Evidence only proves low surpasses high tidal volume (VT) for acute respiratory distress syndrome (ARDS). Intermediate VT is a common setting for ARDS patients and has been demonstrated as effective as low VT in non-ARDS patients. The effectiveness of intermediate VT in ARDS has not been studied and is the objective of this study.
DesignA retrospective cohort study.
SettingFive ICUs with their totally 130 beds in Taiwan.
Patients or participantsARDS patients under invasive ventilation.
InterventionsNo.
Main variables of interest28-D mortality.
ResultTotally 382 patients, with 6958 ventilator settings eligible for lung protection, were classified into low (mean VT=6.7ml/kg), intermediate (mean VT=8.9ml/kg) and high (mean VT=11.2ml/kg) VT groups. With similar baseline ARDS and ICU severities, intermediate and low VT groups did not differ in 28-D mortality (47% vs. 63%, P=0.06) or other outcomes such as 90-D mortality, ventilator-free days, ventilator-dependence rate. Multivariate analysis revealed high VT was independently associated with 28-D and 90-D mortality, but intermediate VT was not significantly associated with 28-D mortality (HR 1.34, CI 0.92–1.97, P=0.13) or 90-D mortality. When the intermediate and low VT groups were matched in propensity scores (n=66 for each group), their outcomes were also not significantly different.
ConclusionIntermediate VT, with its outcomes similar to small VT, is an acceptable option for ventilated ARDS patients. This conclusion needs verification through clinical trials.
La evidencia solo demuestra que el volumen tidal (VT) bajo supera al alto para el síndrome de dificultad respiratoria aguda (ARDS). La VT intermedia es un escenario común para los pacientes con ARDS y se ha demostrado que es tan eficaz como la VT baja en pacientes sin ARDS. No se ha estudiado la eficacia de la VT intermedia en el ARDS y es el objetivo de este estudio.
DiseñoUn estudio de cohorte retrospectivo.
ÁmbitoCinco UCI con un total de 130 camas en Taiwán.
Pacientes o participantesPacientes con ARDS bajo ventilación invasiva.
IntervencionesNo.
Variables de interés principalesMortalidad 28-D.
ResultadoUn total de 382 pacientes, con 6958 configuraciones de ventilador elegibles para protección pulmonar, se clasificaron en bajo (VT medio=6,7ml/kg), intermedio (VT medio=8,9ml/kg) y alto (VT medio=11,2ml/kg). Grupos de VT. Con un ARDS inicial similar y una gravedad en la UCI, los grupos de VT intermedia y baja no difirieron en la mortalidad 28-D (47% vs. 63%, p=0,06) u otros resultados como mortalidad 90-D, días sin ventilador, dependencia del ventilador índice. El análisis multivariado reveló que la VT alta se asoció de forma independiente con la mortalidad 28-D y 90-D, pero la VT intermedia no se asoció significativamente con la mortalidad 28-D (HR 1,34, IC 0,92-1,97, p=0,13) o la mortalidad 90-D. Cuando los grupos de VT intermedia y baja se emparejaron en puntajes de propensión (n=66 para cada grupo), sus resultados tampoco fueron significativamente diferentes.
ConclusiónLa VT intermedia, con resultados similares a la VT pequeña, es una opción aceptable para pacientes con ARDS ventilados. Esta conclusión necesita verificación a través de ensayos clínicos.
Mechanical ventilator support remains the cornerstone of acute respiratory distress syndrome (ARDS) management. Many harmful effects of mechanical ventilation, such as ventilator-induced lung injury (VILI), have been recognized and led to the development of a lung-protective ventilatory strategy, mainly by keeping tidal volume (VT) low. A well-known study by the ARDS Network in 2000 demonstrated that low VT (6ml/kg predicted body weight, PBW) is better than high VT (12ml/kg PBW) in terms of mortality and ventilator-free days.1 The superiority of low VT in this study may stem more from avoiding the harmful effects of high VT (12ml/kg PBW) and plateau pressure (up to 50cmH2O) than strict adherence to low VT per se. This speculation was supported by 3 futile clinical trials in low VT before the year 2000.2–4 With VT around 10ml/kg PBW and plateau pressure less than 31cmH2O in the control groups, the beneficial effects of low VT were completely abolished in these 3 studies.5 Therefore, we hypothesize that intermediate VT (7.5–10ml/kg PBW), by shunning the deleterious effects of high VT, could also be lung-protective as low VT.
