Endovascular techniques have become an essential tool for the treatment of descending thoracic aortic disease (thoracic endovascular aneurysm repair [TEVAR]). The aim is to analyze the indications and outcomes of emergency TEVAR at national level in relation to elective surgery.
Study design and scopeA retrospective multicenter registry of patients with descending thoracic aortic disease treated on an emergency basis using endovascular techniques between 2012–2016, in 11 clinical units.
Patients, inclusion criteria1) Ruptured descending thoracic aortic aneurysms (RTAA); 2) Blunt traumatic thoracic aortic injury (TAI); and 3) Complicated acute type B aortic dissections (TBADc).
Primary variablesPatient mortality, survival and reoperation rate.
Secondary variablesDemographic data, cardiovascular risk factors, specific data by indication, technical resources and postoperative complications.
ResultsA total of 135 urgent TEVARs were included (111 men, mean age 60.4 ± 16.3 years): 43 ruptured thoracic aortic aneurysms (31.9%), 54 type B dissections (40%) and 32 traumatic aortic injuries (23.7%), and other etiologies 4.4%. The overall mortality rate at 30 days was 18.5%, and proved higher in the RTAA group (27.9%). The mean actuarial survival rate was 67 ± 6% at 5 years. The postoperative stroke rate was 5.2%, and the paraplegia rate was 5.9%. Aortic reoperations proved necessary in 12 patients (9%).
ConclusionsEmergency descending thoracic aortic diseases can be treated by endovascular techniques with optimal results and low morbidity and mortality — though the figures are slightly higher than in elective cases. This registry provides, for the first time, real information on the daily clinical practice of emergency TEVAR in Spain.
Las técnicas endovasculares se han convertido en una herramienta esencial para el tratamiento de la patología de aorta torácica descendente (TEVAR). El objetivo es analizar las indicaciones y resultados del TEVAR urgente a nivel nacional en relación con la cirugía programada.
Diseño y ámbito de estudioRegistro multicéntrico retrospectivo de pacientes con patología de aorta torácica descendente tratados de urgencia mediante técnicas endovasculares entre los años 2012–2016 en 11 servicios clínicos.
Pacientes, criterios de inclusión1) Aneurismas de aorta torácica rotos (AATR), 2) roturas traumáticas de aorta torácica (TAT) y 3) disecciones de aorta torácica tipo B (DATBc) complicadas.
Variables principalesMortalidad, supervivencia y tasa de reintervenciones.
Variables secundariasDatos demográficos, factores de riesgo cardiovasculares, datos específicos por indicación, datos técnicos y complicaciones postoperatorias.
ResultadosSe obtuvieron 135 TEVAR urgentes (111 varones, edad media 60,4 ± 16,3 años): 43 aneurismas aórticos rotos (31,9%), 54 disecciones tipo B (40%) y 32 roturas aórticas traumáticas (23,7%) y otras etiologías 4,4%. La mortalidad global a los 30 días fue del 18,5%, siendo superior en los AATR (27,9%). La supervivencia media actuarial ha sido del 67 ± 6% a los 5 años. La tasa de ictus postoperatoria fue del 5,2% y la tasa de isquemia medular del 5,9%. Las reintervenciones aórticas fueron necesarias en 12 pacientes (9%).
ConclusionesLa patología de aorta descendente urgente puede ser tratada mediante técnicas endovasculares con resultados óptimos y baja morbimortalidad, aunque ligeramente superior a los casos electivos. Este registro aporta por primera vez, información de la realidad clínica diaria del TEVAR urgente en España.
Until a little over a decade ago,1 repair of the thoracic aorta was performed adopting the classical open surgery (OS) approach, which was regarded as the gold standard. The application of thoracic endovascular aneurysm repair (TEVAR) techniques in both emergency and elective surgery has produced a genuine revolution in this field. They can be used for the emergency treatment of complex lesions of the thoracic aorta, such as complicated acute type B aortic dissection (TBADc), ruptured thoracic aortic aneurysm (RTAA), intramural hematomas, penetrating aortic ulcers, traumatic thoracic aortic rupture (TTA), etc. The evidence in the international literature shows that TEVAR can reduce patient mortality,2–4 paraplegia and the overall complications rate compared with OS, and this has established TEVAR as the management of choice in high-risk patients in critical condition.
