To investigate the association between early blood pressure drop and worsening renal function (WRF) in ICU patients with liver failure and to evaluate their clinical outcomes.
DesignRetrospective observational study.
SettingIntensive Care Medicine.
PatientsPatients admitted to the ICU for the first time during their first hospitalization; diagnosed with liver failure according to the International Classification of Diseases, Ninth and Tenth Revision codes; and aged ≥18 years were included. Patients with a peak systolic blood pressure (SBP) drop of <0 mmHg were excluded.
InterventionWe analyzed data of ICU patients with liver failure from the Medical Information Mart for Intensive Care IV version 2.2 database. Descriptive statistics, analysis of variance, Kruskal–Wallis test, and chi-square test were employed for analysis. Multivariate linear regression models were used to assess the determinants of blood pressure decline. Cox proportional hazards and generalized additive models were used to evaluate
Main variables of interestThe relationship between blood pressure decline, WRF, and 60-day in-hospital mortality were evaluated, along with subgroup analyses.
ResultsPeak SBP drop was independently associated with higher risks of WRF (P < 0.001) and 60-day in-hospital mortality (P < 0.001), even after adjusting for potential confounders, including baseline SBP. The independent risk relationship observed between peak diastolic blood pressure, mean arterial pressure drop, and the occurrence of WRF and 60-day in-hospital mortality was similar.
ConclusionsIn ICU patients with liver failure, a significant early drop in blood pressure was associated with a higher incidence of WRF, increased risk of 60-day in-hospital mortality, and poorer prognoses.
Investigar la asociación entre los descensos precoces de la presión arterial y el empeoramiento de la función renal (EFR) en pacientes de la UCI con insuficiencia hepática y evaluar sus resultados clínicos.
DiseñoEstudio observacional retrospectivo.
ÁmbitoMedicina Intensiva.
PacientesSe incluyeron los pacientes ingresados en la UCI por primera vez durante su primera hospitalización, diagnosticados de insuficiencia hepática según los códigos de la Clasificación Internacional de Enfermedades, Novena y Décima Revisión, y con una edad ≥18 años. Se excluyó a los pacientes con un descenso máximo de la PAS < 0 mmHg.
IntervenciónSe analizaron los datos de los pacientes de la UCI con insuficiencia hepática de la base de datos Medical Information Mart for Intensive Care IV, versión 2.2. Para el análisis se emplearon estadísticas descriptivas, análisis de varianza, prueba de Kruskal–Wallis y prueba de ji-cuadrado. Se utilizaron modelos de regresión lineal multivariante para evaluar los factores determinantes del descenso de la presión arterial. Se utilizaron modelos de riesgos proporcionales de Cox y modelos aditivos generalizados para evaluar. Se utilizaron modelos de riesgos proporcionales de Cox y modelos aditivos generalizados para evaluar.
Variables de interés principalesSe evaluó la relación entre el descenso de la presión arterial, el EFR y la mortalidad intrahospitalaria a los 60 días, junto con análisis de subgrupos.
ResultadosEl descenso máximo de la presión arterial sistólica (PAS) se asoció de forma independiente con mayores riesgos de EFR (p < 0,001) y mortalidad intrahospitalaria a los 60 días (p < 0,001), incluso tras ajustar por posibles factores de confusión, incluida la PAS basal. La relación de riesgo independiente observada entre la presión arterial diastólica máxima, la caída de la presión arterial media y la aparición de EFR y mortalidad hospitalaria a los 60 días fue similar.
ConclusionesEn los pacientes de la UCI con insuficiencia hepática, una caída precoz significativa de la presión arterial se asoció con una mayor incidencia de EFR, un mayor riesgo de mortalidad intrahospitalaria a los 60 días y un peor pronóstico.
Liver failure is a severe condition characterized by extensive hepatocyte damage, leading to the loss of liver function.1,2 This condition can precipitate multi-organ dysfunction and life-threatening complications. Worsening renal function (WRF) is a common complication observed in patients with liver failure receiving treatment in intensive care units (ICU).3 The renal system is the most frequently affected organ/system in the context of multi-organ failure in patients with liver failure, with approximately 56% of patients experiencing renal impairment.4,5 WRF in this population is associated with elevated mortality rates and an increased chronic kidney disease risk.6 As a result, the early identification and prevention of liver failure in ICU patients at risk of WRF hold significant clinical importance.