Two decades after the publication of the landmark study,1 low VT adherence remains poor throughout the world.6,7 A survey of Chicago physicians found that more than 92% knew that patients with ARDS warranted low VT ventilation, but they ordered low VT in only 7% (0–14%) of their eligible patients.8 The reasons for nonadherence to low VT ventilation are complex. Some physicians are skeptical about applying evidence derived from randomized control trials to critical care practice,9,10 some may concern complications of low VT such as hypercapnia,11 air hunger sensation12 and possible self-inflicted lung injury if there is no adequate sedation or paralysis.13 Therefore, many physicians adopt a less strict version of lung protection ventilation. Intermediate VT was found in some studies to be the most commonly applied ventilator setting for patients with ARDS.14,15
Intermediate VT has been shown to be as effective as low VT for ventilated patients without ARDS in terms of mortality and other clinical outcomes.16–18 However, the role of intermediate VT in patients with ARDS has not been carefully studied. Data inferred from a study of 111 real-world patients with ARDS suggest that the mean VT of 9.5ml/kg PBW is not inferior to 6.1ml/kg PBW in terms of 28-day or 1-year mortality rate.19 In this study, we retrospectively compared the clinical outcomes of patients with ARDS who received intermediate and low VT.
MethodPatient enrollmentWe retrospectively collected invasively ventilated patients with ARDS admitted to Changhua Christian Hospital, a medical center with a total of 130 ICU beds in 5 separate wards, between January 2012 and November 2018. These patients were identified by their discharge diagnoses of ARDS and acute respiratory failure in electronic archives. Each diagnosis of ARDS was defined by the Berlin definition20 and was reconfirmed by one of our pulmonologists (SHW or YCH). Exclusion criteria include age less than 20 or over 90 years, actual body weight less than 40 or over 100kg, been transferred to other hospital or discharged against medical advice without traceable clinical outcome, a total duration of invasive ventilation less than 48h, using airway pressure release ventilation or high-frequency oscillation ventilation or extracorporeal membrane oxygenation during the ARDS period, been withdrawn from the ventilator due to hospice, co-morbidities of metastatic malignancy, end-stage heart failure (left ventricular ejection fraction less than 35%) or ventilator-dependence (invasive ventilation lasting over 21 days before the onset of ARDS), been enrolled in other ARDS-related clinical trials. The patients were followed until death or the 90th day after ARDS was diagnosed. The study was approved by the institutional review board of Changhua Christian Hospital (Approval No. 181214). The Board has waived the requirement for informed consent from participants.
Characteristics of the patients and treatment variablesBaseline variables when ARDS was diagnosed for the first time were collected. They include age, sex, body mass index, acute physiology and chronic health evaluation II (APACHE II) score,21 sequential organ failure assessment (SOFA) score,22 co-morbidity, predisposing factors for ARDS and type of ICU admitted. Whether patients received sedation, muscle relaxant, systemic steroid, vasopressor, hemodialysis, continuous hemofiltration, prone position, or total parenteral nutrition during the ARDS period were recorded.