Endovascular treatment involves the placement of an endoprosthesis (stent) via a femoral access, under fluoroscopic control, with the purpose if isolating the lesions. A priori, these techniques are less invasive than conventional OS, which results in lesser morbidity–mortality.5 This novel treatment option is not without severe complications, however. Specifically, the complications can be classified into two groups: those related to the device (endoleakage, stent migration or rupture, etc.), and ischemic complications secondary to embolic events (paraplegia, spinal cord ischemia or cerebral ischemia, etc.).6
To date there have been no randomized clinical trials involving any of the indicated disease conditions, supporting the superiority of emergency endovascular treatment versus OS, and most of the available scientific evidence is based on international case series and registries.7,8
The aim of the present observational study was to analyze real life practice in terms of the indications and outcomes of TEVAR in emergency situations, based on the data of a multicenter registry (Regis-TEVAR). This is the first publication of the outcomes of emergency TEVAR at Spanish national level.
Patients and methodsStudy design and settingThe Endovascular Surgery Chapter (CCEV) of the Spanish Society of Angiology and Vascular Surgery (Sociedad Española de Angiología y Cirugía Vascular [SEACV]) invited all the Departments of Angiology and Vascular Surgery in Spain to participate in a multicenter retrospective registry of patients with descending thoracic aorta disease treated on an emergency or elective basis using TEVAR techniques. Eleven Departments agreed to participate in the compilation of data on patients operated upon in the period 2012–2016, following approval from the local Ethics Committees.
Patients or participantsA total of 287 patients were included in the national registry (Regis-TEVAR), divided into two groups according to whether surgery was elective (surgery that could be postponed at least 24 h) or constituted emergency or emergent surgery (i.e., surgery performed within less than 24 h). Of the 287 patients, 135 underwent emergency surgery and were selected as the study group. The following indications were included: RTAA, TTA and TBADc, as detailed in Appendix A (Table 1), available only as Supplementary material in the electronic version (inclusion and exclusion criteria). The main aim of our study was to conduct a descriptive analysis of the technical characteristics and outcomes of the patients subjected to emergency surgery, with the 152 patients subjected to elective surgery being used as a reference for the comparison of concrete aspects versus emergency surgery.
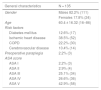
Demographic data and risk factors of the study population.
| General characteristics | N = 135 |
|---|---|
| Gender | Males 82.2% (111) |
| Females 17.8% (24) | |
| Age | 60.4 ± 16.32 (16–86) |
| Risk factors | |
| Diabetes mellitus | 12.6% (17) |
| Ischemic heart disease | 38.5% (52) |
| COPD | 22.2% (30) |
| Cerebrovascular disease | 10.4% (14) |
| Preoperative paraplegia | 2.2% (3) |
| ASA score | |
| ASA I | 2.2% (3) |
| ASA II | 2.9% (4) |
| ASA III | 25.1% (34) |
| ASA IV | 26.6% (36) |
| ASA V | 42.9% (58) |
Continuous data are reported as the mean ± standard deviation (range), while categorical data are reported as percentages and numbers.
ASA: anesthetic risk scale of the American Society of Anesthesiologists; COPD: chronic obstructive pulmonary disease.
From each patient we collected preoperative information, specific data according to the indication of repair, intraoperative data and postoperative data, comprising a total of 56 descriptive variables referred to the technique and outcome (Appendix A [Table 2], available only as Supplementary material in the electronic version). These variables had been previously validated by the VASCUNET (https://vascunet.org), the Working Committee of the European Society of Surgery Vascular (ESVS) created in 1997, with the purpose of collecting information from over 15 vascular registries in Europe, Australia and New Zealand.
