited for a vacancy until the transfer to the ICU or until the referral was cancelled for any reason. Another function of the RRT was to evaluate patients recently discharged from the ICU to prevent readmissions. Evaluation of the RRT performance to prevent readmissions was carried out by comparing the period prior to its implementation (January to December 2008) with the period one year after its implementation (January 2010 to December 2012). The sources used for data collection were the patient medical records and electronic database of the hospital. The calculation of the scores was performed according to the definitions of the respective systems.8–10
Readmission was defined as any patient who had a readmission referral to the ICU after discharge or during the same hospital stay, excluding those with new scheduled admissions due to elective surgical procedures. Readmissions were classified as a recurrence of the original disease, when the diagnosis of readmission was the same as the first admission, or as a new problem, if the diagnosis for readmission was different to the original disease. The readmissions were divided according to the time since the ICU discharge; up to 72h and over 72h.11 Chronic disease was defined according to the description of the Charlson comorbidity index.12
Continuous variables are expressed as mean and standard deviation or median and interquartile ranges. Categorical variables are expressed as absolute and relative frequency. The Student's t test or an equivalent non-parametric test (Mann–Whitney) was used for comparison of continuous variables. Categorical variables were compared using the chi-square test or Fisher's exact test. Bivariate analysis was performed to analyze predictors of outcome (readmission to the ICU). Multivariate logistic regression applying the stepwise forward method was used to assess factors that independently contributed to explain the outcome, the effect of each factor was expressed as an odds ratio (OR) and 95% confidence interval (CI 95%).
The area under the ROC (receiver operating characteristic) curve was calculated to evaluate the accuracy and compare the performance of the prognostic score in discriminating readmitted from non-readmitted patients. Hospital mortality was described as frequency and by the Kaplan–Meier survival curve. The significance level was set at 5% and analyzes were performed using the MedCalc program for Windows, version 15.2.2 (MedCalc Software, Mariakerke, Belgium).
EthicsThis study was approved by the local ethics committee for research involving human beings, No. 032/2013.
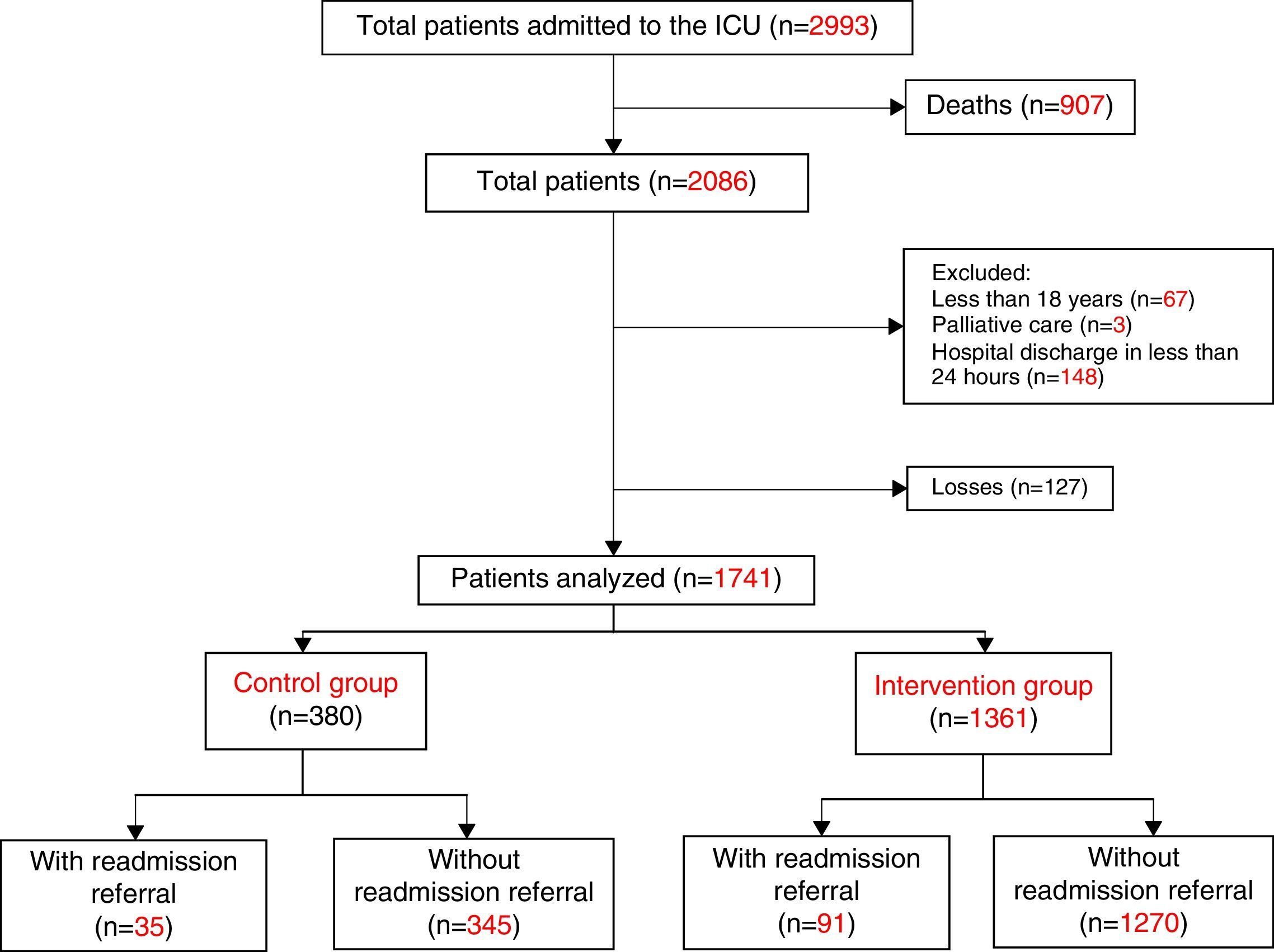
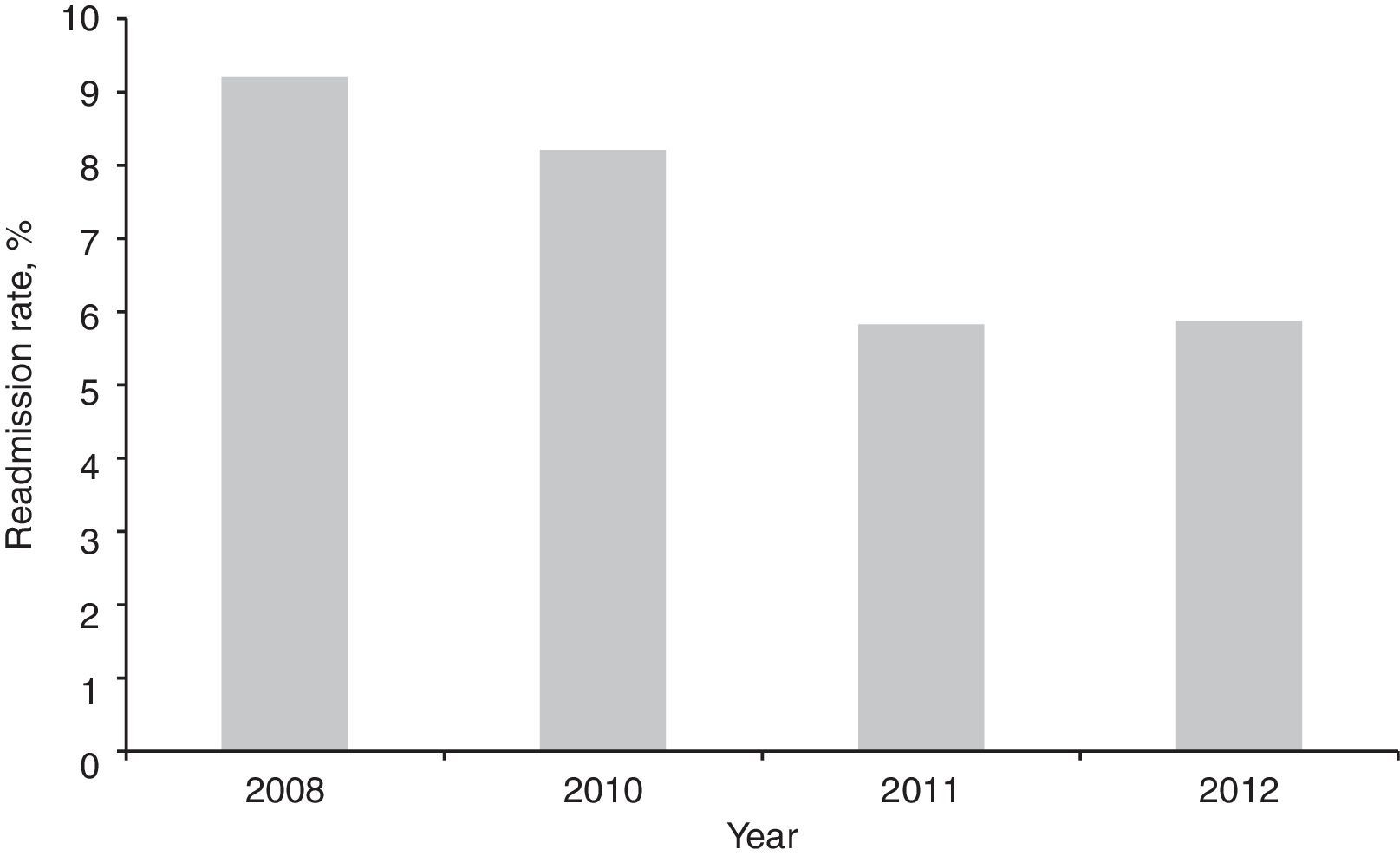
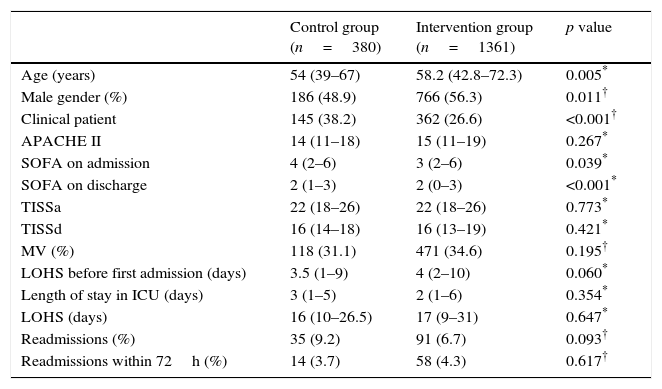
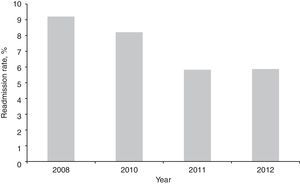
ResultsDuring the study period, 2993 patients were admitted to the ICU, of which 2086 were survivors at the time of discharge from this sector. Of these, 345 patients were excluded (16.5%) so that 380 patients were analyzed in the control group and 1361 patients in the intervention group (Fig. 1). Patients enrolled in both groups were similar regarding severity of illness evaluated by the APACHE II score, use of mechanical ventilation, and length of stay in the ICU. However, the groups presented differences regarding