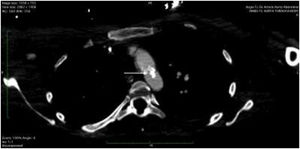
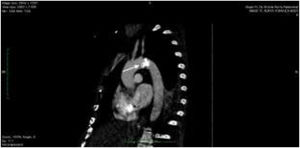
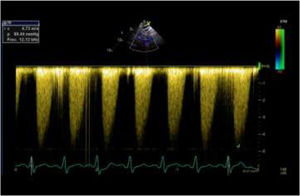
A 40-year-old woman with no relevant medical history was admitted to the ICU due to cardiogenic shock with severe systolic dysfunction and generalized hypocontractility evidenced by transthoracic echocardiography (TTE). Invasive monitoring was attempted using a thermodilution system, with great difficulty in securing ultrasound-guided access to both femoral arteries. A significant pressure gradient between the upper and lower extremities was observed. With a strong suspicion of aortic disease, a guided CT angiography study was requested, which revealed an extensive calcified atheroma plaque in the aortic arch (Fig. 1), with important obstruction in the sagittal plane reconstruction (Fig. 2). Repeat TTE was performed due to the strong suspicion of coarctation, recording a maximum systolic gradient in the descending thoracic aorta of 89 mmHg, which confirmed the disorder (Fig. 3). An endovascular approach was adopted to place a thoracic endoprosthesis supported by an intra-prosthetic steel stent. The subsequent course proved favorable, with a gradual return of ventricular function to normal levels, leaving a residual gradient of 32 mmHg.
Please cite this article as: Muñoz Garach M, Cruces Moreno MT, Moreno Romero O. Coartación aórtica adquirida: aorta en arrecife de coral. Med Intensiva. 2022;46:416–417.