In patients with liver failure, structural changes and distortion in the liver can increase intrahepatic vascular resistance. This leads to the release of potent vasodilators, triggering systemic arterial vasodilation, resulting in inadequate arterial filling and reduced renal blood flow.7,8 Liver failure is characterized by dilation of visceral arterial vessels, leading to a decrease in systemic vascular resistance.9,10 This can increase the synthesis of vasodilators, resulting in more pronounced vasodilation that cannot be compensated for by an increase in cardiac output (CO).11 A reduction in the effective blood volume within the systemic circulation may lead to decreased intravascular blood volume, potentially resulting in decreased renal blood flow. Ultimately, these hemodynamic changes within the kidneys and alterations in renal autoregulation may contribute to WRF.12 Moreover, during liver failure, the activation of systemic vasoconstrictor systems—including the renin-angiotensin-aldosterone system, sympathetic nervous system, and vasopressin— can induce renal vasoconstriction. This occurs even in the presence of an elevated CO, further contributing to WRF.13 Studies suggested that the primary cause of acute kidney injury (AKI) in patients with liver cirrhosis is hypovolemia (∼50%), resulting in reduced perfusion. This is followed by intrinsic renal factors such as acute tubular necrosis (∼30%) and hepatorenal syndrome (∼20%).6,14 The relationship between early blood pressure decline and WRF has been moderately studied in patients with acute heart failure (AHF). WRF in hospitalized patients with AHF is associated with adverse clinical outcomes and can be predicted by a decline in systolic blood pressures (SBP).15 Notably, a pronounced early SBP decline is associated with increased WRF, worsening heart failure, and increased cardiovascular mortality risk at 180 days. Interestingly, the relationship between SBP decline and prognoses remains consistent, irrespective of the WRF presence.16 To date, no studies have investigated the prognostic implications of early blood pressure decline—encompassing SBP, diastolic blood pressure (DBP), and mean arterial pressure (MAP)—and its association with WRF in ICU patients with liver failure, despite the concurrent occurrence of these events.
Therefore, the present study aimed to investigate the relationship between early blood pressure decline and WRF, as well as the clinical outcomes in ICU patients with liver failure. The findings of this study are expected to contribute to the early identification and intervention of WRF in ICU patients with liver failure, providing a scientific basis for clinical management strategy development and potentially improving patient prognoses.
Patients and methodsData sourceThis study used the Medical Information Mart for Intensive Care IV (MIMIC-IV) version 2.2 database. MIMIC IV is a large-scale clinical database that includes the detailed medical records of tens of thousands of ICU patients.17 Access to this database can be obtained through legitimate channels, and detailed information can be found on its official website (https://mimic.mit.edu).
Study populationAll patients in the MIMIC IV database were included in the study. The inclusion criteria were as follows: (1) admission to the ICU for the first time during their first hospitalization; (2) diagnosis of liver failure according to the International Classification of Diseases (ICD), Ninth Revision (ICD-9), and Tenth Revision (ICD-10) codes. (Table S1); and (3) age ≥18 years. Patients with a peak SBP drop of <0 mmHg were excluded.
Data extractionWe extracted demographics, comorbidities, vital signs, and laboratory results from the MIMIC IV database using Structured Query Language and tools such as Navicat. Comorbidities were identified through ICD-9/10 codes (Table S1). The following tables from the MIMIC IV database were used: "diagnoses_icd," "labevents," "patients," "chartevents," and "ICUstays." The average blood pressure value measured within the first hour after ICU admission was taken as the baseline SBP. The recorded creatinine value at the first monitoring after ICU admission was considered the baseline creatinine level. Additionally, the average of the highest and lowest laboratory indices values obtained within 24 h after ICU admission were used to determine the baseline values for laboratory indices.
