Arterial catheterization is a frequent proceeding in critically ill to obtain repetitively blood sampling and continuous monitoring of systemic arterial pressure arterial.1–3 The incidence of accidental catheter removal (ACR) in arterial catheters has been scarcely studied,4–8 and we did not find studies comparing the ACR incidence between femoral, cubital, dorsalis pedis and brachial arterial sites. The importance of ACR lies in that could cause severe complications, such as severe external haemorrhage and vascular damage, and some could be potentially life-threatening. Thus, due to the scarce published data and the possibility of severe complications in relation to ARC of arterial catheters we proposed this study. The objective of this study was to compare the incidence of ACR in femoral, cubital, dorsalis pedis and brachial arterial sites.
We performed a retrospective study over seven years of all patients who were undergoing to femoral, cubital, dorsalis pedis or brachial arterial catheterization during their stay in the polyvalent Intensive Care Unit of the Hospital Universitario de Canarias, Tenerife, Spain. The study was approved by the institutional review board.
The following data were collected: age, sex, diabetes mellitus, APACHE-II, diagnosis group, catheter access, catheter insertion and removal dates, and cause of catheter removal (planned or accidental).
We considered accidental catheter removal as the presence of an unplanned removal produced by the patient or the staff. The ACR can be performed by the patient, either by taking hold of it with their hands or by making voluntary movements that led directly the removal. The ACR can be performed by the staff as consequence of inadequate handling. The catheters removed due to obstruction of the catheter were not considered as ACR.
Statistical analyses were performed with SPSS 12.0.1 (SPSS Inc., Chicago, IL), LogXact 4.1 (Cytel Co., Cambridge, MA) and StatXact 5.0.3 (Cytel Co., Cambridge, MA). Continuous variables are reported as medians and percentiles 25th–75th, and were compared using Mann–Whitney test. Categorical variables are reported as frequencies and percentages, and were compared using Chi-square test. The incidence of ACR between groups was compared using Cox regression. The magnitude of the effects is expressed as Hazard Ratio (HR) and 95% confidence interval (CI). A p-value less than 0.05 was considered statistically significant.
Were included a total of 2199 arterial catheters and remain in situ during 13,237 days. We detected 116 ACR, thus the 5.3% arterial catheters were accidentally removed and we had 0.88 ACR per 100 days of arterial catheterization.
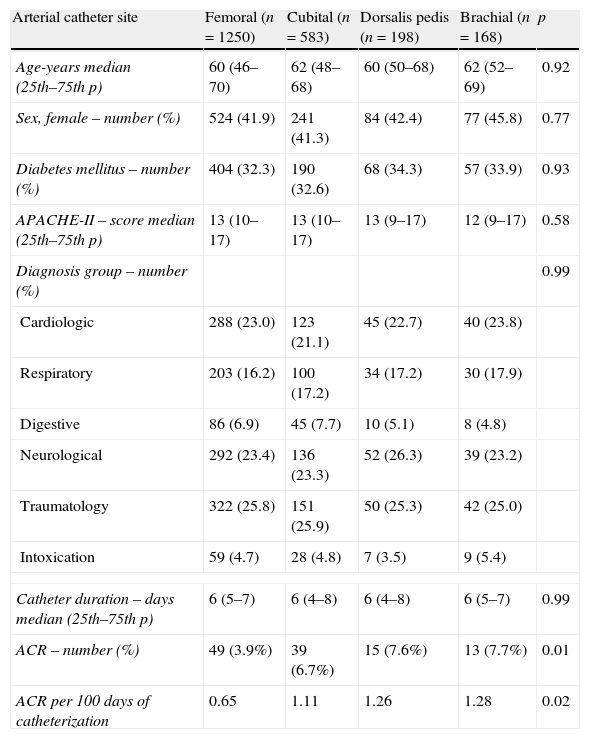
We found 49 events of ACR in 1250 (3.9%) arterial femoral catheters during 7524 days of catheterization (0.65 events of ACR per 100 days of catheterization), 39 events of ACR in 583 (6.7%) arterial cubital catheters during 3513 days of catheterization (1.11 events of ACR per 100 days of catheterization), 15 events of ACR in 198 (7.6%) arterial dorsalis pedis catheters during 1187 days of catheterization (1.26 events of ACR per 100 days of catheterization) and 13 events of ACR in 168 (7.7%) arterial brachial catheters during 1013 days of catheterization (1.28 events of ACR per 100 days of catheterization), As shown in Table 1, there were no significant differences between femoral, cubital, dorsalis pedis and brachial arterial catheters in age, sex, diabetes mellitus, APACHE-II, diagnosis group and duration of the catheter. However, there were found statistically significant differences in the percentage of catheters with ACR (p=0.01) and in the ACR incidence per 100 days of catheterization (p=0.02) between the different arterial sites.