age, gender, and SOFA scores. Readmission rates for the entire hospitalization period tended to be lower in the intervention group (6.7%) compared with the control group (9.2%, p=0.093) (Table 1). When analyzing the annual readmission rates there was a decreasing trend in readmissions after 2011 in the intervention group (Fig. 2), that is, two years after implementation of the RRT.
Demographic and clinical characteristics of patients discharged from the Intensive Care Unit.
| Control group (n=380) | Intervention group (n=1361) | p value | |
|---|---|---|---|
| Age (years) | 54 (39–67) | 58.2 (42.8–72.3) | 0.005* |
| Male gender (%) | 186 (48.9) | 766 (56.3) | 0.011† |
| Clinical patient | 145 (38.2) | 362 (26.6) | <0.001† |
| APACHE II | 14 (11–18) | 15 (11–19) | 0.267* |
| SOFA on admission | 4 (2–6) | 3 (2–6) | 0.039* |
| SOFA on discharge | 2 (1–3) | 2 (0–3) | <0.001* |
| TISSa | 22 (18–26) | 22 (18–26) | 0.773* |
| TISSd | 16 (14–18) | 16 (13–19) | 0.421* |
| MV (%) | 118 (31.1) | 471 (34.6) | 0.195† |
| LOHS before first admission (days) | 3.5 (1–9) | 4 (2–10) | 0.060* |
| Length of stay in ICU (days) | 3 (1–5) | 2 (1–6) | 0.354* |
| LOHS (days) | 16 (10–26.5) | 17 (9–31) | 0.647* |
| Readmissions (%) | 35 (9.2) | 91 (6.7) | 0.093† |
| Readmissions within 72h (%) | 14 (3.7) | 58 (4.3) | 0.617† |
ICU – Intensive care unit; APACHE II – Acute Physiologic and Chronic Health Evaluation; SOFA – Sequential Organ Failure Assessment; TISS – Therapeutic Intervention Scoring System; TISSa – TISS score on admission to ICU; TISSd – TISS score on discharge from ICU; MV – mechanical ventilation; LOHS – length of hospital stay.
