I work in a large quaternary academic ICU (64 beds) in the United States, with several teams caring for complex patients (around 5000 patient admissions a year). In a 24 h period close to 120 caregivers (physicians, trainees, nurses, respiratory therapists…) are involved in patient care. It is a highly complex and varied environment at risk for heterogeneity in practice. The key to our success is the use of protocols to ensure consistent and accountable care. Our ARDS patients all receive a protocolized lung-protective ventilation strategy which includes the application of PEEP (using one of the ARDSnet tables), measurement of the plateau pressure (Pplat), and limitation of the tidal volume (6–8 mL/kg IBW) as well as tidal pressure (aka, driving pressure). We personalize ventilator settings and, as needed, use advanced physiologic monitoring (e.g. esophageal pressure, volumetric capnography). These protocols continue to evolve according to available evidence. Although I could speak on each of the aspects of the protocol, the area where I will focus on in this article is our approach to mode selection and setting optimization. Here we present the framework of our protocol for goal-directed mode selection across the ARDS disease continuum.1
ARDS as a history, not a moment in timePatients with ARDS evolve through time. This evolution is related to the inciting disease and the evolution of lung injury. The risk for ventilator-induced lung injury, VILI, also is likely to change through the course of ARDS. (Fig. 1). In many protocols and reviews, the ventilator management of ARDS focuses on the initial or most acute phase.2 That is, the time when lung injury and risk of VILI are high and gas exchange abnormalities dominate. The main goal during the first stages of ARDS is safety and as such so are the modes and settings selected. However, this stage is a fraction of the time spent on MV and a small portion of the ARDS timeline. We now spend a fair amount of time waking patients up, mobilizing them, and allowing spontaneous breathing. It is illogical to think that one mode or setting (e.g. volume control (VC-CMVs)3 with VT of 6 mL/kg/PBW) would be appropriate throughout the ARDS timeline. Although it is possible to use one simple mode exclusively, doing so is difficult to implement and may expose the patient to other interventions (e.g. sedation) or risks (e.g. dyssynchrony). There is minimal guidance on how to ventilate patients after the most acute phase. While there are more than 500 names of ventilation modes to choose from in the United States alone,4 only three basic 3 modes are commonly used worldwide.5 There is no doubt these 3 modes work and that you can use them to ventilate anyone if you have enough skill. However, I argue that this is missing the point. Similar to cars, we can still use a 1940 car to get from A to Z, yet modern vehicles add features that improve safety, comfort, and efficiency. Available technology can make the ride better for the user, in a car as well as on a ventilator. The technology we have available makes some ventilator modes serve specific goals better than others, and as such, it may allow us to optimize care. But how do we know which of the many modes does what, and when do we apply them during the ARDS timeline?
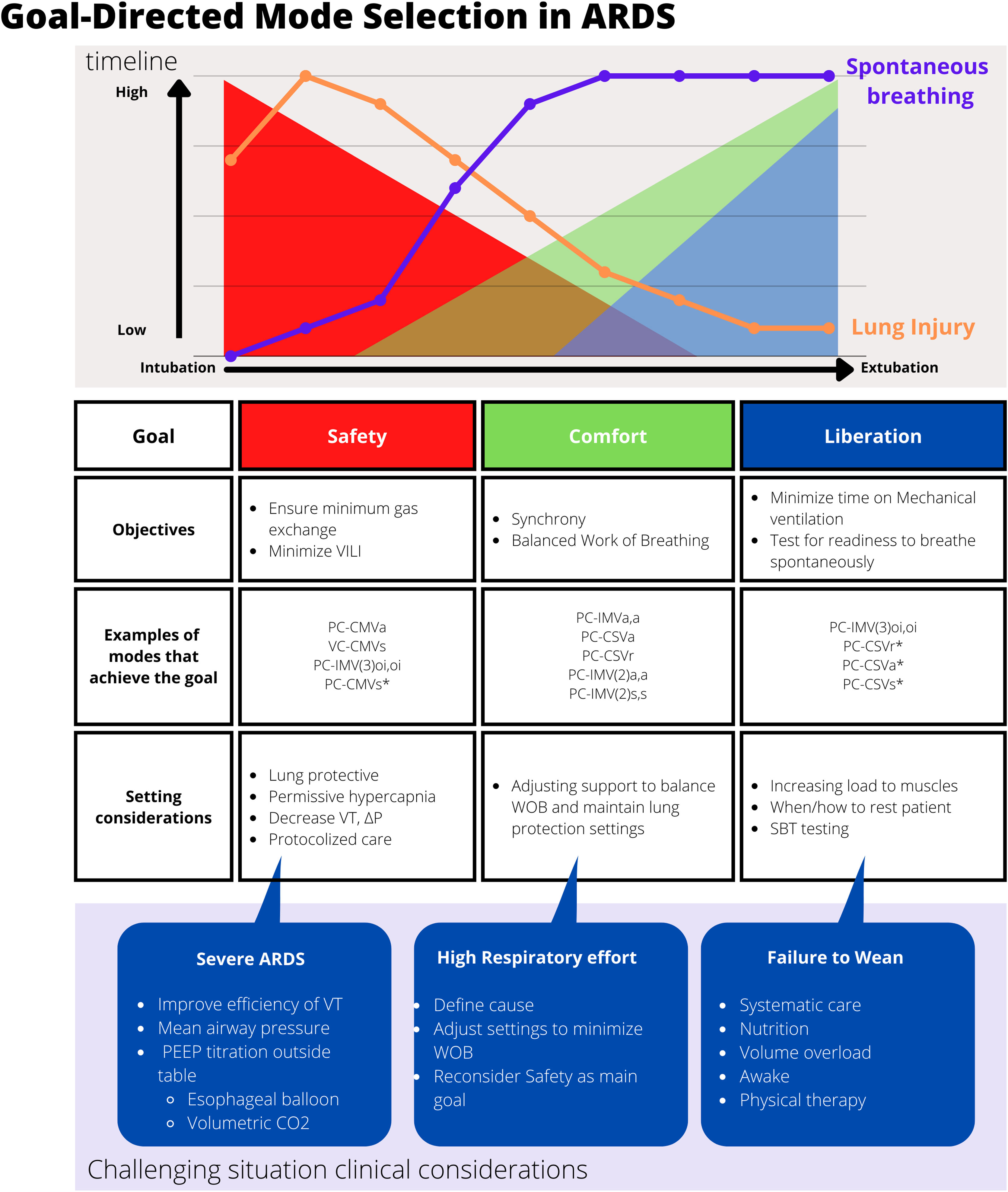
Goal-directed mode selection in ARDS.
