The COVID-19 pandemic challenged clinicians worldwide to treat a new and unknown disease. With more than 95 million confirmed cases since its beginning1, a lot of effort has been made to identify the best possible treatments.
The RECOVERY trial2 provides strong evidence in favor of the administration of 6mg of dexamethasone for ten days once a day in COVID-19 patients, if requiring at least oxygen supplementation (the incidence of death in the dexamethasone group compared to the usual care group was 23.3% vs 26.2% for patients receiving oxygen, and 29.3% vs 41.4% for patients under mechanical ventilation at the time of randomization). This finding changed the WHO therapeutic guidelines for patients with COVID-193 and triggered into clinicians the automatic binomial prescription: oxygen therapy-dexamethasone. In the current pandemic era, where everyone is searching for the magic bullet, and no clear evidence is available on any therapeutic agent capable to reduce mortality, having this option with such a familiar drug gave back to clinicians the feeling of having at least a weapon.
The trial findings were confirmed also in a recent meta-analysis4 including more than seven thousand patients: overall mortality was significantly lower in the corticosteroids group (26% vs 28%, relative risk {RR} = 0.89 [95% confidence interval {CI} 0.82-0.96], p=0.003). However, for COVID-19 patients not requiring oxygen the meta-analysis suggested an increase in mortality in patients receiving corticosteroids (17% vs 13%, RR = 1.23 [95% CI 1.00-1.62], p = 0.05).
The rationale for the use of dexamethasone is the mitigation of the inflammatory organ injury that may occur during SARS-CoV-2 infection. In the RECOVERY Trial the benefit of dexamethasone was indeed clear when inflammatory lung damage was more likely to be common, that is supposed to be in those patients treated “more than 7 days after symptom onset”. However, as mentioned by the authors of the trial, only a subgroup of severe COVID-19 patients showed significant elevation in inflammatory biomarkers (such as C-reactive protein and ferritin), and unfortunately the “inflammatory lung damage” was advocated but not assessed.
Beside the desired anti-inflammatory effect, dexamethasone is also known for its immunosuppressive properties, that can lower resistance to bacterial and viral infections through a cell-mediated mechanism. Although steroids were recently found not to affect time to negativization of nasopharyngeal swab in a cohort of 280 Italian patients5, the development of secondary opportunistic infections certainly remains a major issue, affecting patients’ outcome.
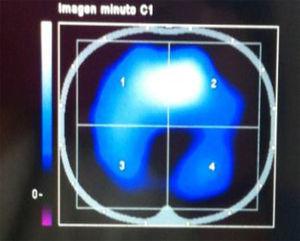
Furthermore, as well as corticosteroids increase mortality in patients not requiring oxygen therapy4, it is reasonable to think that their effect among patients requiring low flow oxygen could be mixed. As in a previous study6 that identified two different subphenotypes of acute respiratory distress syndrome, one of which was categorised by more severe inflammation, it is likely that also in COVID-19 patients different inflammatory patterns may occur. In support to this previous finding, a recent review and meta-analysis of COVID-19 studies focused on the role of cytokines and inflammatory biomarkers and found different mean levels of C-reactive protein between severe and critical COVID-19 patients (55.9μg/mL [CI 23.1-88.8μg/mL
Beyond the initial enthusiasm after the trial results, leading to an almost indiscriminate adoption of dexamethasone in COVID-19 patients, we suggest that a more personalized prescription would lead to further improvements in patients’ outcome. We think that, beside avoiding corticosteroids for patients not on oxygen, COVID-19 patients requiring oxygen should be screened for high or normal inflammatory biomarkers thresholds. Furthermore, for those patients who may benefit from corticosteroid treatment it is reasonable to investigate whether a higher or a lower dose of dexamethasone is most beneficial, and a clinical trial is currently ongoing randomising patients with severe hypoxia to receive either 6 or 12mg of dexamethasone.7
This would serve to target inflammation only in those patients who would probably benefit from its modulation, while removing the burden of corticosteroids side effects in those patients without an inflammatory pattern who would probably not benefit from this therapy.
Authors’ contributionsAll the authors have substantially contributed to the conception of the work, and to the drafting or revision; all the authors have approved the final version and agree to be accountable for all the aspects of the work.
Conflicto de interesesLos autores declaran no tener ningún conflicto de intereses.