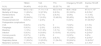
Specific data according to the type of disease condition affecting the descending thoracic aorta (DTA).
| Indications of emergency endovascular repair N = 135 | ||||
|---|---|---|---|---|
| Complicated acute type B aortic dissection (TBADc) | 54 cases (40%) | |||
| Type of complicationsa | ||||
| Visceral ischemia | 17 (31.5%) | |||
| Rupture | 12 (22.2%) | |||
| Refractory pain | 10 (18.5%) | |||
| Dilatation | 1 (1.9%) | |||
| Ruptured thoracic aortic aneurysm (RTAA) | 43 cases (31.9%) | |||
| Mean aortic diameter = 67.67 ± 22.4 mm | ||||
| Traumatic thoracic aortic rupture (TTA) | 32 cases (23.7%) | |||
| Lesion severityb | ||||
| Type I | Type II | Type III | Type IV | |
| 1 | 2 | 18 | 11 | |
| 3.1% | 6.3% | 56.3% | 34.4% | |
Severity of the thoracic aorta lesion according to the classification of Azizzadeh et al.9 Continuous data are reported as the mean ± standard deviation (range), while categorical data are reported as percentages and numbers.
We specifically analyzed the following for each disease condition: type of complication for emergency repair in the dissections, aortic diameter in the ruptured aneurysms and the grade of thoracic aortic traumatism (type I, type II, type III or type IV) according to the classification of Azizzadeh et al.9
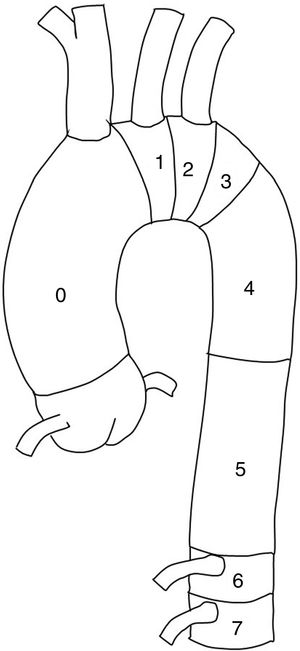
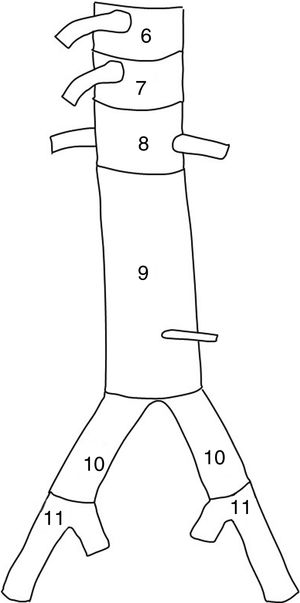
With regard to the surgical technique, we analyzed the number of stents placed and the proximal and distal anchoring zones according to the classification of Fillinger et al.10 (Figs. 1 and 2). Consideration was made of the type of endoprosthesis employed (Valiant, Zenith Alfa, Captivia, TAG, etc.), together with the percentage of branches of the aortic arch revascularized or covered during the procedure, as well as specifically which of the branches (left subclavian artery, left carotid artery, celiac trunk, superior mesenteric artery or renal arteries), with a view to assessing their association to possible postoperative complications. These clinical complications were: infection, postoperative bleeding requiring repeat surgery, postoperative paraplegia, cerebrovascular accident (CVA), acute coronary events, renal failure with a need for dialysis, respiratory failure and intestinal ischemia. We also analyzed survival at 30 days and over the 5-year follow-up period. We took into account the percentage of reinterventions, i.e., any type of endovascular procedure (extensions, embolizations, repeat angioplasty, etc.), with the purpose of correcting technical failures in the first 30 days.