Ventilator setting and monitoring parameters when eligible for lung protectionVentilator settings were recorded every 8h until ventilator discontinuation or the 28th day after diagnosing ARDS. If a fraction of inspired oxygen (FIO2)≥50% and positive end-expiratory pressure (PEEP) was greater than 5cmH2O, it was considered eligible for lung protection. This definition of eligibility was made because it approximated the threshold for a trial of spontaneous breathing without further restriction in VT or plateau pressure in the ARDS Network ventilation protocol.23VT and other ventilator parameters were counted and analyzed only when the occasions were eligible for lung protection. The mean VT was categorized based on each patient's predicted body weight1 into low (<7.5ml/kg PBW),19,24,25 intermediate (7.5–10ml/kg PBW)18 and high (>10ml/kg PBW).16 Other parameters collected include airway pressure (peak, mean, plateau, driving), PEEP, respiratory system compliance (CRS), and arterial oxygenation (PaO2, SpO2, PaO2/FIO2 ratio). When patients were under pressure-targeted ventilation and their plateau pressures were not measured directly, we used the peak airway pressure or the sum of PEEP and set increment of inspiratory pressure to represent plateau pressure.23
Outcome assessmentThe primary outcome was mortality rate of 28 days. Secondary outcome included a 90-day mortality rate, ventilator-free days during the initial 28 days, and ventilator-dependence rate on day 28 (excluding the patient who died within 28 days).
Statistical analysisData were expressed as a number (percent), mean±standard deviation or median, interquartile range (IQR). Each variable was tested for normal distribution using the Kolmogorov–Smirnov test. For the comparison of three groups of continuous variables, we used the analysis of variance or the Kruskal–Wallis analysis of variance test. Regarding categorical variables, the Chi-square or Fisher's exact test was used when appropriate. The Bonferroni-adjusted post hoc significance test was used to compare low and intermediate VT. Uni- and multi-variate Cox proportional hazards regression with backward selection procedure were used to assess hazard ratios (HR) and 95% confidence interval (CI) of mortality. VT category was retained in the models as a priori basis. Variables with a P-value of less than 0.10 in the crude model entered the multivariate model during backward selection. The propensity score was calculated by non-parsimonious multivariable logistic regression. All variables, except respiratory parameters, were considered. Propensity score matching was performed to balance the distributions of measured covariates in the low- and intermediate-VT groups. We matched each patient in the low VT group with one of the intermediate VT group based on propensity scores with a caliper of 0.1 standard deviation unit. All respiratory parameters were tested for collinearities using the variance inflation factor (VIF). A VIF over 2 indicates the presence of collinearity and it was excluded from the model. A P-value of less than 0.05 was considered significant. All statistical analyses were performed using the SPSS statistical package (IBM SPSS Statistics, version 20, IBM Corporation, Chicago, IL, USA).
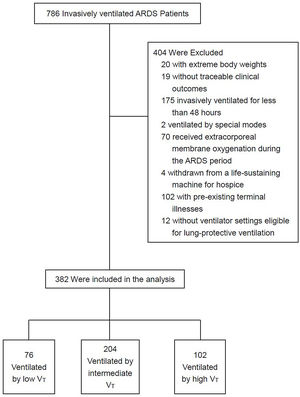
ResultTotally 786 patients were invasively ventilated for their ARDS and acute respiratory failure. Four hundred and four patients were excluded because of 20 with extreme body weights, 19 without traceable clinical outcomes, 175 invasively ventilated for less than 48h, 2 ventilated by special modes, 70 received extracorporeal membrane oxygenation during the ARDS period, 4 withdrawn from a life-sustaining machine for hospice, 102 with pre-existing terminal illnesses and 12 without ventilator settings eligible for lung-protective ventilation. Therefore, 382 patients, with a total of 6958 ventilator settings eligible for lung-protective ventilation, were analyzed. A flowchart of patients included in the final analysis was presented in Fig. 1.
The patients were classified into low (mean VT=6.7ml/kg PBW, n=76, 19.9%), intermediate (mean VT=8.9ml/kg PBW, n=204, 53.4%) and high (mean VT=11.2ml/kg PBW, n=102, 26.7%) VT groups according to their mean VT while eligible for lung protection. Their baseline characteristics, treatment, and ventilator setting variables are summarized in Table 1. Intermediate and low VT groups did not differ in their baseline APACHE II or SOFA scores. Both groups also have a comparable baseline ARDS severity distribution. The driving pressures the patients received were not significantly different.