Exposure and outcomesPeak SBP drop was defined as the difference between the baseline and the lowest values recorded within the first 48 h of the study period.16 For example, if the baseline SBP was 150 mmHg and the lowest SBP within 48 h was 125 mmHg, the drop in peak SBP would be 25 mmHg (not −25 mmHg). WRF was defined as an increase in serum creatinine levels by ≥0.3 mg/dL from baseline to any point on day 5.15 Sixty-day in-hospital survival was defined as the duration between admission to the ICU and either in-hospital death or loss to follow-up at the study’s conclusion, whichever happened first.
Statistical analysisBaseline characteristics were summarized according to the peak SBP drop tertiles within the first 48 h of the study period. Normally distributed data are presented as means ± standard deviations, skewed variables as medians (interquartile ranges), and categorical variables as frequencies (percentages). Analysis of variance was used for normally distributed variables, the Kruskal-Wallis test was used for skewed variables, and the chi-squared test was used for categorical variables.
To evaluate the determinants of peak SBP decline, a multivariate linear regression model was developed to assess the decline in SBP within 48 h using baseline clinical characteristics and routine laboratory parameters of the patients.
Cox proportional hazard models were constructed to determine the relationship between peak blood pressure decline and both WRF and 60-day in-hospital mortality. In the multivariate models, adjustment for covariates was performed by introducing covariates into the baseline model or excluding covariates from the full model if they induced more than 10% alteration in the regression coefficient of the independent variable.
A generalized additive model was used to explore the potential nonlinear relationship between the peak blood pressure drop and WRF. Hierarchical Cox regression models were used for subgroup analyses, and likelihood ratio tests were conducted to evaluate the interactions among the subgroups. Kaplan–Meier curves were analyzed using the log-rank test. Statistical analyses were performed using the R version 4.3.2 (http://www.R-project.org). The two-sided significance level was set at 0.05.
ResultsPatient characteristicsAmong the 1,062 patients with liver failure who were admitted to ICUs for the first time, 1,039 adult patients experienced an early drop in peak SBP, and these patients were included in the final cohort of this study. The patient screening process is illustrated in Fig. 1. Baseline characteristics and outcomes are succinctly encapsulated according to peak SBP decrease tertiles within the MIMIC IV dataset, as delineated in Table 1. Compared to patients in the low tertile, those in the high tertile of peak SBP drop were more likely to exhibit the following characteristics: heart failure; older age; rapid respiratory rate; elevated heart rate; higher baseline SBP, DBP, and MAP levels; increased levels of alanine aminotransferase, lactate dehydrogenase, potassium, and sodium; lower levels of alkaline phosphatase, and total bilirubin; and a higher risk of developing WRF. Additionally, they had a higher mortality rate (60 days) during their hospital stays.
Baseline characteristics of patients stratified by peak SBP drop tertiles (within first 48 h).
| Characteristics | Peak SBP Drop Tertiles | P-value | ||
|---|---|---|---|---|
| Low tertile (0−23 mm Hg) (N = 331) | Medium tertile (23−39 mm Hg) (N = 354) | High tertile (39−140 mm Hg) (N = 354) | ||
| Age (y) | 58.0 ± 15.3 | 60.4 ± 14.8 | 62.2 ± 15.0 | 0.002 |
| Sex (Male) | 200 (60.4%) | 221 (62.4%) | 211 (59.6%) | 0.731 |
| BMI (kg/m2) | 30.5 ± 6.5 | 30.3 ± 6.9 | 30.4 ± 7.4 | 0.960 |
| Race | 0.066 | |||
| White | 205 (61.9%) | 210 (59.3%) | 189 (53.4%) | |