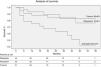
Continuous variables were reported as the mean ± standard deviation (SD). Categorical data were expressed as percentages. Patient survival – both perioperative and after up to 5 years – was assessed based on Kaplan–Meier analysis. Survival rates were compared using the log-rank test and Gehan test. Statistical significance was considered for p < 0.05. The SPSS version 24 statistical package was used throughout.
ResultsStudy populationA total of 287 patients were consecutively included, covering the period 2012–2016: 152 subjected to elective surgery and 135 to emergency surgery. Of the 135 emergency procedures, 111 corresponded to males (82.2%) and 24 to females (17.8%), from 11 Departments of Angiology and Vascular Surgery throughout Spain. The number of patients included per center ranged from 8 to 78 cases. The mean age was 60.4 ± 16.3 years among the emergency surgery cases (this being younger than the patients subjected to elective surgery, with 67.4 ± 11.15 years). A total of 12.6% of the patients presented diabetes mellitus, 38.5% suffered ischemic heart disease, and 22.2% presented chronic obstructive pulmonary disease (COPD). The main cardiovascular risk factors are reported in Table 1. With regard to risk status, 42.9% of the patients subjected to emergency surgery (58 cases) presented a preoperative ASA (American Society of Anesthesiologists) score of V, versus only 2% of the patients subjected to elective surgery.
The most frequent indication of emergency TEVAR was complicated type B dissections, with 54 cases (40%), followed by RTAA with 43 cases (31.9%), TTA with 32 cases (23.7%) and other less frequent conditions such as intramural hematomas and complicated penetrating ulcers (4.4%) (Table 2). The mean diameter of the thoracic aorta in the 43 cases of ruptured aneurysms was 67.67 ± 22.4 mm — this being greater than the aortic diameter in the cases of elective repair (61.31 ± 16.05 mm).
Of the 54 cases with TBADc, 31.5% initially manifested in the form of visceral ischemia, 22.2% as aortic rupture and 18.5% in the form of pain refractory to treatment, obliging emergency repair. With regard to TTA (32 cases), a total of 56.3% were lesions classified as type III or pseudoaneurysms, while 11 (34.4%) were classified as type IV (aortic rupture) according to the classification of Azizzadeh et al.9
Surgical techniqueThe present study did not include data such as the type of femoral access (percutaneous versus open), the use of ultrasound (transesophageal ultrasound or intravascular ultrasound [IVUS]), lumbar cerebrospinal fluid (CSF) drainage, etc. We analyzed the type of endoprosthesis used (Gore TAG, Relay, Valiant, etc.) and the number of stents placed — no statistically significant differences being observed. Anchoring of the endoprosthesis was proximal to the left subclavian artery (LSA), specifically in zones 0 and 1 (Fig. 1) in only 2.2% of the cases, representing coverage of three left carotid arteries, all revascularized in the same surgical step. In turn, 41.5% of the TEVARs were anchored in zone 2, representing the coverage of 58 LSAs (43% of the total), of which only 6 were revascularized (4.4% of the cases) — this being far lower than the 30.9% of LSAs revascularized in the cases of elective repair (Table 3). No statistically significant differences were recorded in the paraplegia or CVA rates between the group of patients with covered and revascularized LSA and the cases in which such revascularization was not made. Distal anchoring (Fig. 2) was in zone 5 in 48.1% of the cases and in zone 4 in 38.5% of the cases — this representing a total of 86.6% of the distal anchorings above the celiac trunk without the covering of visceral branches. In turn, 8.9% of the endoprostheses were positioned in zones 6, 7 and 8, representing the covering of four celiac trunks (25% revascularized, when associating disease in the other two axes), two superior mesenteric arteries (100% revascularized), and four renal arteries (100% revascularized).
