Editado por: Alberto García-Salido - Cuidados Intensivos Pediátricos, Hospital Infantil Universitario Niño Jesús, Madrid
Última actualización: Mayo 2024
Más datosTo assess children's functional outcomes one year after critical illness and identify which factors influenced these functional outcomes.
DesignAmbispective cohort study.
SettingPediatric intensive care unit (PICU) in a tertiary academic center.
ParticipantsChildren (1 month–17-year-old) and their caregivers.
InterventionsNone.
Main variables of interestDemographic, clinical, and functional status.
ResultsOf 242 patients screened, 128 completed the year follow-up. These children had significant changes in functional status over time (p<0.001). The functional decline occurred in 62% of children at discharge and, after one year, was persistent in 33%. Age>12 months was a protective factor against poor functional outcomes in two regression models (p<0.05). A moderately abnormal functional status and a severely/very severely abnormal functional status at discharge increased the risks of poor functional outcomes by 4.14 (95% CI 1.02–16.72; p=0.04), and 4.76 (CI 95% 1.19–19.0; p=0.02). A functional decline at discharge increased by 6.86 (95%CI: 2.16-21.79; p=0.001) the risks of children's long-term poor functional outcomes, regardless of the FSS scores.
ConclusionThis is the first study evaluating long-term functional outcomes after pediatric critical illnesses in Latin America. Our findings show baseline data and raise relevant questions for future multicentre studies in this field in Latin America, contributing to a better understanding of the effects of critical illnesses on long-term functional outcomes in children.
Evaluar los resultados funcionales de los niños un año después de la enfermedad crítica e identificar qué factores influyeron en estos resultados funcionales.
DiseñoEstudio de cohorte ambispectivo.
EntornoUnidad de Cuidados Intensivos Pediátricos (UCIP) de un centro académico terciario.
ParticipantesNiños (1 mes-17 años) y sus cuidadores.
IntervencionesNinguna.
Principales variables de interésEstado demográfico, clínico y funcional.
ResultadosDe 242 niños examinados, 128 completaron el seguimiento. Estos niños y adolescentes cambiaron su estado funcional significativamente con el tiempo (p<0,001). El deterioro funcional ocurrió en el 62% de los niños al momento del alta y, después de un año, fue persistente en el 33%. La edad >12 meses fue un factor protector contra malos resultados funcionales en dos modelos de regresión (p<0,05). Un estado funcional moderadamente anormal y severamente/muy severamente anormal al alta aumentó el riesgo de resultados funcionales deficientes en 4,14 (IC95% 1,02-16,72; p=0,04) y 4,76 (IC95% 1,19-19,0; p=0,02). Una disminución funcional en el momento del alta aumentó los riesgos de resultados funcionales deficientes a largo plazo en 6,86 (IC95% 2,16-21,79; p=0,001), independientemente de las puntuaciones de FSS.
ConclusiónEste es el primer estudio que evalúa los resultados funcionales a largo plazo después de enfermedades críticas pediátricas en América Latina. Nuestros datos son básicos y plantean preguntas relevantes para futuros estudios multicéntricos en América Latina y pueden contribuir a una mejor comprensión de los efectos de enfermedades críticas en los resultados funcionales a largo plazo en niños.
The development of new morbidities after pediatric critical care became the focus of assessing pediatric critical care outcomes over the years.1–5 In the general pediatric intensive care units (PICUs), morbidity rates represent twice the mortality rates.2,6 Currently, the rates of children surviving critical illnesses and returning to their homes with a functional status decline vary between 68% and 85.1%.1,7 Thus, the assessment of functional status became relevant to measuring health status and has been increasingly recognized as an important outcome in the PICUs.3 The functional status is related to the individual capacity for developing daily activities. And recently, the impairments in functional status, including physical, cognitive, social, and emotional function after critical illness, are recognized as post-intensive care syndrome in pediatrics (PICs-p).8,9
The PICs-p, when not early identified and treated, may result in child developmental delays, changing the family routine, and impacting the quality of life of the whole family.1,10,11 Also, these children surviving critical illnesses frequently go home with technological dependency,12 increasing costs for families and the healthcare system.13 However, evidence following these children's functional outcomes in the long term is still limited.14
The few studies describing long-term functional outcomes are from high-income countries PICUs sets1,6,15,16 with different resources that do not represent low and middle-income countries. Moreover, based on the latest literature,17 there is a lack of long-term functional outcomes studies focused on general PICU survivors in Latin America.