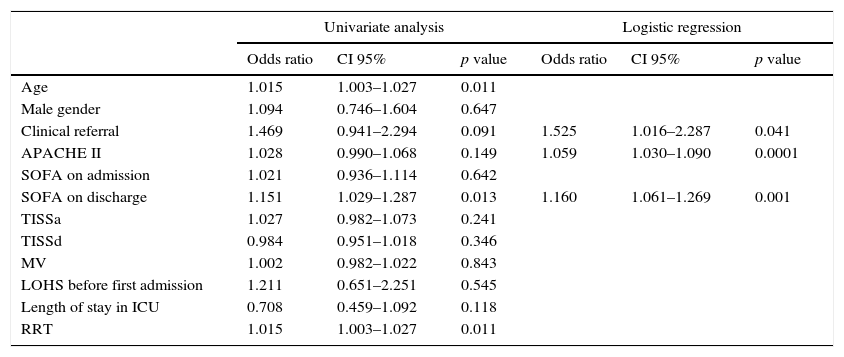
In the logistic regression model, clinical referral, APACHE II score, and SOFA on the day of ICU discharge were independently associated with readmission (Table 2). An ROC curve was performed for the APACHE II and SOFA on discharge considering a readmission referral to the ICU as the outcome. For the APACHE II the area under the curve was 0.683 with a cutoff point of 15 to predict readmission and respective sensitivity and specificity were (71.4% and 59.6%, p<0.0001). For the SOFA at discharge the area under the curve was 0.636 with a cutoff point of 2 to predict readmission and respective sensitivity and specificity were (57.1% and 69.1%, p<0.0001).
Univariate and multivariate* analysis of factors associated with readmission after discharge from the ICU.
| Univariate analysis | Logistic regression | |||||
|---|---|---|---|---|---|---|
| Odds ratio | CI 95% | p value | Odds ratio | CI 95% | p value | |
| Age | 1.015 | 1.003–1.027 | 0.011 | |||
| Male gender | 1.094 | 0.746–1.604 | 0.647 | |||
| Clinical referral | 1.469 | 0.941–2.294 | 0.091 | 1.525 | 1.016–2.287 | 0.041 |
| APACHE II | 1.028 | 0.990–1.068 | 0.149 | 1.059 | 1.030–1.090 | 0.0001 |
| SOFA on admission | 1.021 | 0.936–1.114 | 0.642 | |||
| SOFA on discharge | 1.151 | 1.029–1.287 | 0.013 | 1.160 | 1.061–1.269 | 0.001 |
| TISSa | 1.027 | 0.982–1.073 | 0.241 | |||
| TISSd | 0.984 | 0.951–1.018 | 0.346 | |||
| MV | 1.002 | 0.982–1.022 | 0.843 | |||
| LOHS before first admission | 1.211 | 0.651–2.251 | 0.545 | |||
| Length of stay in ICU | 0.708 | 0.459–1.092 | 0.118 | |||
| RRT | 1.015 | 1.003–1.027 | 0.011 | |||
CI 95% – confidence interval; APACHE II – Acute Physiologic and Chronic Health Evaluation; SOFA – Sequential Organ Failure Assessment; TISS – Therapeutic Intervention Scoring System; TISSa – TISS score on admission to ICU; TISSd – TISS score on discharge from ICU; MV – mechanical ventilation; LOHS – length of hospital stay.
Regarding the readmission diagnoses, 34 (27.0%) were considered as a recurrence of the original disease. Sixty-two patients (49.2%) were readmitted due to sepsis. Acute pulmonary edema, gastrointestinal bleeding, cardiopulmonary arrest, subarachnoid hemorrhage, pulmonary embolism, arrhythmia, and congestive heart failure were other reasons that led to readmission.