Baseline characteristics and treatment variables.
| Low VT(n=76) | Intermediate VT(n=204) | High VT(n=102) | P-value | Adjusted P-valuec of intermediate vs. low VT | |
|---|---|---|---|---|---|
| Age (year), mean±SD | 61±17 | 64±16 | 66±15 | 0.17 | 0.70 |
| Male, No. (%) | 61 (80) | 145 (71) | 58 (57) | <0.01 | 0.36 |
| Body mass index, median (IQR), (kg/m2) | 22 (19–24) | 23 (20–26) | 23 (21–26) | 0.01 | 0.01 |
| APACHE II Score, median (IQR) | 25 (21–30) | 25 (19–29) | 21 (17–30) | 0.21 | 1.00 |
| SOFA score, median (IQR) | 7 (5–10) | 8 (5–10) | 7 (5–9) | 0.65 | 1.00 |
| Severity of ARDS at diagnosis | |||||
| mild, No. (%) | 16 (21) | 41 (21) | 26 (28) | 0.55 | 0.99 |
| moderate, No. (%) | 30 (40) | 92 (48) | 48 (51) | 0.58 | 0.48 |
| severe, No. (%) | 29 (39) | 60 (31) | 20 (21) | 0.02 | 0.21 |
| PaO2/FIO2 at diagnosis | 119 (90–176) | 126 (95–180) | 154 (109–208) | 0.03 | 0.98 |
| Etiology | |||||
| Sepsis, No. (%) | 32 (42) | 80 (39) | 42 (41) | 0.91 | 1.00 |
| Pneumonia, No. (%) | 62 (82) | 149 (73) | 60 (59) | <0.01 | 0.47 |
| Pancreatitis, No. (%) | 1 (1) | 9 (4) | 3 (3) | 0.42 | 0.64 |
| Aspiration, No. (%) | 4 (5) | 14 (7) | 8 (8) | 0.80 | 1.00 |
| Blood transfusion, No. (%) | 7 (9) | 25 (12) | 15 (15) | 0.54 | 1.00 |
| Others or Unknown, No. (%) | 9 (12) | 27 (13) | 26 (26) | 0.04 | 1.00 |
| Comorbidity | |||||
| Chronic obstructive pulmonary disease, No. (%) | 27 (36) | 71 (35) | 29 (28) | 0.48 | 1.00 |
| Diabetes mellitus, No. (%) | 35 (46) | 73 (36) | 32 (31) | 0.12 | 0.35 |
| Hypertension, No. (%) | 28 (37) | 98 (48) | 55 (54) | 0.08 | 0.28 |
| Chronic kidney disease, No. (%) | 11 (14) | 27 (13) | 13 (13) | 0.94 | 1.00 |
| Heart failure, No. (%) | 20 (26) | 66 (32) | 33 (32) | 0.60 | 0.99 |
| Cerebral vascular accident, No. (%) | 13 (17) | 56 (27) | 22 (22) | 0.16 | 0.22 |
| Liver cirrhosis, No. (%) | 8 (10) | 25 (12) | 11 (11) | 0.89 | 1.00 |
| Malignancy, No. (%) | 23 (30) | 44 (22) | 22 (22) | 0.28 | 0.39 |
| Immunosuppressed, No. (%) | 15 (20) | 30 (15) | 26 (25) | 0.07 | 0.92 |
| Surgical ICU admission, No. (%) | 5 (7) | 22 (11) | 30 (29) | <0.01 | 0.87 |
| Cumulative fluid balance in the 1st week, median (IQR), (L) | 5 (2–9) | 4 (1–8) | 4 (0–7) | 0.55 | 1.00 |
| Treatment received during ARDS | |||||
| Sedation, No. (%) | 73 (96) | 187 (92) | 93 (91) | 0.40 | 0.62 |
| Muscle relaxant, No. (%) | 75 (99) | 189 (93) | 80 (78) | <0.01 | 0.08 |
| Single shot facilitating intubation | 1 (1) | 6 (3) | 7 (9) | 0.13 | 0.10 |
| Continuous infusion facilitating synchrony | 65 (87) | 150 (79) | 63 (79) | ||
| For both intubation and synchrony | 9 (12) | 33 (17) | 10 (12) | ||
| Vasopressor, No. (%) | 62 (82) | 160 (78) | 74 (73) | 0.32 | 1.00 |
| Total parenteral nutrition, No. (%) | 13 (17) | 36 (18) | 26 (25) | 0.22 | 1.00 |
| Systemic steroid, No. (%) | 69 (91) | 172 (84) | 81(79) | 0.12 | 0.49 |