Main outcomes and complications according to the type of disease condition.
| TBADc | TAA | TTA | Emergency TEVAR | Elective TEVAR | |
|---|---|---|---|---|---|
| N (%) | 54 (40%) | 43 (31.9%) | 32 (23.7%) | 135 | 152 |
| Mean age | 60.13 ± 12.1 | 71.11 ± 11.5 | 45.5 ± 16.6 | 60.4 ± 16.32 | 67.4 ± 11.15a |
| Mortality at 30 days | 11 (20.4%) | 12 (27.9%) | 2 (6.3%) | 25 (18.5%) | 8 (5.3%)a |
| Reinterventions | 7 (13%) | 3 (7.1%) | 2 (6.3%) | 12 (9%) | 11 (7.3%) |
| Covered LSA | 35 (64.8%) | 7 (16.3%) | 15 (46.9%) | 58 (43%) | 54 (35.5%) |
| Revascularized LSA | 5 (9.3%) | 1 (2.3%) | 0 | 6 (4.4%) | 47 (30.9%)a |
| Postoperative complications | |||||
| CVA | 5 (9.3%) | 2 (4.7%) | 0 | 7 (5.2%) | 2 (1.3%) |
| Paraplegia | 5 (9.3%) | 1 (2.3%) | 2 (6.3%) | 8 (5.9%) | 7 (4.6%) |
| Bleeding | 1 (1.9%) | 5 (11.6%) | 1 (3.1%) | 7 (5.2%) | 9 (5.9%) |
| Infection | 5 (9.3%) | 8 (18.6%) | 5 (15.6%) | 18 (13.3%) | 4 (2.6%)a |
| Coronary events | 2 (3.7%) | 1 (2.3%) | 0 | 3 (2.2%) | 3 (2%) |
| Hemodialysis | 10 (18.5%) | 5 (11.6%) | 2 (6.3%) | 17 (12.6%) | 4 (2.6%)a |
| Respiratory failure | 11 (20.4%) | 10 (23.3%) | 11 (34.4%) | 33 (24.4%) | 10 (6.6%)a |
| Mesenteric ischemia | 6 (11.1%) | 2 (4.7%) | 0 | 8 (5.9%) | 2 (1.3%)a |
The global mortality rate among the cases of emergency TEVAR was 18.5% (25 of the 135 patients died within the first 30 days after the operation) versus 5.3% in the cases of elective surgery (8/152) — though the difference was not statistically significant: 20.4% in TBADc, 27.9% in RTAA and 6.3% in TTA.
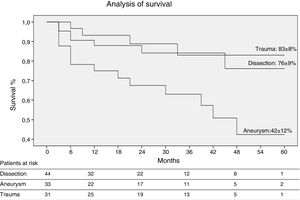
Survival was analyzed using the Kaplan–Meyer method for a maximum follow-up period of 60 months. A total of 67 ± 6% were still alive at the end of follow-up. The actuarial survival rate according to disease condition was 76% in the cases of TBADc, 42% in RTAA and 83% in TTA at 5 years (Fig. 3). The comparison of the survival rates according to the type of disease revealed statistically significant differences (Gehan test; p < 0.05).
Reinterventions during admission were required in 12 patients (9%), being more frequent in dissections (13%) than in the rest of the disease conditions. Sixty percent of these reinterventions were due to technical failures related with the devices, such as type I endoleakage, LSA occlusion failure, etc.
Immediate postoperative complicationsThe incidence of postoperative bleeding was 5.2%, and was higher in the case of ruptured thoracic aneurysms (11.6%) (Table 3). The incidence of infection in any location was 13.3% (18.6% in RTAA). Most of these infections were respiratory processes (11.1%), possibly due to the associated lung concussion and ventilation difficulties. In turn, the postoperative CVA rate was 5.2%, and was mainly associated with dissections (9.3%) — the percentage being considerably greater than the 1.3% in the cases subjected to elective surgery. The incidence of postoperative paraplegia was 5.9% (the highest figure again corresponding to dissections with 9.3%, versus 2.3% in RTAA and 6.3% in TTA). Coronary events were observed in 2.2% of the operated patients, and 12.6% required postoperative hemofiltration (18.5% in the case of dissections). Mesenteric ischemia was recorded in 5.9% of the cases, and was likewise more common among the dissections (11.1%). Of the patients with thoracic trauma, one-third suffered postoperative respiratory failure.