Identifying factors associated with long-term poor functional outcomes is needed to prevent harm and improve rehabilitation strategies.14 Thus, this research's primary aim was to assess children's functional status one year after critical illness. The secondary aim was to verify whether preexisting characteristics and critical illness factors influenced these children's long-term functional outcomes.
Patients and methodsDesign and settingThis was an ambispective cohort study. Participants were previously selected in a cross-sectional study developed in a single-center tertiary PICU.7 This PICU admits clinical and surgical patients, except for trauma and cardiac surgery, from 1 month to 18 years. For the present study, we follow PICU survivors one year after PICU discharge. The Research Ethics Committee from Hospital de Clínicas de Porto Alegre approved this study (2.646.290). All caregivers signed the informed consent form.
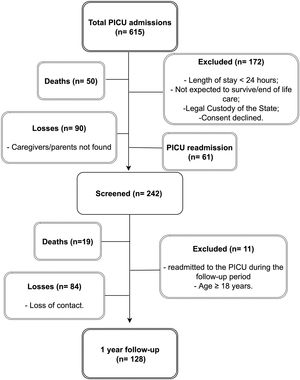
ParticipantsAll children aged one month to 16 years and 11 months previously recruited in the cross-sectional study7 (September 2016–October 2017) were evaluated for eligibility for this follow-up one year after discharge from the PICU (September 2017–October 2018). The previous exclusion criteria were: PICU length of stay<24h, children who returned to the PICU in the same hospitalization, children in the custody of the State, and end-of-life palliative care. For the follow-up, we excluded children readmitted to the PICU, those who had completed 18 years old, and who died. For children readmitted to the PICU in a different hospitalization, we only considered the information about the last discharge.
The original sample mainly consisted of males (62.7%), aged from one month to 12 months (38%), with preexisting chronic disease (66%), admitted to the PICU with respiratory diagnosis (43%).7
Sample sizeDue to a follow-up sample loss higher than expected, we calculated the power of our analysis. With a sample size of 128 patients, considering a significance level of 5%, and using an exact method, our sample has a statistical power of 90.2% to detect a 33% proportion of functional decline after a year (the proportion we detected). A multiple regression analysis was considered with ten planned predictors and respecting the rule of 10 patients for each predictor variable.
Data collection and outcomesParticipants’ previous information, including baseline functional status, clinical data, and discharge functional status, were collected from the previous study digital database.7 We collected follow-up information through telephone interviews with the caregivers.
The admission motive/diagnosis was classified as follows: neurologic, respiratory, others (metabolic, gastrointestinal, hematologic/oncologic, genetic) and surgical.2,15 The pre-existing chronic condition was defined as a medical diagnosis that required more health-related services than normally expected for children, including technology dependence.18,19 We considered an adverse event/complication any injury or damage associated with patient care during the critical illness that could not be explained by the diagnosis or PICU admission reason.20 That includes care-associated infections, post-procedural complications, health care-associated infections, and cardiorespiratory arrest.
We used the Functional Status Scale-FSS-Brazil to assess children's functional status.21 The FSS scale categorizes functional status as follows: normal (6–7 points); mildly abnormal (8–9); moderately abnormal (10–15); severely abnormal (16–21); very severely abnormal (>21).22 The functional status at baseline and PICU discharge were consulted from our previous study's database.7 We defined a functional decline on discharge from the PICU as a worse classification of FSS total scores compared to baseline. The third functional evaluation was accomplished by telephone interview a year after the patient's PICU discharge, in which parents/caregivers were asked about their child's current functional condition.15,22 Unanswered calls were considered losses after five attempts made on different days.
Data analysisData are presented as median (first, third quartile) or count (percentages). The total sample was split into two groups according to the functional outcome (good or poor). We used the Mann–Whitney U test, Pearson's Chi-squared test, Yates Continuous Correction, or Fisher Exact test to verify differences between the two outcome groups. Differences in the FSS scores across time were checked using the Friedman Test, with Dunn-Bonferroni post-hoc. Differences were considered statistically significant if p≤0.05.