| Prone position, No. (%) | 15 (20) | 25 (12) | 2 (2) | <0.01 | 0.34 |
| Hemodialysis, No. (%) | 13 (17) | 27 (13) | 10 (10) | 0.36 | 1.00 |
| Continuous hemofiltration, No. (%) | 35 (46) | 72 (35) | 20 (20) | <0.01 | 0.30 |
| Respiratory parameters when eligible for lung protection, median (IQR) | |||||
| VT/PBW (ml/Kg) | 6.7 (6.2–7.1) | 8.9 (8.3–9.4) | 11.2 (10.6–12.0) | <0.01 | <0.01 |
| CRSa (ml/cmH2O) | 21 (18–26) | 27 (23–31) | 29 (24–34) | <0.01 | <0.01 |
| Plateau pressureb (cmH2O) | 33 (31–35) | 32 (30–34) | 32 (29–34) | 0.02 | 0.04 |
| PEEP (cmH2O) | 12 (10–14) | 11 (10–12) | 10 (9–10) | <0.01 | <0.01 |
| Driving pressureb (cmH2O) | 21 (18–24) | 21 (18–23) | 22 (20–25) | 0.04 | 1.00 |
The outcomes of the three groups are shown in Table 2. Intermediate VT has similar 28-day mortality with the low VT group (47.1% vs. 63.2%, P=0.06). Intermediate and low VT groups did not differ significantly in other outcomes, such as 90-day mortality, ventilator-free days, ventilator-dependence rate, or barotrauma rate. By Cox regression model analysis, high VT (HR 1.78, 95% CI 1.08–2.94, P=0.03), male, low CRS, liver cirrhosis, and high PEEP were independently associated with mortality at 28 days (Table 3). Intermediate VT was not independently associated with 28-day mortality (HR 1.34, 95% CI 0.92–1.97, P=0.13). Factors independently associated with 90-day mortality include high VT (HR 1.62, 95% CI 1.06–2.49, P=0.03), age, male, hypertension, liver cirrhosis, malignancy, low CRS, high FIO2 and low PaO2 (Table s1). Again, intermediate VT was not independently associated with mortality at 90 days. The collinearities of FIO2, PaO2, and CRS were excluded due to their lower than 2 VIF values (Table s2).
Outcomes of ARDS patients receiving various VT.
| Low VT(n=76) | Intermediate VT(n=204) | High VT(n=102) | P-value | Adjusted P-value for intermediate vs. low VTb | |
|---|---|---|---|---|---|
| Mortality at day 28 (%) | 48 (63) | 96 (47) | 43 (42) | 0.02* | 0.06 |
| Mortality at day 90 (%) | 52 (68) | 125 (61) | 58 (57) | 0.29 | 0.81 |
| Ventilator-free days, day 1–28a, median (IQR) | 12 (2–18) | 13 (0–18) | 10 (0–19) | 0.84 | 1.00 |
| Ventilator dependence by day 28a(%) | 8 (29) | 40 (37) | 23 (39) | 0.62 | 1.00 |
| Evolution of ARDS severity in the 1st week | 0.16 | 0.93 | |||
| Improved, No (%) | 23 (30) | 74 (36) | 44 (43) | ||
| Worsened, No (%) | 21 (28) | 64 (38) | 33 (32) | ||
| Stationary, No (%) | 32 (42) | 66 (32) | 25 (24) | ||
| Length of stay in ICU, median (IQR), day | 11 (6–19) | 13 (7–19) | 13 (7–21) | 0.70 | 1.00 |
| Length of stay in hospital, median (IQR), day | 14 (6–23) | 16 (8–30) | 18 (9–37) | 0.06 | 0.40 |
| Pneumothorax (%) | 3 (4) | 8 (4) | 10 (10) | 0.08 | 1.00 |
| Subcutaneous emphysema (%) | 6 (8) | 9 (4) | 6 (6) | 0.51 | 0.75 |
Factors associated with 28-day mortality.