DiscussionAnalysis of mortality in emergency open surgery versus emergency endovascular repairEmergency lesions of the thoracic aorta, including TBADc, RTAA and TTA, are a management challenge. The emergency repair of these conditions is associated with high morbidity–mortality, and despite the advances in surgical techniques and perioperative management, this type of surgery continues to pose a very high risk.11 Although initially developed for the treatment of abdominal aneurysms, endovascular techniques have become the option of choice in emergency situations, since the morbidity–mortality reported in the literature is favorable to these techniques versus classical OS.12 A recent meta-analysis including 14,580 patients (10,672 subjected to OS and 3908 to endovascular techniques) has reported better perioperative outcomes with TEVAR, despite the fact that the patients presented greater surgical risk.13 However, there is still not enough evidence comparing the outcomes at 5 and 10 years between the two treatment strategies. Specifically, in the case of RTAA, the existing literature evidences an in-hospital mortality rate of between 24.6% and 45.6% for OS, while in the case of TEVAR the figure varies between 17.4% and 30%.14 In our series, the global mortality rate was 18.5%, though in the specific case of the mentioned disease condition the figure was 27.9% — the highest percentage of all three indications. A limitation of our study is the fact that we have not been able to compare our series with patients subjected to OS, since this was not the purpose of our research. The recent European guide on endovascular treatment of the descending thoracic aorta (Management of Descending Thoracic Aorta Diseases: Clinical Practice Guidelines of the European Society for Vascular Surgery [CPG-ESVS])14 recommends endovascular repair as the first option in cases of RTAA, provided the anatomical characteristics are suitable (recommendation 23: class I, level of evidence B).
In the case of TBADc, the aim of emergency repair in both OS and TEVAR is not only to cover the tear in the intima of the aorta but also to reduce the pressure in the false lumen, and thus improve perfusion of vital organs such as the intestine and kidneys. In our series, 31.5% of the cases of TBAD initially presented mesenteric ischemia as the main preoperative treatment indication. Although the outcomes of OS over TBADc have improved in recent decades, its complication rates remain high, and the mortality rate is between 25%–50%,16 due to the long surgery times and profuse bleeding. The CPG-ESVS considers OS in TBADc to be an alternative to endovascular treatment when the latter has failed or is contraindicated (recommendation 19: class IIa, level of evidence C). At present there are three meta-analyses with short- and middle-term outcomes referred to patients with TBADc and TEVAR, describing mortality rates between 2.6% and 9.8% (somewhat higher in our series: 20.4%) and a neurological complications rate of between 0.6% and 3.1%.17–19 The presence of visceral complications due to hypoperfusion is a predictor of greater mortality20; in this regard, one of the main advantages of TEVAR over OS is that is allows faster patient stabilization, with lesser invasiveness, and thus reduces the poor perfusion syndrome associated to TBADc.21 In our series, 6/8 cases of postoperative mesenteric ischemia were recorded in TBADc (11.1%), with a mortality rate of 16.7% in these patients.
In the case of thoracic trauma, in the same way as in TBADc and RTAA, the conventional treatment of thoracic damage always involved open repair and the placement of a stent. The mortality rate of OS in TTA has been very high (24%–42%), due to the fact that trauma implies lung contusion, solid organ damage, head injuries, the need for anticoagulation for surgery, etc. Because of this, there has been great interest in developing a less invasive technique for TTA, and TEVAR has been essential from the beginning in this respect — demonstrating a decrease in mortality rate to 9.7% (6.3% in our series).22,23 The GPC-ESVS recommends TEVAR in these patients as first treatment option (recommendation 29: class I, level of evidence C).
