Sepsis and septic shock continue to be the most frequent reason for admission to intensive care units, affecting millions of people around the world. Global incidence has been estimated between 250 and 500 cases/100.000 cases per year1 and can lead up to 6% of total hospital admissions only in the United States.2. Up to 51.1% require Intensive Care Unit (ICU) admission, reaching mortality rates of 30% and even 50% in cases of septic shock.3 Additionally, septic patients present short- and long-term complications, which lead to decreased quality of life and increased 5-year mortality.4 Our research group described an annual sepsis incidence in Catalonia of 264.1 per 100.000 inhabitants/year, and it increased every year, going from 144.5 in 2005 to 410.1 in 2019.5
In the constant search for a “cure” for sepsis, Marik et al. suggested that the early use of intravenous vitamin C, together with corticosteroids and thiamine, are effective in preventing progressive organ dysfunction, including acute kidney injury, and in reducing the mortality of patients with severe sepsis and septic shock.6 Despite the limitations of the study, their results and interesting pathophysiological argument, raised enough enthusiasm to put in motion several studies looking to reproduce his findings. Until today, there are no studies that support Dr Marik’s findings, and the use of vitamin C, corticosteroids and thiamine is not supported in current sepsis management recommendations.7
We performed a phase III, randomized, open, parallel group pilot study, which aimed to study 28-day mortality in patients with severe sepsis or septic shock treated according to current guidelines vs. patients treated with vitamin C, thiamine, and hydrocortisone added to usual treatment. As it was a pilot study, sample size calculation was not required; however, an N of 20 patients per group was expected for the time set for the study.
Subjects were patients with septic shock admitted to the ICU of 2 different hospitals in the same sanitary region that met the criteria to enter the study and signed the informed consent. Patients were randomized into a treatment and a control group. Randomization was aleatory, using the nQuery program.
Study was approved by the hospital’s ethics committee and registered in ClinicalTrials.gov (Identifier: NCT04111822). Reasons for exclusions were pregnancy, chronic use of vitamin C, thiamine or hydrocortisone, existing immunosuppression, and a defined limitation in ICU therapy upon intake.
Demographic data, sepsis biomarkers and other aspects of treatment were collected during the first 7 days, final outcomes were also included in the database.
The primary endpoint was 28-day mortality, and the secondary endpoints were number of ICU days, mechanical ventilation days and vasopressor dose.
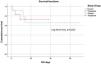
Descriptive statistics and comparative analyses between treatment vs. control group and survived and dead patients were made using the chi-square test, Student t-test or nonparametric estimation (Mann-Whitney U test), when appropriate. We designed Kaplan-Meier survival curves comparing treatment vs. control group. P value of <0.05 were considered statistically significant.
A total of 24 patients were included in the pilot study, unfortunately, by March 2020 the COVID-19 pandemic forced us to put the study on pause due to obvious reasons. By the time patient recruiting could be resumed, our preliminary analysis combined with the results of several studies, mainly the VICTAS,8 VITAMIN9 and the ACTS RCT10 led us to decide termination of the trial. This decision was based on the data of these studies and a preliminary analysis of our data that showed futility of the treatment. Trial termination was decided on what we mainly considered were ethical reasons.
Baseline characteristics were generally similar between the treatment group and the control group (Table 1). Six patients died (25%) during ICU stay, there was no statistically significant difference in the mortality between the treatment and the control group (Fig. 1), these results are similar to the ones of the ACTS RCT,10 and even though the VITAMINS RCT9 administered hydrocortisone to the control group, they also found no statistically significant differences in mortality between the two groups.
Participant characteristics (Treatment vs. Control group).
| Characteristics | Total (n = 24) | Treatment group(n = 12) | Control group(n = 12) | p |
|---|---|---|---|---|
| Age, mean, y (SD) | 64.8 (13) | 63.3 (11.3) | 66.3 (14.7) | 0.58 |
| Male, No. (%) | 13 (54) | 7 (58.3) | 6 (50.0) | 0.68 |
| Diabetes, No. (%) | 7 (29.2) | 3 (25) | 4 (33.3) | 0.65 |