Characteristics of different arterial catheters.
| Arterial catheter site | Femoral (n=1250) | Cubital (n=583) | Dorsalis pedis (n=198) | Brachial (n=168) | p |
| Age-years median (25th–75th p) | 60 (46–70) | 62 (48–68) | 60 (50–68) | 62 (52–69) | 0.92 |
| Sex, female – number (%) | 524 (41.9) | 241 (41.3) | 84 (42.4) | 77 (45.8) | 0.77 |
| Diabetes mellitus – number (%) | 404 (32.3) | 190 (32.6) | 68 (34.3) | 57 (33.9) | 0.93 |
| APACHE-II – score median (25th–75th p) | 13 (10–17) | 13 (10–17) | 13 (9–17) | 12 (9–17) | 0.58 |
| Diagnosis group – number (%) | 0.99 | ||||
| Cardiologic | 288 (23.0) | 123 (21.1) | 45 (22.7) | 40 (23.8) | |
| Respiratory | 203 (16.2) | 100 (17.2) | 34 (17.2) | 30 (17.9) | |
| Digestive | 86 (6.9) | 45 (7.7) | 10 (5.1) | 8 (4.8) | |
| Neurological | 292 (23.4) | 136 (23.3) | 52 (26.3) | 39 (23.2) | |
| Traumatology | 322 (25.8) | 151 (25.9) | 50 (25.3) | 42 (25.0) | |
| Intoxication | 59 (4.7) | 28 (4.8) | 7 (3.5) | 9 (5.4) | |
| Catheter duration – days median (25th–75th p) | 6 (5–7) | 6 (4–8) | 6 (4–8) | 6 (5–7) | 0.99 |
| ACR – number (%) | 49 (3.9%) | 39 (6.7%) | 15 (7.6%) | 13 (7.7%) | 0.01 |
| ACR per 100 days of catheterization | 0.65 | 1.11 | 1.26 | 1.28 | 0.02 |
ACR: accidental catheter removal; p: percentile.
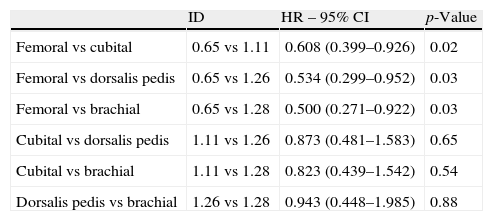
Cox regression analysis showed a lower ACR incidence in femoral than in cubital (Hazard Ratio=0.608; 95% CI=0.399–0.926; p=0.02), dorsalis pedis (Hazard Ratio=0.534; 95% CI=0.299–0.952; p=0.03) and brachial (Hazard Ratio=0.500; 95% CI=0.271–0.922; p=0.03) arterial catheters (Table 2).
Comparisons of ACR incidence between different arterial sites.
| ID | HR – 95% CI | p-Value | |
| Femoral vs cubital | 0.65 vs 1.11 | 0.608 (0.399–0.926) | 0.02 |
| Femoral vs dorsalis pedis | 0.65 vs 1.26 | 0.534 (0.299–0.952) | 0.03 |
| Femoral vs brachial | 0.65 vs 1.28 | 0.500 (0.271–0.922) | 0.03 |
| Cubital vs dorsalis pedis | 1.11 vs 1.26 | 0.873 (0.481–1.583) | 0.65 |
| Cubital vs brachial | 1.11 vs 1.28 | 0.823 (0.439–1.542) | 0.54 |
| Dorsalis pedis vs brachial | 1.26 vs 1.28 | 0.943 (0.448–1.985) | 0.88 |
ACR: accidental catheter removal; ID: incidence density (defined as number of ACR per 100 catheter-days); HR: hazard ratio; CI: confidence interval.
To our knowledge, this is the first study comparing ACR incidence between femoral, cubital, dorsalis pedis and brachial arterial sites. The most relevant finding of our study is that femoral arterial catheter showed a lower ACR incidence that cubital, dorsalis pedis and brachial arterial catheters.
In our study, we found that the 5.3% of arterial catheters were accidentally removed and an ACR rate of 0.88 events per 100 days of arterial catheterization. Our ACR rate is in the limit low according the previously reported rates, which is range between 3.8 and 18.4% catheters and of 1.17–1.8 events of ACR per 100 days of catheterization.4–8
In addition, we found for the first time that femoral arterial catheter showed a lower ACR incidence that cubital, dorsalis pedis and brachial arterial catheters. This is a novel aspect in relation to ACR of arterial catheters due to that previously was not reported a comparison of ACR between these arterial sites.
In a previous study of our team,9 we did not find significant differences in the ACR rate between 1057 radial, 125 femoral, 30 dorsalis pedis and 19 brachial arterial sites. Afterwards, increasing the sample size to 2419 radial and 1085 femoral arterial catheters was found a lower ACR in femoral than in radial arterial catheter.10 In the same way, the increase of sample size to 1250 femoral, 583 cubital, 198 dorsalis pedis and 168 brachial arterial sites could contributed in the appearance of significant differences in our current study.
Whereas the strength of our study was the relatively large sample size compared with previous studies,4–8 some limitations should be recognized. First, there was not a randomization in the different arterial catheter site and the site was chose by criteria physician. Second, cubital, dorsalis pedis and brachial arterial catheters were fixed by steri-strip, and femoral arterial catheters were fixed by silk suture. Despite these limitations, we think that the results of our study could contribute to know more about ACR in critically ill patient.
In conclusion, ACR is a frequent complication between the critically ill patients and is another important aspect of patient safety. In our study, the arterial femoral site showed a lower risk of ACR than cubital, dorsalis pedis and brachial arterial sites.
FundingsThis study was supported, in part, by a grant from Instituto de Salud Carlos III (I3SNS-INT-11-063 and I3SNS-INT-12-087) (Madrid, Spain).