| Univariate analysis | Multivariate analysis | |||||
|---|---|---|---|---|---|---|
| Crude HR (95% CI) | P-value | Adjusted HR (95% CI) | P-value | Adjusted HRa (95% CI) | P-value | |
| Low VT | 1 | |||||
| Intermediate VT | 0.70 (0.50, 0.99) | 0.04 | 1.44 (0.98, 2.14) | 0.07 | 1.34 (0.92, 1.97) | 0.13 |
| High VT | 0.57 (0.38, 0.86) | 0.01 | 1.86 (1.12, 3.10) | 0.02 | 1.78 (1.08, 2.94) | 0.03 |
| Age, per year | 1.00 (0.99, 1.01) | 0.37 | ||||
| Male | 1.36 (0.99, 1.88) | 0.06 | 2.01 (1.41, 2.86) | <0.01 | 2.09 (1.47, 2.98) | <0.01 |
| Body mass index, per kg/m2 | 0.97 (0.94, 1.00) | 0.06 | 0.99 (0.95, 1.02) | 0.42 | ||
| APACHE II score, per point | 1.01 (0.99, 1.02) | 0.53 | ||||
| SOFA score, per point | 1.02 (0.98, 1.06) | 0.30 | ||||
| PaO2/FIO2 at diagnosis | 1.00 (0.99, 1.00) | 0.35 | ||||
| Chronic obstructive pulmonary disease | 1.15 (0.86, 1.54) | 0.36 | ||||
| Diabetes mellitus | 0.91 (0.68, 1.23) | 0.53 | ||||
| Hypertension | 0.74 (0.55, 0.99) | 0.04 | 0.84 (0.62, 1.13) | 0.24 | ||
| Chronic renal failure | 0.88 (0.59, 1.33) | 0.55 | ||||
| Heart failure | 0.92 (0.68, 1.26) | 0.61 | ||||
| Liver cirrhosis | 1.61 (1.08, 2.39) | 0.02 | 1.61 (1.07, 2.41) | 0.02 | 1.72 (1.15, 2.56) | 0.01 |
| Malignancy | 1.57 (1.15, 2.14) | 0.01 | 1.27 (0.92, 1.76) | 0.15 | ||
| Continuous hemofiltration | 2.01 (1.51, 2.68) | <0.01 | ||||
| CRSb, per ml/cmH2O | 0.94 (0.92, 0.96) | <0.01 | 0.92 (0.89, 0.94) | <0.01 | 0.91 (0.89, 0.94) | <0.01 |
| Plateau Pressure, per cmH2O | 1.00 (1.00, 1.01) | 0.42 | ||||
| PEEP, per cmH2O | 1.13 (1.06, 1.22) | <0.01 | 1.24 (1.15, 1.34) | <0.01 | 1.23 (1.14, 1.33) | <0.01 |
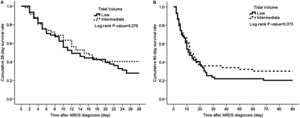
Intermediate and low VT cohorts matched with the propensity score were developed. Their characteristics and outcomes are presented in Table 4. Both groups did not differ in mortality (Fig. 2) and all other clinical outcomes. Multivariate analysis revealed that low CRS and high FIO2 were independently associated with mortality rate of 28- or 90-days, while intermediate VT was not (Table s3).