The figure depicts 3 sections. The top panel highlights the timeline of ARDS from intubation and extubation in the X axis. The Y axis depicts intensity or importance. The orange line depicts a theorical amount or intensity of lung injury. The purple line depicts the presence of spontaneous breathing. The shaded areas are the goals of mechanical ventilation: Safety (red), Comfort (green) and Liberation (blue). The mid panel has the goals and objectives and an example of modes that serve these goals. The lower panel has considerations for settings in challenging situations. VILI, Ventilator-Induced Lung Injury; PC, Pressure Control; VC, Volume control; CMV, continuous mandatory ventilation; CSV, continuous spontaneous ventilation; IMV, Intermitent Mandatory ventilation; a, adaptive; s, set-point; o, optimal; i, intelligent; r, servo; *depending on settings and protocol used; VT, tidal volume; WOB, work of breathing; ΔP, driving pressure; SBT, spontaneous breathing trial; CO2, carbon dioxide.
Goal-directed ventilator mode selection aims at helping to select the mode and settings of ventilation according to the primary clinical goal at any point on the timeline. This applies to any disease or patient receiving mechanical ventilation, but we will focus on ARDS. We have defined 3 clinical goals of mechanical ventilation (safety, comfort, and liberation) and each goal has clinical objectives (Figure 1 and 2).1 These clinical goals highlight specific aspects of mechanical ventilation that we want to achieve with the ventilator. The goals change as the patient condition evolves. If the goal is safety, which encompasses ensuring a minimum level of gas exchange and preventing VILI, the mode we select should have technical features that will maximize the safety objectives (eg, ensures minimum minute ventilation, or limits tidal volume). This is also aligned with other interventions where patients may be kept more sedated during the initial phases of ARDS to minimize potential self-induced lung injury. Without a doubt, safety is an important goal throughout the timeline a patient is on mechanical ventilation. However, as lung injury decreases or the patient awakens, there is a change toward fostering appropriate patient-ventilator interactions, minimizing sedation, and allowing spontaneous breathing. This is served by the clinical goal of comfort, where the objective is to enhance synchrony and balance the work of breathing performed by the ventilator and the patient. Safety is still important and certainly will affect what mode we chose, but modes that have features that support the goal of comfort are favored. As the patient continues to recover, liberation emerges as the most important goal. There are modes that have features that favor liberation. Again, this does not mean safety and comfort are not relevant, these are just not the primary aim. In most cases liberation of the ventilator occurs after implementing a spontaneous breathing trial (SBT) protocol. Because an SBT is a test rather than a mode of ventialtion per se, the specific mode features may not be relevant. However, with difficult or prolonged weaning, ventilator modes that have features supporting the goal of liberation would be favored (eg, automatic reduction of support to maintain an optimal breathing pattern). Fig. 1 illustrates the idea that at any given time, more than one goal may exist. However, for the sake of mode selection, we chose one goal as the main one. A secondary goal may be present, but the main goal is the driver of mode and settings selections. By choosing a goal first, it is then easier and more effective to choose the mode of ventilation and settings, the sedation strategy, and other interventions. This is putting the patient first in the most practical sense, rather than reflexively using modes that are most familiar.