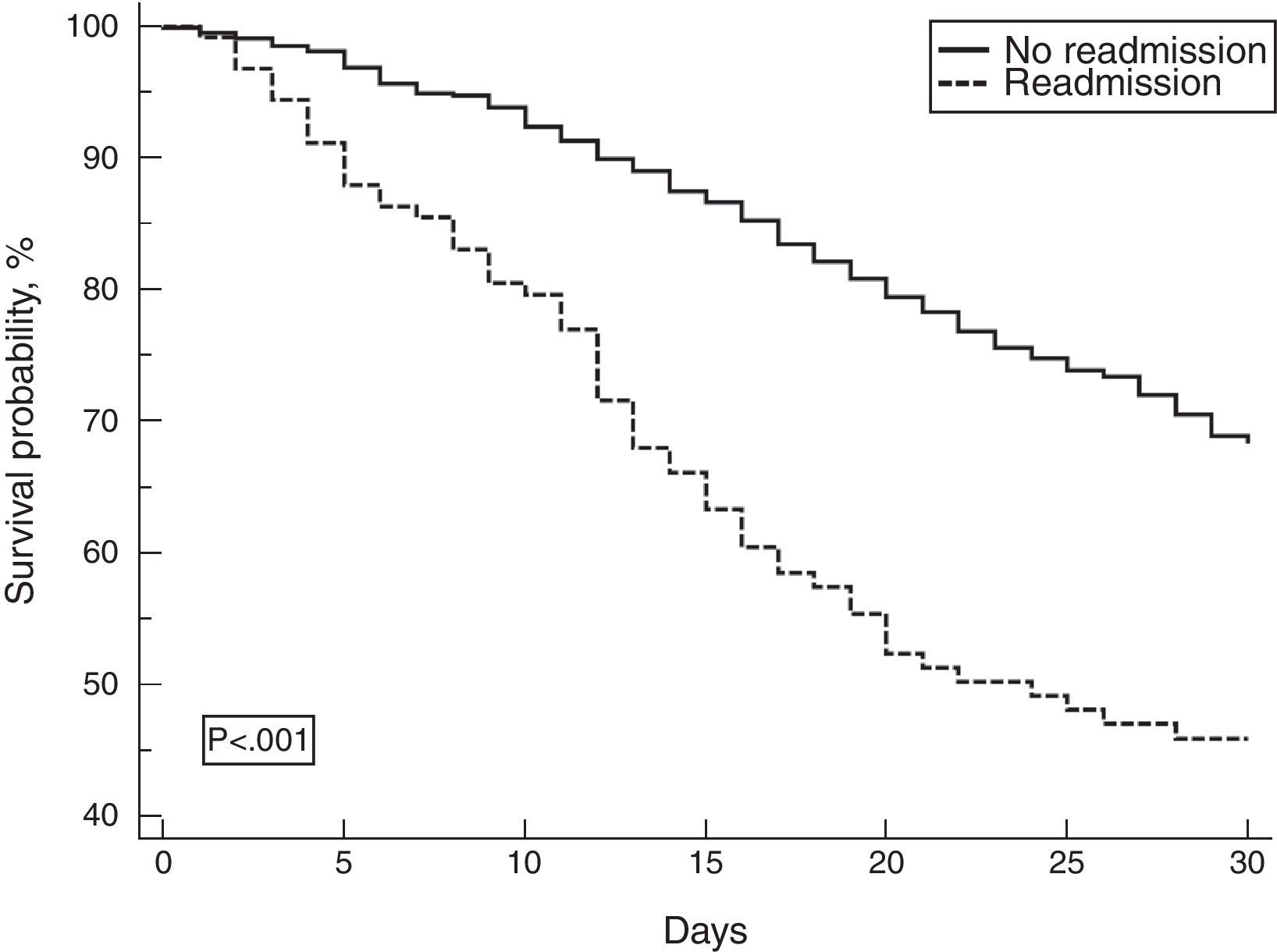
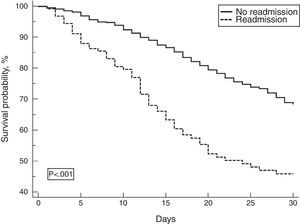
Mortality on the 30th day after ICU discharge was higher among readmitted patients compared with those not readmitted (47.6% vs. 8.5%, respectively; p<0.001) (Fig. 3).