| Other | 126 (38.1%) | 144 (40.7%) | 165 (46.6%) | |
| Laboratory parameters | ||||
| INR | 1.8 (1.4−2.4) | 1.8 (1.4−2.3) | 1.8 (1.4−2.4) | 0.283 |
| ALT (U/L) | 88.0 (30.0−468.2) | 80.8 (30.1−352.2) | 117.5 (35.1−581.9) | 0.041 |
| ALP (U/L) | 123.5 (82.2−184.0) | 114.8 (76.0−172.3) | 108.0 (74.8−159.8) | 0.013 |
| AST (U/L) | 192.0 (69.5−883.8) | 170.8 (65.0−629.4) | 237.8 (71.2−927.1) | 0.123 |
| LDH (U/L) | 546.0 (310.5−1111.4) | 498.3 (325.7−900.4) | 654.5 (353.3−1334.3) | 0.005 |
| Total bilirubin (mg/dL) | 3.0 (1.2−8.2) | 2.7 (1.0−6.8) | 2.0 (0.9−5.1) | 0.012 |
| BUN (mg/dL) | 30.5 (17.5−48.5) | 29.5 (17.0−50.5) | 29.5 (18.0−46.9) | 0.558 |
| Creatinine (mg/dL) | 1.5 (0.9−2.7) | 1.4 (1.0−2.4) | 1.7 (1.1−2.6) | 0.306 |
| Potassium (mmol/L) | 4.4 ± 0.8 | 4.4 ± 0.8 | 4.6 ± 0.8 | <0.001 |
| Sodium (mmol/L) | 136.6 ± 6.2 | 137.5 ± 6.0 | 138.0 ± 6.4 | 0.015 |
| Vital signs | ||||
| Respiratory rate (breaths/min) | 19.9 ± 4.6 | 20.6 ± 4.7 | 21.4 ± 5.1 | <0.001 |
| Heart rate (beats/min) | 89.9 ± 16.7 | 91.1 ± 17.4 | 94.2 ± 18.9 | 0.004 |
| Temperature (℃) | 36.8 ± 0.6 | 36.8 ± 0.7 | 36.8 ± 0.9 | 0.533 |
| SPO2 (%) | 96.2 ± 3.5 | 96.5 ± 2.9 | 96.1 ± 3.8 | 0.159 |
| Coexisting illness | ||||
| Hypertension | 88 (26.6%) | 108 (30.5%) | 97 (27.4%) | 0.480 |
| Diabetes mellitus | 83 (25.1%) | 109 (30.8%) | 86 (24.3%) | 0.105 |
| Heart failure | 79 (23.9%) | 91 (25.7%) | 117 (33.1%) | 0.017 |
| CKD | 56 (16.9%) | 72 (20.3%) | 82 (23.2%) | 0.126 |
| Respiratory failure | 177 (53.5%) | 192 (54.2%) | 204 (57.6%) | 0.503 |
| Baseline SBP (mmHg) | 103.3 ± 15.0 | 114.6 ± 14.4 | 129.4 ± 24.5 | <0.001 |
| Baseline DBP (mmHg) | 61.8 ± 13.3 | 66.7 ± 13.0 | 73.7 ± 19.6 | <0.001 |
| Baseline MAP (mmHg) | 75.6 ± 12.4 | 82.7 ± 11.8 | 92.3 ± 19.0 | <0.001 |
| WRF through day 5 | 143 (43.2%) | 172 (48.6%) | 198 (55.9%) | 0.004 |
| Death through day 60 | 112 (33.8%) | 142 (40.1%) | 181 (51.1%) | <0.001 |
SBP, systolic blood pressure; BMI, body mass index; INR, international normalized ratio; ALT, alanine aminotransferase; ALP, alkaline phosphatase; AST, aspartate aminotransferase; LDH, lactate dehydrogenase; BUN, blood urea nitrogen; SPO2, oxygen saturation; CKD, chronic kidney disease; DBP, diastolic blood pressure; MAP, mean arterial pressure; WRF, worsening renal function.
Table S2 presents the factors associated with the peak SBP drop in the univariate and multivariate linear regression analyses. Within the multivariate linear regression analysis, baseline SBP emerged as the strongest predictor of a greater drop in peak SBP within 48 h. Other independent predictors of a greater SBP decrease included older age, elevated heart rate, increased respiratory rate, higher international normalized ratio (INR), respiratory failure, and elevated serum potassium levels.
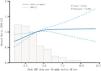
Relationship between SBP drop and WRFFigure S1 displays the survival curves of the WRF model stratified by the peak SBP drop tertiles within 48 h. The results indicated that patients in the high tertile of peak SBP drop were more likely to develop WRF. In the multivariate Cox regression analysis, accounting for potential confounders including baseline SBP (Table 2), a drop in peak SBP was positively associated with WRF (hazard ratio [HR]: 1.08 per 10 mmHg drop, 95% confidence interval [CI]: 1.03, 1.13). Within fully adjusted model 3, the HR and 95% CI for the high and middle tertiles with respect to dipped peak SBP were 1.63 (1.26, 2.10) and 1.26 (1.00, 1.59), respectively, compared to the low tertile (P for trend <0.001).We used generalized additive models to evaluate the relationship between the peak blood pressure drop and WRF (Fig. 2). This analysis showed a sustained positive correlation between early peak SBP, and WRF after adjusting for potential confounders with no threshold effect observed (P-nonlinear >0.05).