The primary outcome of our analysis was a worsening in the FSS total scores in the third functional evaluation (a year after PICU discharge) compared with the baseline. For the multivariable analysis, we coded this information as a binary variable “Functional decline=poor functional outcome,” “no change in total FSS scores=good functional outcome.” We identified factors independently associated with long-term outcomes using multiple Poisson regression with a robust error variance estimation. Due to the sample size, we grouped patients with severe abnormal and very severe abnormal into one combined severe/very severe category.
Variables presented p<0.20 in the univariate analysis were considered when assembling the final regression models. The multicollinearity between variables was tested. All statistical analyses were performed using the SPSS version 21.0. for Windows.
ResultsFig. 1 shows the patient flow chart. During the recruitment period, 615 admissions occurred in our PICU. Our original sample consisted of 303 PICU admissions; of these, 61 were readmissions. Therefore, excluding readmissions, 242 patients were previously screened. However, 19 patients died over one year, 11 were excluded due to readmission to the PICU or reaching 18 years old during the follow-up period, and 84 families were considered lost contacts. There were no relevant differences between the study cohort and the lost follow-up group (Supplemental Digital Content 1). Thus, a total of 128 patients completed the year follow-up. The sample characteristics and the comparison between the two groups (good and poor outcomes) are shown in Table 1.
Sample general characteristics and association between variables and one-year outcomes.
| Functional outcome | ||||
|---|---|---|---|---|
| Variables | Total samplen=128 (100%) | Goodn=86 (100%) | Poorn=42 (100%) | p |
| Pre-existing characteristics | ||||
| Age, months | 16 (5–54) | 18 (6–78.75) | 11 (3–37.25) | 0.04b |
| Sex, male | 81 (63) | 54 (63) | 27 (64) | 1.00a |
| Premature birth | 41 (32) | 22 (26.5) | 19 (45) | 0.05a |
| Chronic condition | 91 (71) | 57 (66) | 34 (81) | 0.13a |
| Baseline functional status | ||||
| Good/normal | 88 (69) | 68 (79) | 20 (48) | 0.001c |
| Mildly abnormal | 29 (23) | 12 (14) | 17 (40) | |
| Moderately abnormal | 11 (8) | 6 (7) | 5 (12) | |
| Critical illness factors | ||||
| PIM2 | 1.25 (0.46–2.90) | 1.25 (0.42–3.15) | 1.33 (0.51–2.72) | 0.74b |
| Admission reason | ||||
| Neurologic | 13 (10) | 5 (6) | 8 (19) | 0.10c |
| Respiratory | 37 (29) | 24 (28) | 13 (31) | |
| Surgical | 48 (37) | 35 (41) | 13 (31) | |
| Others | 30 (23) | 22 (25) | 8 (19) | |
| Sedative | 96 (75) | 64 (74) | 32 (76) | 1.00a |
| Sedative time, days | 1 (1–4) | 1 (1–3.25) | 1 (0.75–4.25) | 0.48b |
| Neuromuscular blockade | 24 (19) | 17 (20) | 7 (17) | 0.85a |
| Adverse event/complication | 42 (33) | 23 (27) | 19 (45) | 0.05a |
| IMV use | 68 (53) | 42 (49) | 26 (62) | 0.22a |
| IMV time, days | 1 (0–4) | 0 (0–4) | 1.5 (0–8.25) | 0.06b |
| PICU length of stay | 5 (3–10) | 5 (3–8.5) | 6.5 (4–13.25) | 0.07b |
| Functional decline at PICU discharge | 79 (62) | 3 (7) | 39 (93) | <0.001a |
| Discharge functional status | <0.001d | |||
| Good/normal | 41 (32) | 39 (45) | 2 (5) | |
| Mildly abnormal | 28 (22) | 24 (28) | 4 (9) | |
| Moderately abnormal | 45 (35) | 21 (24) | 24 (57) | |
| Severely/very severely abnormal | 14 (11) | 2 (2) | 12 (28) | |
Variables are described as n (%) or the median (interquartile range: 25–75), Functional outcome evaluated according to FSS total scores, Good (FSS total score unchanged or better), Poor (FSS total score changed for worst). Age in months is referred the age at PICU admission. PIM2=Pediatric Index of Mortality; IMV=invasive mechanical ventilation.