Analysis of elective TEVAR versus emergency TEVARHaving established the advantages of TEVAR versus OS in diseases of the descending thoracic aorta (DTA), important differences in outcome are observed according to whether the technique is performed on an emergency or elective basis. In our registry, the mortality rate with the endoprosthesis was 5.3% in the case of elective repair and 18.5% in emergency endovascular repair — though the difference was not statistically significant. There is information in our series that may explain these differences, such as the fact that the preoperative ASA score in the emergency cases was V in 42.9% of the cases, while only 2% of the elective cases presented this same score. It has also been established that an older age of the patients and a greater diameter of the thoracic aorta aneurysm (TAA) are predictors of greater mortality.24 Both of these circumstances concur in our emergency TEVAR group versus the elective group (Table 5).
In the case of the traumatisms in our series, 56.3% were of type III (pseudoaneurysms of the thoracic aorta) and 34.4% of type IV (complete transection). This is an indicator of the greater severity of the emergency cases. In elective TEVAR, these percentages were lower and the lesions were less severe (type I and type II). An extensive literature review25 including 139 studies and 7768 patients suggests that aortic repair in TTA should be postponed if there are other severe lesions that require stabilization — though if the aortic lesion is severe, repair should be carried out on an emergency basis (recommendation 27: class I, level of evidence C).15,26
Analysis of emergency TEVAR according to indicationComplicated acute type B aortic dissectionAmong the three emergency indications of DTA repair, TBADc involves the greatest postoperative complications. In our series it was associated to an increase incidence of postoperative CVA, paraplegia and the need for hemofiltration (9.3%, 9.3% and 18.5%, respectively) versus RTAA and TTA (Table 3). For this reason, it is important in these patients to analyze risk from the start, in order to determine whether the best option in each case is medical treatment, OS or TEVAR. Nevertheless, and despite the lack of randomized clinical trials, there is growing evidence that the emergency endovascular intervention affords greater benefit in TBADc than the other two options.12,20,27,28
Ruptured thoracic aortic aneurysmThe mortality rate in this subgroup was the highest at 27.9% (20.4% in TBADc and 6.3% in TTA), possibly because these patients were significantly older (mean age 71.11 ± 11.5 years) and with larger aortic diameters than in elective surgery. In our series, these patients had a greater incidence of infection (18.4%; mostly pulmonary infections secondary to lung contusion) and postoperative bleeding (11.6%) versus the rest of the groups. Due to the above, endovascular techniques have always been regarded as an attractive option in these high-risk patients. A recent review of the Cochrane Collaboration29 has attempted to demonstrate that TEVAR is a good alternative to OS in reducing this high morbidity–mortality, but was unable to do so because of the lack of randomized clinical trials; although the level of evidence is high, it comes mainly from non-randomized studies or case series. Nevertheless, three international clinical practice guides recommend TEVAR over OS in RTAA, provided the anatomical characteristics and comorbidities are appropriate.5,24,30
Traumatic thoracic aortic ruptureTraumatic thoracic aortic rupture is a potentially fatal surgical emergency that is most often caused by rapid acceleration/deceleration injuries in the context of a traffic accident and/or closed chest trauma. This implies that the treated patients are younger (mean age 45.5 ± 16.6 years in our series), that there are comparatively fewer complications than in the other two disease conditions (no CVA or coronary events, and no need for postoperative hemofiltration in our series), and that the 30-day mortality rate is lower (6.3% of the cases, versus 27.9% in RTAA). In traumatisms, TEVAR has had a spectacular introduction, and although there are no randomized clinical trials determining that this technique is associated to lesser morbidity–mortality,31 the severity of the situation, and the results of meta-analyses and long case series, have caused it to be the technique chosen by most surgeons.