Association between peak SBP drop (per 10 mmHg) within 48 h from baseline and WRF.
| Exposure | Non-adjusted model | Model I | Model II | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Peak SBP drop (per 10 mmHg drop) | 1.05 (1.01, 1.09) | 0.011 | 1.15 (1.10, 1.20) | <0.001 | 1.08 (1.03, 1.13) | 0.003 |
| Peak SBP drop tertile | ||||||
| Low | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||
| Middle | 1.14 (0.92, 1.43) | 0.242 | 1.35 (1.07, 1.70) | 0.010 | 1.26 (1.00, 1.59) | 0.047 |
| High | 1.44 (1.16, 1.79) | <0.001 | 2.12 (1.66, 2.72) | <0.001 | 1.63 (1.26, 2.10) | <0.001 |
| P for trend | <0.001 | <0.001 | <0.001 | |||
Non-adjusted model considered: none.
Model I was adjusted for baseline SBP.
Model II was adjusted for age, sex, baseline SBP, total bilirubin, creatinine, potassium, respiratory rate, heart rate, and respiratory failure.
SBP, systolic blood pressure; WRF, worsening renal function; HR, hazard ratio; CI, confidence interval.
To examine the correlation between early peak SBP drop and WRF occurrence, we conducted subgroup analyses. Patients were stratified based on age, sex, race, body mass index (BMI), baseline blood pressure, and comorbidities to discern potential risk factors and identify any special population that might influence this association. The results from the subgroup analysis revealed no significant interaction between a greater drop in early peak SBP and a high risk for WRF across all subgroups (P > 0.05 for all interactions, Figure S2).
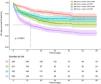
Relationship between SBP drop and prognosisTo determine whether the impact of greater SBP drops on prognosis is mediated by the occurrence of WRF, patients were categorized into four groups: peak SBP drop ≤ median without WRF (n = 294), peak SBP drop ≤ median with WRF (n = 221), peak SBP drop > median without WRF (n = 232), and peak SBP drop > median with WRF (n = 292). Kaplan-Meier curve analysis for 60-day in-hospital mortality showed significant differences among the groups, with increased mortality rates observed in patients with peak SBP drops above the median and in those with WRF (Fig. 3). In the adjusted Cox regression analysis (Table 3), a 10 mmHg decline in peak SBP correlated with a 14% rise in the 60-day in-hospital mortality risk (P < 0.001). Furthermore, we found that patients presenting with both WRF and an early peak SBP drops above the median exhibited the highest 60-day mortality risk (HR [95% CI] = 2.99 [2.21, 4.04], P < 0.001). This was followed by patients without WRF, yet with an early peak SBP drop above the median (HR [95% CI] = 2.29 [1.62, 3.22], P < 0.001), and lastly, patients with WRF and an early peak SBP drop at or below the median (HR [95% CI] = 1.34 [0.98, 1.83], P = 0.035).
Associations of SBP drops within 48 h with/without WRF and 60-day in-hospital mortality.
| Exposure | Non-adjusted model | Model I | Model II | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | |
| Peak SBP drop (per 10 mmHg drop) | 1.09 (1.05, 1.13) | <0.001 | 1.20 (1.14, 1.25) | <0.001 | 1.14 (1.09, 1.20) | <0.001 |
| Peak SBP drop median | ||||||
| SBP drop ≤ median without WRF | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | |||
| SBP drop ≤ median with WRF | 2.02 (1.49, 2.73) | <0.001 | 1.87 (1.38, 2.54) | <0.001 | 1.34 (0.98, 1.83) | 0.070 |
| SBP drop > median without WRF | 1.60 (1.17, 2.18) | 0.004 | 2.54 (1.81, 3.56) | <0.001 | 2.29 (1.62, 3.22) | <0.001 |
| SBP drop > median with WRF | 3.48 (2.65, 4.56) | <0.001 | 4.58 (3.46, 6.06) | <0.001 | 2.99 (2.21, 4.04) | <0.001 |
Non-adjusted model considered: none.