One year after critical illness, 42 (33%) patients presented functional decline. As shown in Table 1, the groups good and poor long-term functional outcomes presented differences regarding the following factors: age, premature birth, baseline functional status, adverse event/complication, functional decline, and functional status at PICU discharge (p≤0.05). A total of 79 (62%) patients had a functional decline at PICU discharge.
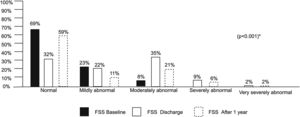
Fig. 2 illustrates a significant difference in functional status over time (p<0.001). Most children had a baseline functional status normal 69% and mildly abnormal 23%, and none were classified as having a severe or very severe abnormal baseline functional status. However, at PICU discharge, the number of children classified with a normal and mildly functional status reduced to 32% and 22%, respectively. On the other hand, the number of children with moderately abnormal functional status increased from 8% (baseline) to 35% at discharge, remaining at 21% within one year after discharge from the PICU. Furthermore, although no child was classified as having a severe or very severe baseline functional status, at PICU discharge, the number of children classified as having a severe functional status increased by 9%, and a very severe abnormal functional status increased by 2%. One year after PICU discharge, 6% of children still presented a functional status severely abnormal and 2% a functional status very severely abnormal.
Comparison between FSS scores across the time (baseline, PICU discharge, and one year). * Friedman test.. Pairwise comparisons (Dunn-Bonferroni post-hoc): FSS baseline x FSS discharge p=0.007; FSS baseline x FSS after one year p<0.001; FSS discharge x FSS after one year p<0.001. PICU=pediatric intensive care unit. FSS=functional status scale.
Tables 2 and 3 present two different multiple regression models to predict the one-year functional outcome, one considering the functional status at PICU discharge (categorized) and the second regarding the presence of functional decline at PICU discharge (compared with baseline) (simple regression analysis are on Supplemental Digital Content 2). In both models, age at admission and functional conditions at discharge (functional status or functional decline at PICU discharge) were independently associated with poor functional outcomes after one year.
Multiple regression analysis of variables related to the one-year functional outcome, considering the functional status at pediatric critical care discharge as a factor.
| Model I (p<0.001) | Model I Adjusted* (p=0.009) | |||
|---|---|---|---|---|
| Variables | RR (CI 95%) | p | RR (CI 95%) | p |
| Admission age, months | 0.05 | 0.01 | ||
| 1–12 | Ref. | – | Ref. | – |
| 13–48 | 0.59(0.36–0.97) | 0.04 | 0.38(0.19–0.74) | 0.004 |
| ≥49 | 0.60(0.34–1.06) | 0.08 | 0.52(0.25–1.06) | 0.07 |
| Discharge functional status | <0.001 | 0.08 | ||
| Good/normal | Ref. | – | Ref. | – |
| Mildly abnormal | 2.68(0.52–13.67) | 0.23 | 2.33(0.45–12.08) | 0.31 |
| Moderately abnormal | 9.63(2.43–38.04) | 0.001 | 4.14(1.02–16.72) | 0.04 |
| Severely/very severely abnormal | 17.40(4.47–67.77) | <0.001 | 4.76(1.19–19.0) | 0.02 |
Multiple regression analysis of variables related to the one-year functional outcome, considering the functional decline at the pediatric critical care discharge as a factor.
| Model II (p<0.001) | Model II adjusted* (p<0.001) | |||
|---|---|---|---|---|
| Variables | RR (CI 95%) | p | RR (CI 95%) | p |
| Admission age, months | 0.20 | 0.003 | ||
| 1–12 | Ref. | – | Ref. | – |
| 13–48 | 0.72(0.43–1.21) | 0.22 | 0.44(0.25–0.77) | 0.005 |
| ≥49 | 0.58(0.29–1.15) | 0.12 | 0.48(0.26–0.87) | 0.01 |
| Functional decline at discharge | 7.45(2.42–22.95) | 0.001 | 6.86(2.16–21.79) | 0.001 |
Model adjusted by baseline functional status. Dependent variable: Functional outcome after one year (good/unchanged, poor). Functional decline was considered a worsening in total FSS scores classification comparing with baseline. RR=Relative risk; CI 95%=Confidence interval; Statistical significance=p<0.05.