The implication of this strategy is that we use modes to serve the goals, and some modes will facilitate the goals better than others. A classic example is VC-CMVs (aka, volume assist/control),3 which is a staple of ARDS protocols. This is a mode where we, the operators, regulate all parameters of the assisted breath (ie, tidal volume and inspiratory flow, along with trigger and cycle thresholds). This mode serves the goal of safety perfectly. However, from the comfort standpoint, the more we control in a breath, the higher the chance of mismatch with the inspiratory efforts of a spontaneously breathing patient. Of course, an experienced operator may be able to change the settings to improve the interactions, but this requires the operator to be at the bedside frequently, and even then, discordance may occur as we walk away. If we then think of goal-directed mode selection in a patient in the initial phase of ARDS, where safety is the primary clinical goal, then VC-CMVs may make sense. Especially when sedation/paralysis may be used and patient-ventilatory synchrony is not an issue. However, if the patient will be less sedated, or in later phases, as ARDS improves, then VC-CMVs may predispose to dangerous patient-ventilator discordance (e.g. work shifting or breath stacking). Under these circumstances, a goal-directed approach would suggest a mode serving the primary goal of comfort, and safety as the secondary goal. We need a mode that favors synchrony (eg, by allowing and assisting spontaneous breaths) and balanced work of breathing but delivers a safe tidal volume dosage and targets a minimum minute ventilation. For example, PC-CMVa ( AKA as PRVC, VC+, APV). Some modes may allow transitions to serve different goals as the patient evolves. The most technically advanced modes that do this are those such as IntelliVent and Adaptive Support Ventilation (Hamilton ventilators), Adaptive Mode Ventilation (Vyaire bellavista ventilator) and AutoMode (Getinge ventilators). Indeed, these modes have a degree of automation to allow the clinical goals to be met (including liberation) without having to manually change modes during the ventilation timeline as the goals change (assuming the goal change is even identified in a timely fashion). The message is that there are available modes that will serve our clinical goals better. Moreover, there is enough technology now that may improve patient-ventilator interactions, improve safety measures and reduce the need for clinician interventions.