Model I was adjusted for baseline SBP.
Model II was adjusted for age, sex, baseline SBP, total bilirubin, creatinine, potassium, respiratory rate, heart rate, and respiratory failure.
SBP, systolic blood pressure; WRF, worsening renal function; HR, hazard ratio; CI, confidence interval.
To delve deeper into the correlation between early blood pressure decline and clinical outcomes among ICU patients with liver failure, we examined two other commonly utilized blood pressure parameters alongside SBP. After accounting for potential confounding factors, a decrease of 10 mmHg in the DBP was linked to an HR of 1.11 (95% CI: 1.02, 1.20; P = 0.013) for WRF, as well as an HR of 1.20 (95% CI: 1.10, 1.32; P < 0.001) for mortality within a 60-day hospitalization period. Similarly, a 10 mmHg reduction in the MAP was associated with an HR of 1.11 (95% CI: 1.04, 1.19; P = 0.004) for WRF, as well as an HR of 1.44 (95% CI: 1.34, 1.55; P < 0.001) for 60-day in-hospital mortality (Table S3).
DiscussionThis retrospective cohort study using the MIMIC-IV database found that for every 10 mmHg drop in early peak blood pressure (SBP, DBP, and MAP) in ICU patients with liver failure, the risk of developing WRF increased by 8%, 11%, and 11%, respectively. This correlation was independent of the patient's baseline clinical characteristics, including baseline blood pressure. In addition, a 10 mmHg drop in early peak blood pressure (SBP, DBP, MAP) was associated with a 14%, 20%, and 44% increased risk of 60-day hospital mortality, respectively. These findings underscore the importance of blood pressure monitoring and management in patients with liver failure. Clinicians should remain vigilant in identifying patients at risk of experiencing a substantial early drop in blood pressure, as this may indicate a higher likelihood of developing WRF and subsequent adverse outcomes. Strategies to prevent or mitigate this drop in blood pressure, such as optimizing fluid status and adjusting medication regimens, may improve patient outcomes.
In addition to examining the link between an early peak blood pressure drop and the risk and prognosis of WRF in ICU patients with liver failure, we identified independent predictors of an early drop in peak SBP. These factors included older age, increased respiratory rates, elevated heart rates, elevated INRs, elevated blood potassium levels, and concomitant respiratory failure. However, the strongest predictor of a drop in peak SBP is its baseline level. Our findings are consistent with those of previous studies concerning predictors of early SBP drop in patients with AHF, in which a higher baseline SBP was the strongest predictor.16,18,19 However, it is important to note that this finding may be attributed to "regression toward the mean" rather than specific pathophysiologic mechanisms, which makes predicting early SBP drops based on patient characteristics challenging.
Our subgroup analysis revealed a consistent association between an early drop in SBPs and the WRF risk across all subgroups (age, sex, BMI, race, baseline SBP, and comorbidities), indicating the stability of this relationship within each subgroup. Previous studies have indicated a significant positive correlation between baseline SBP and WRF risk. However, when considering these factors in a multivariate regression model, an early SBP drop, rather than baseline SBP levels, was independently linked to a higher risk of WRF.20 In our study, the connection between an early peak SBP drop and a heightened WRF risk persisted within the subgroups with higher baseline SBP and hypertension. This suggests that in clinical practice, a significant early drop in SBP should be avoided, even in patients with higher baseline SBP or concomitant hypertension in ICU patients with liver failure.