Despite all the promise brought by the emergent endovascular technology, the limitations of TEVAR cannot be obviated. A first issue is the risk associated to management of the guides in the aortic arch, with the need to cover a large extension of the thoracic aorta or the LSA. This implies an increased risk of CVA and postoperative paraplegia (5.2% and 5.9% of the patients in our registry). Despite this high risk, however, multiple systematic reviews and meta-analyses have demonstrated lower postoperative neurological complication rates with TEVAR versus OS.32 The second concern is the high reintervention rate among patients subjected to TEVAR, with figures ranging between 7.6% and 9% at 30 days, versus 0% to 2.9% in OS (9% in our series). In many cases such risk could be related to the emergency situation, since the physicians would not have the opportunity to optimize the size of the prosthesis and the placement site, giving rise to anchoring or material failures over the long term.33 This may have a negative impact upon the quality of life of the patients treated with TEVAR. Lastly, a third concern is referred to the long-term outcomes of endovascular treatment. Further studies are needed, involving longer follow-up periods, to determine whether there are survival benefits with TEVAR over the long term versus OS. This would be important for the choice of treatment in younger patients with a longer life expectancy.
Although our study involves a large number of patients, they do not represent all the cases operated upon in Spain, and this could result in selection bias. We also must underscore that this is a retrospective multicenter study, with variability of the applied protocols. These limitations must be considered on drawing conclusions, though the lack of randomized clinical trials comparing this novel technique versus classical surgery implies that registries of case series such as our own are of great importance.
ConclusionsThe endovascular treatment of emergency conditions of the descending thoracic aorta has resulted in revolutionary changes in the perioperative management of these patients both at surgical level and in the Intensive Care Unit. This study represents the largest evaluation of patients with DTA disease treated on an emergency basis with TEVAR in Spain, and may offer the best evidence currently available regarding the treatment of this life-threatening type of disorder. The present study is the first to reflect real-life clinical practice in our setting at national level. Given the chronic nature of the disease, continuous monitoring is required after TEVAR, and additional improvements are needed in endoprosthesis design in order to reduce the complications related with the endoprosthesis and improve patient long-term survival.
Financial supportThis study has received no funding in the form of grants or external financial support. The registry was developed independently of the industry and was supported by the scientific interest of the Endovascular Surgery Chapter of the SEACV and its participants.
Authorship/collaboratorsAll the authors provided critical comments and actively contributed to the analysis and the investigation.
Author 1: Cristina López-Espada. Study conception and general management and planning. Data compilation and writing of the manuscript, with the contribution of all the authors.
Author 2: José Patricio Linares-Palomino. Conception and development of theory; design of the model and statistical analysis.
Author 3: José Manuel Domínguez-González. Data contribution and development of the theoretical setting.
Author 4: Elena Iborra-Ortega. Data contribution and supervision of the project.
Author 5: Pascual Lozano Vilardell. Data contribution and design of figures for comprehension of the text.
Author 6: Teresa Solanich-Valdaura. Data contribution and statistical analysis.
Author 7: Guido Volo-Pérez. Data contribution and assistance in supervising the project.
Author 8: Estrella Blanco-Cañibano. Data contribution and development of the theoretical setting.
Author 9: Andrés Álvarez-Salgado. Data contribution and checking of the statistical methodology.
Author 10: Juan Carlos Fernández-Fernández. Data contribution and assistance in designing the figures.
Author 11: Manuel Hernández-Rydings. Data contribution and assistance in supervising the project.
Author 12: Manuel Miralles-Hernández. Data contribution and assistance in designing and implementing the research.
Conflict of interestThe authors declare that they have no conflicts of interest.
Thanks are due to the Endovascular Surgery Chapter (CCEV) and the Spanish Society of Angiology and Vascular Surgery (SEACV) for their support of this project in promoting care improvement initiatives in our specialty.
Please cite this article as: López Espada C, Linares Palomino JP, Domínguez González JM, Iborra Ortega E, Lozano Vilardell P, Solanich Valldaura T, et al. Estudio multicéntrico de la reparación endovascular urgente de la aorta torácica: indicaciones y resultados. Med Intensiva. 2021;45:280–288.