Characteristics and outcomes of propensity score-matched cohorts.
| Low VT(n=66) | Intermediate VT(n=66) | P-value | |
|---|---|---|---|
| Age (year) | 62±17 | 60±16 | 0.53 |
| Male (%) | 52 (79) | 57 (86) | 0.25 |
| Body mass index (kg/m2) | 22 (19–24) | 24 (22–26) | 0.00 |
| APACHE II score | 25 (20–30) | 25 (18–28) | 0.47 |
| SOFA score | 7 (5–9) | 8 (6–11) | 0.21 |
| Lung injury score | 12 (11–13) | 11 (10–13) | 0.54 |
| Comorbidity | |||
| Chronic obstructive pulmonary disease (%) | 22 (33) | 20 (30) | 0.71 |
| Diabetes mellitus (%) | 28 (42) | 25 (38) | 0.59 |
| Hypertension (%) | 26 (39) | 22 (33) | 0.47 |
| Chronic renal failure (%) | 9 (14) | 7 (11) | 0.59 |
| Heart failure (%) | 18 (27) | 20 (30) | 0.70 |
| Cerebral vascular accident (%) | 11 (17) | 11(17) | 1.00 |
| Liver cirrhosis (%) | 8 (12) | 10 (15) | 0.61 |
| Malignancy (%) | 20 (30) | 22 (33) | 0.71 |
| Admission for surgical conditions (%) | 5 (8) | 11 (17) | 0.11 |
| VT/predicted body weight (ml/kg) | 6.7 (6.1–7.2) | 9.0 (8.3–9.4) | 0.00 |
| CRSb (ml/H2O) | 21 (17–25) | 29 (25–33) | 0.00 |
| Driving pressure (cmH2O) | 21 (18–24) | 21 (18–23) | 0.20 |
| FIO2 (%) | 73 (64–89) | 66 (59–77) | 0.04 |
| PaO2/FIO2 ratio | 127 (94–183) | 127 (83–192) | 0.76 |
| Outcomes | |||
| Ventilator-free days, day 1–28a, median (IQR) | 12 (2–18) | 15 (3–19) | 0.51 |
| Ventilator dependence by day 28a (%) | 7 (32) | 8 (25) | 0.58 |
| 28-Day mortality (%) | 44 (67) | 34 (52) | 0.08 |
| 90-Day mortality (%) | 47 (71) | 37 (56) | 0.07 |
| Barotrauma (%) | 6 (9) | 5 (8) | 0.75 |
According to several surveys,14,17 intermediate VT was commonly used in patients with or without ARDS throughout the world. However, our study is the first report on the clinical outcomes of the use of intermediate VT in patients with ARDS.
Some animal studies have confirmed that high VT contributes to VILI.26,27 A recent study found that patients ventilated with VT of 12ml/kg PBW for as short as 4 days could induce lung inflammation.28 The well-known study by the ARDS Network showed that high VT has a worse outcome than low VT.1 Our results also confirm that high VT is independently associated with mortality at 28 and 90 days in patients with ARDS. However, strict adhesion to low VT may not be necessary. According to data from our study, intermediate VT, by shunning the deleterious effect of high VT, has comparable clinical outcomes with low VT.