| Hypertension, No. (%) | 16 (66.7) | 8 (66.7) | 8 (66.7) | 1 |
| Neoplasic disease, No. (%) | 4 (16.7) | 1 (8.3) | 3 (25) | 0.27 |
| COPD, No. (%) | 3 (12.5) | 1 (8.3) | 2 (16.7) | 0.53 |
| Obesity, No. (%) | 10 (41.7) | 5 (41.7) | 5 (41.7) | 1 |
| Diagnose No. (%) | ||||
| Pneumonia | 8 (33.3) | 6 (50) | 2 (16.7) | 0.26 |
| Abdominal sepsis | 5 (20.8) | 1 (8.3) | 4 (33.3) | |
| Urinary tract sepsis | 5 (20.8) | 2 (16.7) | 3 (25) | |
| Other | 6 (25) | 3 (25) | 3 (23) | |
| Clinical values, mean (SD) | ||||
| APACHE II score | 26.3 (16.1) | 28.7 (21.6) | 24 (8) | 0.48 |
| SAPS II score | 60.5 (20.4) | 61 (23.6) | 60 (17.7) | 0.29 |
| Initial SOFA score | 9.8 (2.1) | 9.8 (2.2) | 10 (2) | 0.85 |
| Lactate on admission, mg/dl | 27.4 (17.6) | 23.6 (16.8) | 31 (18.3) | 0.3 |
| Lactate 6 hours, mg/dl | 26.8 (19.1) | 28.3 (24) | 25.2 (13) | 0.7 |
| Lactate 24 hours, mg/dl | 26.6 (27.9) | 27 (33) | 26.2 (23) | 0.9 |
| Noradrenaline dose intake, mcg/k/min | 0.5 (0.5) | 0.5 (0.5) | 0.45 (0.42) | 0.55 |
| Noradrenaline dose day 3, mcg/k/min | 0.3 (0.4) | 0.4 (0.4) | 0.2 (0.3) | 0.48 |
| Noradrenaline dose day 7, mcg/k/min | 0.3 (0.5) | 0.4 (0.7) | 0.1 (0.1) | 0.29 |
| Urinary output day 1, L/24 hours | 1.4 (0.8) | 1.2 (0.8) | 1.7 (0.7) | 0.22 |
| PCR at intake, mg/dl | 41 (41.4) | 49.2 (57.5) | 32.8 (11.2) | 0.13 |
| PCR day 3, mg/dl | 26.1 (28.5) | 32.2 (39) | 20 (10.5) | 0.05 |
| Procalcitonin on admission, ng/ml | 26 (33.9) | 25.8 (37.3) | 31.7 (9) | 0.9 |
| Procalcitonin day 3, ng/ml | 13.6 (18.9) | 8.6 (9.6) | 19 (24.8) | 0.2 |
| Creatinine at intake, mg/dl | 1.8 (1.4) | 2.1 (2) | 1.4 (0.5) | 0.28 |
| Creatinine day 3, mg/dl | 1.4 (0.8) | 1.4 (0.8) | 1.4 (0.9) | 0.86 |
| Creatinine day 7, mg/dl | 1.1 (0.8) | 1.5 (1) | 0.7(0.5) | 0.09 |
| White blood cell count intake, 10³/mcl | 21.4 (11.3) | 16 (14.4) | 18.4 (10.7) | 0.65 |
| White blood cell count day 3, 10³/mcl | 17 (9.3) | 19.3 (10.6) | 14.7 (7.6) | 0.26 |
| White blood cell count day 7, 10³/ mcl | 18 (5.7) | 20.3 (5.6) | 15.8 (5.3) | 0.13 |
| Platelets on admission, 10³/ mcl | 202 (140.5) | 214 (180.8) | 189.8 (91) | 0.68 |
| Platelets day 3, 10³/ mcl | 174 (166.4) | 205 (223.6) | 142.6 (77.4) | 0.39 |
| Platelets day 7, 10³/ mcl | 260 (148.5) | 261.3 (183) | 259.1 (124.2) | 0.97 |
| Bilirubin on admission, mg/dl | 1.2 (1) | 1.3 (1) | 1.2 (1) | 0.86 |
| Bilirubin day 3, mg/dl | 0.7 (0.7) | 0.7 (0.7) | 0.7 (0.6) | 1 |
| Bilirubin day 7, mg/dl | 0.5 (0.2) | 0.45 (0.2) | 0.5 (0.3) | 0.36 |
| Dialysis, No. (%) | 8 (33.3) | 5 (41.7) | 3 (25) | 0.38 |
| Need of surgical procedure, No. (%) | 11 (45.8) | 2 (16.7) | 9 (75) | 0.00 |
| Mechanical ventilation, days (SD) | 14.5 (14.8) | 8.0 (7) | 22.3 (18.2) | 0.04 |
| ICU stay, days (SD) | 18.5 (13) | 12.3 (10) | 24.8 (23.5) | 0.11 |
| Hospital stay, days (SD) | 32 (30.5) | 24 (23.8) | 40.1 (35.3) | 0.2 |
| 28-day mortality, No, (%) | 6 (25) | 3 (25) | 3 (25) | 1.0 |
We also found no statistically significant difference in the decrease of vasopressor dose during the first 7 days of treatment, results that are equivalent to the ones of the VITAMINS (16) and the VICTAS8 studies. Patients on the control group required more surgical procedures than the treatment group: 75% vs. 16.7% (P = 0.00), given the number of patients of this study, we believe that this finding would probably disappear on a larger group.
Patients in the intervention group spent less time on mechanical ventilation than the control group. The mean number of mechanical ventilation days was 8.0 (SD 7.0) for the treatment group vs. 22.3 (SD 18.2) for the control group (P = 0.04). Other studies have found no statistically significant differences in mechanical ventilation free days, we consider that larger studies and larger samples have provided data that does not support this finding.
The authors consider that even though the results are similar to recent larger studies, they should not be considered comparable to them, because of the obvious limitations of our study. Even though our data showed a difference in mechanical ventilator days, we consider the sample was not big enough to make any affirmations and there are larger studies that did not find these differences.
In conclusion, in our series, the combination of intravenous vitamin C, thiamine and hydrocortisone compared to a control group did not show statistically significant differences in vasopressor dose or 28-day mortality in critically ill patients.
Conflict of interestThe authors declare that there are no conflicts of interest related to this article.
FinancingThere were no public or private funding sources for carrying out this study.