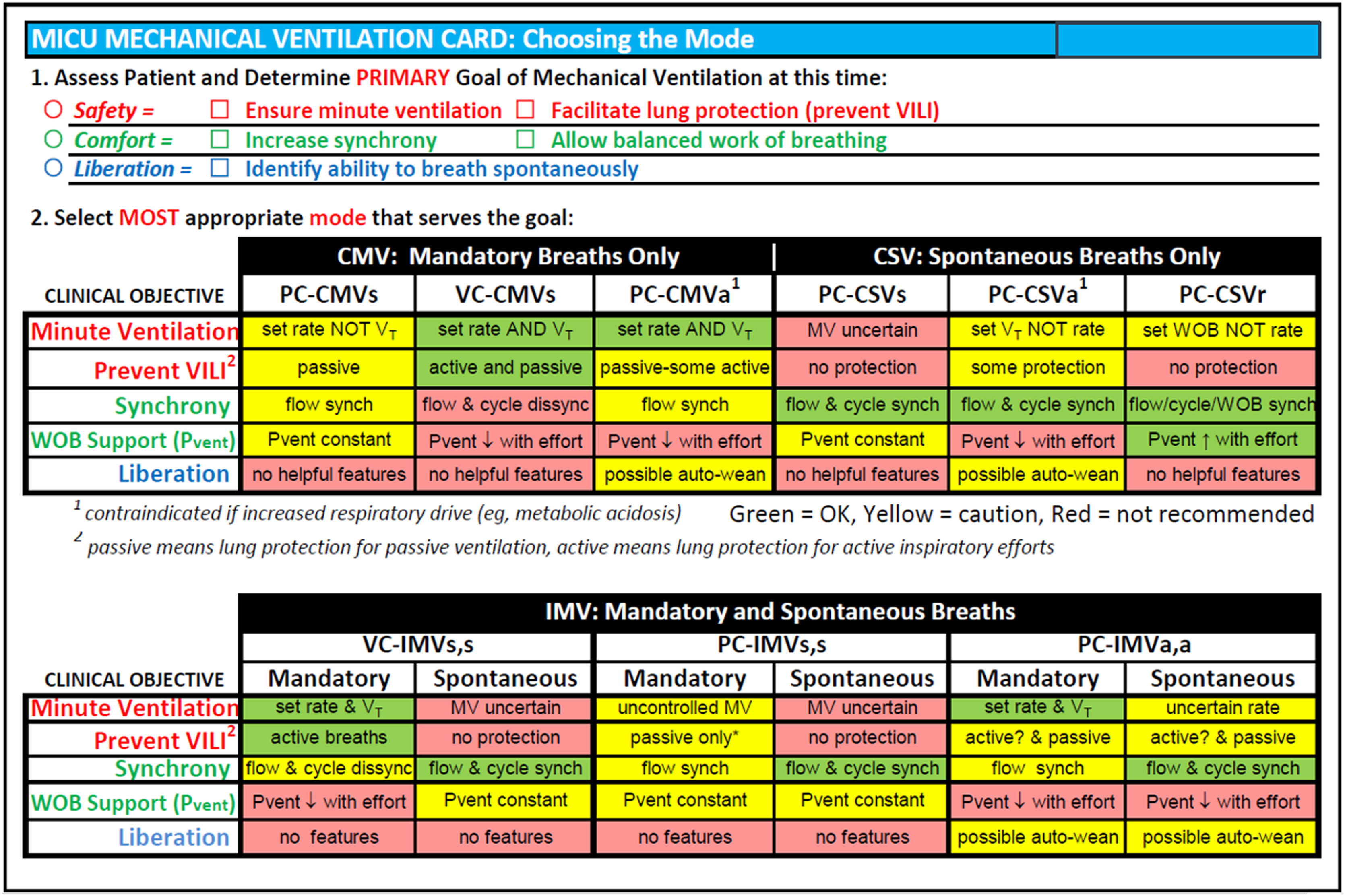
The challenge for our clinicians is to know what each mode does, how it serves the goals, and how to adjust settings to optimize the mode. We have written extensively about this topic.1,3,6,7 By using the mode taxonomy to classify all modes, we then know what each ventilator has available and how it serves the goals. Fig. 2 presents a fragment of a table we use to help our clinicians choose modes according to how they serve the goal. From my practice standpoint, I always start by asking what is my primary goal for the patient. This helps drive the ventilator strategy (mode and settings) and the related interventions (sedation goals, mobility). This is shared with the team, so they have clarity on how to adjust and modify settings through the patient care continuum. By using the patient-ventilator interaction taxonomy,7 we can monitor the change in clinical goals and how well the selected modes and settings serve the goals.
Modes and how they serve the goal.
Handout that highlights the method to use the Goal-directed mode selection. The clinician first choses the primary goal of ventilation, and secondary if relevant. The second step is to choose out of the grid the mode that better serves the primary goal. The grid is color coded. Green: the mode technical features serve the goal. Yellow: Caution, the mode technical feautures may serve the goal partially or it may not serve them under specific cirumstances (e.g. high respiratory effort). Red: Does not serve the goal and thus is not recommended. The second panel has IMV (intermittent mandatory ventilation) modes, where spontaneous and mandatory breaths coexist.
In summary, I follow a protocol that is guided by lung-protective strategy principles. During the ARDS timeline, I use goal-directed mode selection to guide patient and ventilator care to better use available technology to achieve the clinical goals.
ContributionsEduardo Mireles-Cabodevila, MD did Literature search, manuscript preparation, and review of manuscript.
Financial supportNone.
Conflict of interestDr. Mireles-Cabodevila is a co-owner of a patent for Mid–Frequency Ventilation. He receives royalties from the American College of Physicians, Elsevier, and Jones & Bartlett publishers. Consultant IngMar Medical.