Editado por: Rosario Amaya Villar - Unidad de Cuidados Intensivos, Hospital Universitario Virgen del Rocio, Sevilla, España
Última actualización: Febrero 2024
Más datosAcute respiratory distress syndrome (ARDS) is a frequent condition in the intensive care unit (ICU).1 It is clinically manifested by hypoxemic respiratory failure, airspaces flooding by inflammatory edema, and regional lung collapse due to “gas compression” of the dependent lung regions.2 Hypoxemia is due to a ventilation/perfusion mismatch, especially in a heterogeneously ventilated and perfused lung.3 Prone positioning (PP) has shown to improve oxygenation and survival in selected ARDS patients. In addition, PP has been associated with recruiting of dorsal lung regions, with a more homogeneous ventilation and a reduction of pleural pressure gradient contributing with an improvement in the ventilation/perfusion (V/Q) ratio.4,5
Electrical Impedance Tomography (EIT) is a bedside non-invasive monitoring tool of ventilation and perfusion distribution. Several studies have demonstrated EIT's benefits in establishing ventilatory parameters and its role in assess the lung perfusion in ARDS.6 Thus, in this study we aimed to analyze PP's effects on the distribution of pulmonary ventilation and perfusion in patients with severe ARDS connected to mechanical ventilation (MV).
These data were presented preliminary as a poster in ESICM 2021.7
This is an observational sub-study of an already finished clinical study (Nº 170315007) which was conducted on patients admitted to the Intensive Care Department of the Hospital Clínico UC-Christus (Santiago, Chile), between November 2019 and March 2020 and required EIT as part of the ventilatory multimodal monitoring protocol. Considering that EIT perfusion measurements were indicated by attending physicians as an alternative diagnostic approach (i.e., thromboembolic disease), a waiver to use this data was requested to the ethical-scientific committee of the Pontificia Universidad Católica de Chile (Nº 210510004).
Patients with moderate to severe ARDS were included. PP was indicated by the attendant physician according to ICU protocols. The distribution of pulmonary ventilation and perfusion was evaluated with EIT (Enlight 1800, Timpel, São Paulo, Brazil) in the supine position (SP) and then in prone 2 h after proning. Impedance Ratio (IR) and Global Inhomogeneity (GI) indices were obtained from the EIT data, and arterial blood gases, hemodynamic parameters, and ventilatory mechanics were registered in each position.
The ventilation and perfusion maps delivered by EIT were divided into four regions of interest (quadrants), and in two gravitational regions (ventral and dorsal). For the regional analysis of the V/Q relationship we used the Pearson Correlation Coefficient. Values are expressed as mean ± standard deviation (SD). Comparisons of physiological changes between SP and PP were performed with paired Student's t-test, using GraphPad Prism (GraphPad Software, San Diego, CA, USA). The level of significance was established at a P-value ≤ 0.05.
Eight patients with pneumonia (57 ± 11 years, 50% female) were included. Hemodynamic parameters were similar in both positions.
During PP, we found a significant increase in PaO2/FIO2 (206 ± 32 vs. 125 ± 34 mmHg, p < 0.005) and in respiratory system compliance (33.8 ± 6 vs. 30.3 ± 6 ml/cmH2O, p = 0.02), associated to a decrease in driving pressure (10.8 ± 2.1 vs. 12.3 ± 2.5 cmH2O, p = 0.04), as compared to SP. PEEP setting was 9.4 ± 2.9 cmH2O during PP, and 9.2 ± 3.7 cm H2O during SP.
We observed a redistribution of ventilation (Impedance ratio) from ventral regions in SP to dorsal regions in PP in all patients (0.77 ± 0.3 to 2.23 ± 0.9 AU, p = 0.007). Such rearrangements were associated with ventilation homogenization, as indicated by a decrease in GI from 1.24 ± 0.3 to 0.82 ± 0.1 (AU) (p = 0.02).
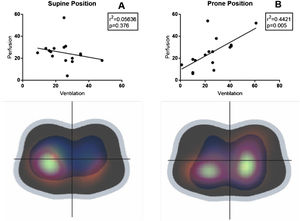
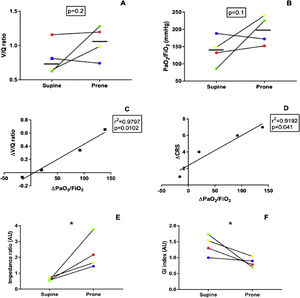
Four of the eight patients were subjected to pulmonary perfusion assessment. Perfusion was predominantly dorsal in both SP and PP. Regional distribution of ventilation and perfusion (quadrants) exhibited a positive linear correlation in PP (R2 = 0.44, p = 0.005), but not in SP (R2 = 0.056, p = 0.37) (Fig. 1), suggesting the optimization of the V/Q mismatch with PP. In addition, we observed a good correlation (R2 > 0.9) between changes of PaO2/FiO2, dorsal V/Q ratio, and the change of respiratory system compliance (Fig. 2).
Individual changes in dorsal ventilation/perfusion ratios (V/Q, A) and oxygenation (PaO2/FIO2, B) and from supine to prone positioning in the dorsal lung regions. Relationships between changes in PaO2/FIO2 and V/Q ratios of the dorsal lung regions are represented in C and between changes in PaO2/FIO2 and the CRS in panel D. A different color represents each patient. Changes in EIT indices are shown in E and F. V: ventilation: Q: perfusion; PaO2: arterial partial pressure of oxygen; FIO2: fraction of inspired oxygen, CRS: Respiratory system compliance, GI: global inhomogeneity index, AU: arbitrary units, * = p < 0.05.
This observational study suggests that prone PP in mechanically ventilated patients with ARDS was associated with a change in the ventilation distribution pattern to dorsal lung regions; and homogenization of gas and perfusion distribution, resulting in improved V/Q ratio. In addition, the change of dorsal V/Q ratio was good correlated with the individual change of oxygenation and respiratory mechanics.
The PP promoted a significant improvement in oxygenation and lung mechanics, which is in line with previous reports.8 The improved oxygenation was directly correlated to improvements in the dorsal V/Q ratio (Fig. 2). Improved V/Q could be explained by diversion of ventilation to dorsal lung regions, due to changes in the superimposed pressure gradient9 in the presence of a dorsal dominance of perfusion. These findings have been previously demonstrated in other settings, such healthy volunteers, and experimental models of lung injury.10
In this small series of patients, we observed that PP improved gas exchange and pulmonary mechanics through a change in the distribution of ventilation towards the dorsal regions of the lungs and promoting a more homogeneous ventilation distribution. Analysis of V/Q ratio through EIT could provide bedside, real-time, and individual information on the effectiveness of the prone maneuver and possibly predict tolerance to position changes. New studies with a larger number of patients are necessary to validate these findings.
FundingThis work was supported by project grant FONDECYT 1171810 from Fondo Nacional de Desarrollo Científico y Tecnológico, Chile 2017.
Conflicts of interestAuthors declare no conflicts of interest.
We would like to thank Vanessa Oviedo, Luis Felipe Damiani, Yorschua Jalil, and David Carpio for their technical support and valuable contribution.