Low VT is not by itself the only factor in preventing VILI. Amato et al. found that VT divided by CRS, or driving pressure, is most strongly associated with survival in ARDS.29 Gattinoni et al. coined the term ‘baby lung’ to describe a fraction of the lung parenchyma that maintains normal inflation in patients with ARDS. They argued that VT should be adjusted according to the size of the baby lung and the strain it received during mechanical inflation instead of ideal body weight.30 They incorporated VT and a bundle of respiratory parameters to measure the mechanical power lung received during ventilation,31 which is considered more accurate in predicting the likelihood of VILI.32 Since VT per se is not of utmost importance in preventing VILI, more strict control of VT (i.e., ultralow VT) failed to produce additional benefit as some researchers expected.33
Strictly low VT may not be necessary for all patients with ARDS. Several ARDS phenotypes have been identified. About 55% of patients who met the Berlin definition of ARDS do not have typical pathological diffuse alveolar damage. These patients tend to have milder symptoms and shorter clinical courses.34 About 10–17% of patients with ARDS were extubated or no longer met the criteria for ARDS in less than 24h.14,35 These subsets of ARDS with their distinct clinical course may warrant personalized treatment. A recently published French trial tested personalized treatment by giving patients with ARDS with focal involvement a VT of 8ml/kg PBW and those without focal involvement a VT of 6ml/kg PBW in addition to a bundle of other related ventilatory maneuvers. The per protocol analysis showed that patients in the personalized treatment group have a survival advantage over the control group, who universally received a VT of 6ml/kg PBW.36
To classify VT as low or not, some observational studies on ARDS only counted the VT patients received in the initial few days.6,19 However, this way of counting inappropriately neglected the influences of VT patients received in subsequent days. We adopted the method of Needham et al. by counting all VT patients received for up to 28 days if their ventilator settings were considered eligible for lung protection.23 We recorded VT three times per day, more frequently than Needham (twice per day). Based on the mean of all VT patients received throughout the whole ventilation courses, we believe our categorization of VT is more accurate than many previous observational studies on ARDS.
The VT received by our patients were not randomly assigned, but were given according to the in-charge doctors’ choice. We find those receiving low VT have lower CRS (Table 1), which made higher VT inappropriate because the limitation of plateau pressure could easily be exceeded. Whereas those with higher CRS were more likely to receive intermediate, rather than low VT. This practice was in line with the global tendency toward nonadherence to low VT6–8 as we have mentioned in our introduction.
Prone positioning has been proved effective for moderate to severe ARDS patients,37 but only 12% and 20% (from intermediate and low VT group respectively, both with a median of PaO2/FIO2<150mmHg) of our patients received this adjunctive therapy. This was just another example of discrepancy between clinical trial and clinical practice. This trend was also universal. The LUNG SAFE study, involving 50 countries around the world, found prone was used in only 6% and 16% of the moderate and severe ARDS patients respectively.14 A recent survey of moderate-to-severe ARDS patients in the US found only 6% of them received prone in their early management.38 Efforts are needed to find reasons behind the widespread nonadherence.
Liver cirrhosis was found to be an independent risk factor for 28- and 90-day mortality in our patients with ARDS. This finding was in accordance with previous studies.39,40 Increased pro-inflammatory interleukine-6 and interleukine-8 in patients with decompensated cirrhosis were thought to contribute to lung injury in those at risk.41
There are several limitations to this study. First, it was a retrospective observation. The classification of VT groups was not assigned randomly. Selection bias and unrecognized confounders are possible. Second, our data were all from one center. The generalizability of our conclusion can be limited. Third, for patients with pressure-targeted ventilation, plateau pressures were not measured directly. We used the peak airway pressure or the sum of PEEP and set increment of inspiratory pressure instead.23 The plateau pressure derived by this way is prone to over-estimation.42 Driving pressure and CRS calculated from this putative plateau pressure were all subject to imprecision.
In conclusion, we found that high VT is harmful to patients with ARDS. Intermediate and low VT and have similar clinical outcomes. Our results suggested that intermediate VT is an acceptable option for ventilated patients with ARDS. This conclusion needs to be verified by randomized control trials.
FundingThe study was supported by grant number 108-CCH-IRP-012 (Changhua Christian Hospital).
Authors’ contributionsSHW drafted the manuscript. CTK analyzed the data and performed statistical calculations. CYL collected clinical data from study patients. YCH gave final approval of the version to be published.
Conflict of interestNo conflict of interest to declare.
We thank Hui-Ching Chen, Kuan-I Lee and Wan-ping Wen for secretarial assistance.
We thank Dr. Lon-Yen Tsao for the critical review of our manuscript.