Table 2 shows a multiple regression analysis considering the functional status at PICU discharge as an influencing factor. Patients aged between 13–48 months had a reduction of 0.38 (CI 95% 0.19–0.74, p=0.004) in the risks of poor functional outcomes compared with younger patients. On the other hand, a moderately abnormal functional status at PICU discharge increased the risks of long-term poor functional outcomes in 4.14 (CI 95% 1.02–16.72; p=0.04). The risks for long-term poor functional outcomes increased even more in children with severe/very severe abnormal functional status at PICU discharge, 4.76 (CI 95% 1.19–19.0; p=0.02).
In Table 3, considering the functional decline at PICU discharge as an influencing factor, age over 12 months again represented a protective factor against long-term poor functional outcomes (p=0.003). In addition, a functional decline at PICU discharge increased in 6.86 (CI95% 2.16–21.79; p=0.001) the risks of long-term poor functional outcomes.
DiscussionAfter one year, 33% of the children still had some functional decline. In addition, age at admission and functional status at discharge were independently associated with poor functional outcomes after one year. Our data provide information about significant changes in functional status over time and identify factors related to long-term functional outcomes in a cohort of children after critical illness in Brazil. Based on the latest literature,17 this is the first study to evaluate long-term functional outcomes in Latin American children after critical illnesses and one of the few in this field to consider baseline functional status evaluation, which is relevant for PICU outcomes evaluation.9 Some studies already reported factors related to functional outcomes of children after critical illnesses.1,11,22,23 However, these studies were developed in high-income countries with different resources and health care systems than most Latin American Countries.
Identifying functional changes over time in children after critical illnesses and understanding which factors are related to poor functional outcomes may improve clinical practice and contribute to the development of rehabilitation strategies focused on these patients’ needs. For example, the improvement of early mobilization strategies, recently highlighted as safe and important to prevent functional impairments in children,24–26 and supporting post-PICU rehabilitation plans focused on these survivors’ needs.
The levels of functional impairment at PICU discharge found in our study seem high compared to the range of functional impairment reported by previous studies, 5.2–36%,3,5,6,15,27 including studies that used the same functional status evaluation tool (FSS). Another study from the same PICU also found high levels of functional impairment, reporting 86% of global morbidity at PICU discharge.28 However, the authors used the Pediatric Cerebral Performance Category (PCPC) and the Pediatric Overall Performance Category (POPC) and did not follow patients after PICU discharge. Our findings are similar to those reported by a study developed with 181 patients in two Canadian PICUs, which applied the Pediatric Evaluation of Disabilities Inventory Computer Adaptive Test (PEDI-CAT) and found a high level of functional decline (81.5%) at PICU discharge and 55.7% of functional impairment six months after discharge.1 Another North American study that followed PICU functional outcomes six months and three years after discharge reported 38% of functional status worsening or dead after three years.15 It is believed that the extensive variability of new functional impairments between studies may be explained by each PICU patient profile, each country's level of income, and the choice of measurement tools.3 This high variability range between studies also limits the comparisons between findings.17
In our two multiple regression models, age at admission was independently associated with long-term poor functional outcomes. Age over 12 months represented a protective factor against poor long-term functional outcomes, and that is new. We found just one study that reported similar findings. The North American multicenter study reported that new morbidities occurred in all age groups, but more often in infants.2 However, this study evaluated new morbidities at hospital discharge and did not follow children after that. We found no other studies reporting the influence of young age on long-term functional outcomes in critically ill children, which may highlight the lack of long-term outcomes data in pediatric intensive care. Also, this finding can be related to the profile of patients admitted to our PICU since most were infants under two years. Anyhow, an episode of critical illness during childhood is stressful for children and their families.29 In addition, it is known that during the first years of life, the experiences offered through the environment play a crucial role in promoting conditions for healthy development and growth, influencing long-term development.30,31