Portal hypertension is a key feature of disease progression in cirrhosis.21 A previous study by Garg et al. revealed that the baseline hepatic venous pressure gradient (HVPG) is a predictor of mortality in patients with acute-on-chronic liver failure, and that early elevation of portal pressure may increase the risk of variceal bleeding.22 Elevated portal pressures lead to systemic hemodynamic changes, such as increased CO, decreased peripheral vascular resistance, and a reduction in MAP. Our study showed that an early drop in blood pressure in ICU patients with liver failure was an independent predictor of 60-day hospitalization. A 10 mmHg decrease in early SBP, DBP, or MAP was associated with a 14%, 20%, and 44% increase in the risk of 60-day in-hospital mortality, respectively. Our findings suggest that an early blood pressure drop may serve as a more accessible and cost-effective predictor of prognosis than more complex measurements such as HVPGs. Early peak blood pressure drop measurements are readily available in clinical practice and can provide valuable information for risk stratification and prognostic assessment.23 Additionally, several studies have indicated that worse baseline renal function and AKI are independently associated with worse prognoses.24,25 Our study demonstrated that patients with a greater early drop in blood pressure and the development of WRF had the highest 60-day risk of in-hospital death, similar to previous studies. These findings present novel ideas for diagnostic and prognostic assessment. However, further validation and studies are warranted to confirm their clinical applications.
Our study has several strengths. First, this is the first study to explore the relationship between early blood pressure drops, WRF, and prognoses in ICU patients with liver failure. Furthermore, we investigated the associations between early DBP and MAP drops, WRF, and prognoses for the first time. Second, this study utilized data from the MIMIC IV database, offering the advantages of a large sample size and numerous blood pressure measurements taken at short intervals. Third, a subgroup analysis was conducted to examine the relationship between early blood drops and renal function deterioration in different subgroups. The results consistently demonstrated this association across various subgroups, thus enhancing the generalizability and applicability of the findings. Finally, the study was adjusted for potential confounding factors, including baseline blood pressure, to assess the independent correlation between early blood pressure drop and outcomes, thereby minimizing the impact of other factors and providing a more accurate estimation of the relationship.
Nonetheless, our study had some limitations. The included patients with liver failure were diagnosed using ICD-10 codes, which may have introduced bias in the available information about the liver failure cohort. Additionally, as this was a retrospective cohort study, a causal relationship between the early peak blood pressure drops and the occurrence and mortality rates of WRF could not be proven. Nevertheless, this large-scale cohort study utilizing a comprehensive database and multiple statistical methods demonstrated a correlation between early peak blood pressure drops and WRF, offering valuable clinical reference points. Finally, owing to the complex interactions between diseases, some confounding factors may still exist that could potentially mask or magnify the relationship between the study factors and the WRF.
ConclusionsOur findings suggest a significant association between an early drop in SBP, DBP, and MAP within the first 48 h and the development of WRF and 60-day in-hospital mortality among ICU patients with liver failure. In addition, early blood pressure drops and WRF development were associated with a poorer prognosis in patients with these risk factors, compared to other patients. However, further studies are needed to determine the causal relationship between blood pressure changes and renal function and its impact on prognoses.
CRediT authorship contribution statementRubing Guo: Writing – review & editing, Writing – original draft, Validation, Supervision, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. Jingjing Tong: Methodology, Investigation, Formal analysis, Conceptualization. Li Wang: Data curation. Bo Yang: Data curation. Liang Ma: Methodology. Yongtong Cao: Methodology. Wei Zhao: Methodology, Investigation, Formal analysis, Data curation, Conceptualization.
Consent for publicationNot applicable.
Ethics approval and consent to participateBecause our study was an independent research analysis of the already available MIMIC IV database, no approval was obtained from our local ethics committee, although it was reviewed and approved by the PhysioNet Review Board. The requirement for informed consent was waived owing to the retrospective nature of the study.
FundingThis work was supported by the National High Level Hospital Clinical Research Funding [grant number 2023-NHLHCRF-PY-04]; the Wu Jieping Medical Foundation [grant number 320.6750.2023-06-60]; and the Research Projects of Gansu Provincial Hospital [grant number 23GSSYD-25].
Availability of data and materialsThe present investigation utilized openly accessible datasets. The aforementioned data can be accessed via the following link. The MIMIC IV database (version 2.2) is publicly accessible at https://mimic-iv.mit.edu. Researchers who comply with the stipulated data utilization requirements are granted authorization to access these databases.
We extend our sincere gratitude to the team at the Laboratory for Computational Physiology (LCP) of the Massachusetts Institute of Technology (MIT) for providing the invaluable MIMIC-IV database. Their efforts have greatly facilitated our research in the medical field, and we truly appreciate their contributions.