DiscussionThis study compared the clinical outcomes of patients who were discharged from the ICU and assessed the impact of the introduction of an RRT to follow-up these patients. There was reduction in readmission rates one year after RRT implementation but no change in length of stay in the hospital or ICU. The independent risk factors for readmission to the ICU were APACHE II and SOFA scores and classification of patients as a clinical referral to the ICU.
Readmission rates are variable in the literature. They depend both on the definition of the time interval established, as well as the predominant characteristics of the service and patients studied. Some researchers have associated unexpected death within seven days of discharge from the ICU in the calculation of readmission rates, thus obtaining higher values.13 Some studies extend the definition of readmission to all unplanned readmissions to the ICU during the same hospital stay, while other publications consider a time interval of 48h after the ICU discharge.14 The results of the present study are consistent when compared with studies of a similar design.
Another consideration is related to the availability of intensive care beds. In the study by Wagner et al. involving more than 200,000 patients, the readmission rate was 3.9% with an average length of ICU stay of 48.8h when occupancy was high (95%), and 2.9% and 55.1h, respectively, when occupancy was low (5%), suggesting an increase in early ICU discharge and a consequent increase in readmissions in periods of low bed availability.15 The institution in the present study presented ICU occupancy rates above 95% during the study period, with longer stays in the ICU than described by other authors and readmission rates similar to the period of high occupancy. One possible explanation for this discrepancy is the absence of an intermediate care unit in the investigated hospital, delaying the discharge until the patient is able to be cared for in a low complexity unit and therefore with a low risk of readmission.
Factors associated with readmission to the ICU in the patients registered in the present study are consistent with the literature. In a review published by Rosenberg et al., in 2000, the main risk factors for readmission were respiratory disorders, including hypoxia and bronchial toilet difficulty, followed by cardiac abnormalities, gastrointestinal bleeding, and neurological disorders.3 Other studies have found the same diagnoses leading to readmission.16,17 In the present study, disease severity scores, such as the APACHE II and SOFA on the day of discharge, were different between readmitted and non-readmitted patients, as observed in other published studies.13,18 Despite the area under the curve revealing a poor discrimination ability to predict readmission, the cut off points could be of help to detect high risk patients and prevent readmissions.
The RRT intervention resulted in a reduction in readmission rates over time, one year after implementation of this service. The maturation period has proven to be important for assessing the effectiveness of rapid response systems. It is considered that the maturity of the entire system promotes heightened sensitivity, with recognition of the warning signs and more activations leading to better results and outcomes.19,20
Given the long term benefits demonstrated by the RRT in reducing readmission rates in the present study, we suggest that referral for RRT follow-up post ICU should be considered, especially for patients identified as higher risk.
There are limitations to be considered in the present study. As it was conducted in a single center, extrapolation of the findings should be performed with caution in populations with similar characteristics. The study aimed to evaluate several consecutive months to avoid seasonal bias. An analysis of the number of activations/admitted patients should be carried out to complement the data. In addition, the study was retrospective, with part of the data collected from medical records, which is prone to errors and data loss. The strength of this study lies in the fact that it is one of the few studies conducted in Latin America to describe readmission data and performance of a specialized team caring for patients after discharge from the ICU and using a score of therapeutic intervention.
ConclusionThe RRT intervention resulted in a sustained reduction in readmission rates one year after implementation of this service. The APACHE II score and SOFA on discharge from the ICU were independent factors associated with readmission, as well as clinical referral to the ICU. The use of a specialized team in health institutions is recommended for surviving patients from the ICU.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo funding to declare.
Contribution of the authorsPaula, RB: conception of the study, acquisition of data, drafting the article, final approval of the version to be submitted.
Tanita MT: analysis and interpretation of data, revising the article, final approval of the version to be submitted.
Festti, J: conception of the study, acquisition of data, revising the article, final approval of the version to be submitted.
Cardoso, LTQ: design of the study, analysis and interpretation of data, revising the article, final approval of the version to be submitted.
Grion, CMC: design of the study, analysis and interpretation of data, revising the article, final approval of the version to be submitted.
Conflict of interestNo conflict of interest to declare.