A functional status moderately abnormal increased by 4.14 the risks of long-term poor functional outcomes, and patients classified as having severe/very severe abnormal functional status were even more at risk of poor outcomes in our study. This association between the functional status at PICU discharge measured by FSS and long-term poor functional outcomes was previously reported in a 3-year cohort study.15 The authors found long-term poor functional outcomes in patients who had worse functional status classification at the discharge. Similarly, another study1 reported an independent association between a greater degree of functional decline at PICU discharge, increased hospital length of stay, and worse functional outcomes after six months. However, a different tool was used. Anyhow, in our study, regardless of the FSS classification, just considering a functional decline compared to baseline status, the functional decline at discharge represented an increase of 6.86 in the risks of long-term poor functional outcomes. On the other hand, a recent multicenter study developed in the USA, which also used the FSS as a tool, did not find an association between long-term outcomes and hospital discharge functional status.32 However, this study was a follow-up only focused on children discharged from the hospital with substantial new functional status morbidity, limiting comparison with our findings. Other studies reported the disease's severity, invasive therapies (invasive mechanical ventilation, extracorporeal membrane oxygenation), length of stay, and cardiopulmonary resuscitation, as poor functional outcomes influencing factors.5,23,33,34 Still, most of these studies investigated children with specific illnesses, and the risk factors were related to short-time outcomes.
The single-center study limits our findings. The sample was representative of our tertiary PICU concerning admission motive, age, and previous chronic condition. Our data highlight the need for a more extensive study to overcome the limitations found in this study. Although we had a loss of sample higher than expected, there were no relevant differences between the study cohort and the lost follow-up group. In addition, the power of our statistical analysis was 90.2%. But, on the other hand, the categorization of some continuous variables may have affected the power of our results. Also, we made the long-term evaluation by telephone interview with caregivers, which can cause some inaccuracy in the data collection. However, this data collection model for long-term outcomes was also used by other studies, including some of the FSS authors.15,23,35,36 We were also unable to collect information about rehabilitation impact since these children did not have standardized rehabilitation follow-up care after critical illness. We understand that Brazil is a continental country with resource differences, and seasonal illness, varying significantly between regions, which may influence the results. Therefore, we believe a multicenter study is needed to understand better the influence of the critical illnesses on children's functional outcomes. Despite the limitations, we believe that our findings can be considered baseline data in Brazil and other Latin American countries as we raise relevant questions for future multicenter studies in this field.
The prevention and early identification of functional impairments are essential health care priorities for PICUs, as reported by recent literature.37 In addition, the functional impairment can become persistent if not identified and treated early, affecting children's functional independence, causing development delays, frequent hospital readmission, and increasing costs for the health care system and families.8,13 Furthermore, the long-term functional status reflects on the quality of life and is considered essential for child development and a family-centred care strategy.10,38
ConclusionsOur research shows significant changes over time in the functional status of a cohort of children after critical illnesses in Brazil. One year after discharge from the PICU, 33% of the children still had a functional decline. In addition, age at admission and functional status at discharge were independently associated with poor functional outcomes after one year.
Authors’ contributionsVCD had substantial contributions to the study, including conceptualization, methodology, acquisition of data, literature review, data analysis and interpretation, writing—original draft.
PMER and PRAC had substantial contributions to the study, including conceptualization, methodology, project administration, supervision, writing—review, editing and final approval.
Ethical approvalThis study was approved by the Research Ethics Committee in our institution (CEP-HCPA) with the approval number 2.646.290. All caregivers signed the informed consent form.
Data availabilityThe data supporting this study's findings are available on request from the corresponding author VCD and after approval for the ethics committee of our institution.
FundingThis research was partially supported by CAPES – Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Ministério da Educação – Brazil, CNPq Conselho Nacional de Desenvolvimento Científico e Tecnológico, and Fundo de Incentivo à Pesquisa e Eventos – FIPE, Hospital de Clínicas de Porto Alegre.
Conflict of interestNo financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
We want to thank all children and parents who kindly collaborated with this study.